When Professor Per-Ingvar Brånemark placed the first titanium root-form dental implant in 1965, only patients with adequate bone volume were considered candidates for implant rehabilitation. Patients with atrophy and alveolar deficiencies were restricted to prosthetic reconstruction with conventional prostheses. As dental implants became more popular and their indications for restoration became more diverse, the need to address alveolar deficiencies also grew. Technologic innovations in bone physiology, tissue banking, and surgical techniques have advanced the knowledge and understanding of the reconstruction of alveolar defects.
Since the infancy of dental implants in the late 1960s and 1970s, implant dentistry has grown to greater than a $700 million industry in the United States in 2008. It is estimated that the U.S. dental implant market will exceed $1 billion by the year 2013. The widespread acceptance and increased placement of implants have also led to a significant rise in concomitant reconstructive procedures, including hard and soft tissue grafting. Successful implant osseointegration, stability, and long-term survival require that the implant site have sufficient bone quality and quantity that will withstand loading and occlusal forces. When alveolar ridge deficiencies exist, reconstruction of the defect is required before or concurrent with implant placement. The contemporary oral and maxillofacial surgeon must not only be able to place implants but also possess the knowledge and surgical prowess to address alveolar deficiencies for comprehensive implant reconstruction. Reconstruction of alveolar defects encompasses replacement of hard and soft tissues that have been lost secondary to congenital anomalies, trauma, pathology, atrophy, or other causes. Autogenous grafts are the most widespread and predictable graft materials used for the reconstruction of alveolar defects.
Etiopathogenesis/Causative Factors
It was estimated that by the year 2010, 100 million Americans will be missing one or more teeth and that 36 million will be edentulous in one or both arches. As teeth are lost, the supporting periodontal structures and bone are also lost, and this creates alveolar defects. Alveolar resorption following tooth loss occurs in a predictable pattern, initially along the labial surface of the alveolar crest. This reduces alveolar width and, later, alveolar height. The majority of the bone loss, estimated to be 40% to 60%, occurs within the first 36 months following the loss of teeth, and the resorption pattern declines to 0.25% to 0.5% annually after the first 3 years. The resulting defects can be manifested as insufficient alveolar bone width, height, or a combination of both deficiencies. Alveolar defects can compromise implant support, function, and esthetics.
A variety of graft materials are available for restoring alveolar defects, including autologous, allogeneic, and xenogeneic grafts and alloplastic materials. When compared with bone substitutes, autogenous bone has more ideal biochemical properties and greater potential for integration with the surrounding tissues. Autogenous grafts are the gold standard by which other graft materials are compared. They are well documented and have been used extensively for reconstructing alveolar defects. Autogenous bone is a connective tissue that has the ability to heal and remodel by cellular regeneration and the production of a mineral matrix, as opposed to collagen deposition and scar formation. Bone cellular regeneration involves osteoprogenitor cells that have the ability to differentiate into bone-forming cell lineages: osteoblasts, osteocytes, and osteoclasts. It is this unique property of cellular regeneration that allows reconstructive surgeons to predictably perform bone grafting.
Autogenous grafts are superior to other graft materials because of their combined osteoconductive, osteoinductive, and osteogenic properties. Osteoconduction is the formation of new bone from adjacent bone or periosteum along a physical matrix. The matrix acts as a scaffold and allows deposition and new bone growth on its surface. With autogenous grafts, the cortical portion of the graft acts as a scaffold and is remodeled and replaced with new bone in a process known as creeping substitution. Osteoinduction describes a process whereby new bone is produced in an area where bone did not exist previously. Osteoinduction is the formation of bone by biochemical stimulation and transformation of undifferentiated pluripotent mesenchymal cells into bone-forming cells. Osteogenesis is the development and formation of new bone from osteoid produced by osteoblasts. Osteogenesis can be induced by osteoprogenitor cells from within the bony defect or by the transfer of live osteoprogenitor cells from the harvest site. The osteogenic property of autogenous grafts is one of the most important characteristics that separate autogenous grafts from all other graft materials. Autogenous grafts also have the advantage of invoking minimal immunologic reactions.
Advancements in gene technology by recombinant techniques have revealed the sequence of many growth factors and other proteins involved in the formation and remodeling of bone. Recombinant human proteins in the form of bone morphogenetic protein (rhBMP-2) have shown the ability to regenerate skeletal tissue and induce new bone formation. Because the growth factors are proteins, a carrier is required for their release at intervals, and the carrier must be degraded with minimal tissue reaction. Although rhBMP-2 has shown considerable promise, additional clinical trials are needed to address the delivery technology, accuracy in dosing, and conditions for stimulation of bone growth.
Patient Evaluation/Diagnostic Studies
Preoperative evaluation consists of a thorough medical and dental examination ( Box 18-1 ). A systems review is performed and all medications noted. The social history is reviewed, including inquiries about tobacco use. Smoking has been implicated in increased failure rates in bone grafting and implants. The dental examination evaluates occlusion, teeth adjacent to the defect, periodontal status, and gingival architecture. The quantity of keratinized tissue and the thickness of the mucosa are assessed. Thin periodontal biotypes have a higher incidence of recession than do thick biotypes. The endodontic status of teeth adjacent to the recipient site is also evaluated.
- •
Medical evaluation
- •
Dental examination
- •
Radiographic examination: Panorex, periapicals, lateral cephalogram, computed tomography (if available)
- •
Facial and intraoral photographs
- •
Mounted models: diagnostic wax-up
- •
Conference with the restorative dentist or prosthodontist
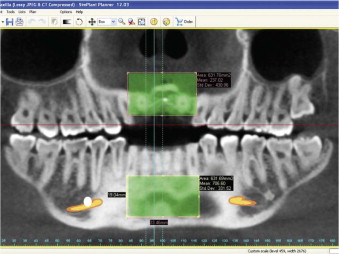
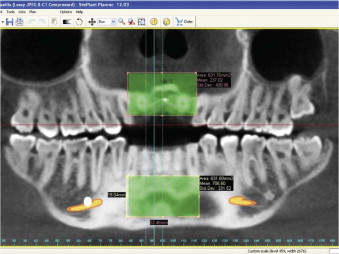
The radiographic examination consists of plain films to visualize the alveolar defect and potential donor sites. The films are also used to evaluate the surrounding anatomy, including the tooth roots, maxillary sinus, mental foramen, and inferior alveolar neurovascular bundle. Computed tomography (CT) provides three-dimensional visualization of the alveolar defect and potential donor sites ( Fig. 18-1 ). The images have minimal distortion with superior accuracy of the related anatomy. CT scans provide unsurpassed volumetric analysis of alveolar defects in comparison to plain films. Multiple computer-based software programs are available to analyze the CT scans and aid in planning treatment for implants and bone graft requirements. Stereolithic models can be generated from the CT scan to provide replicas of the craniofacial skeleton. Hounsfield units obtained from the CT scan provide a measure of the bone density at the alveolar defect and donor site.
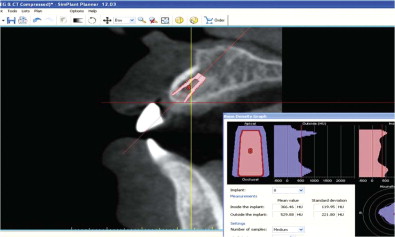
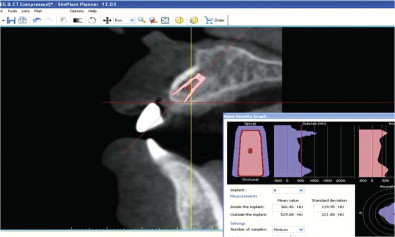
Facial and intraoral photographs provide valuable information about esthetics, facial contours, and symmetry. The soft tissues can also be evaluated at rest and with animation. Photographs provide a permanent record of the pretreatment conditions that can be compared with the final treatment results. Mounted models provide ridge form and interocclusal relationships between arches. Diagnostic waxing allows visualization of the planned prosthetic outcome. Visualizing the proposed tooth position helps in determining ideal implant placement and graft requirements. The wax-up can also be used as a radiographic template for the CT scan and as a surgical guide for placement of the implant ( Fig. 18-2 ).
After the aforementioned examinations have been performed and the diagnostic data have been compiled and analyzed, a treatment plan can be formulated. Treatment planning incorporates the restorative dentist or prosthodontist and the surgeon. The treatment plan addresses the patient’s chief complaint, restorative goals, and any hard or soft tissue deficiencies. The decision to perform bone grafting is driven by the requirements for the prosthesis.
Patient Evaluation/Diagnostic Studies
Preoperative evaluation consists of a thorough medical and dental examination ( Box 18-1 ). A systems review is performed and all medications noted. The social history is reviewed, including inquiries about tobacco use. Smoking has been implicated in increased failure rates in bone grafting and implants. The dental examination evaluates occlusion, teeth adjacent to the defect, periodontal status, and gingival architecture. The quantity of keratinized tissue and the thickness of the mucosa are assessed. Thin periodontal biotypes have a higher incidence of recession than do thick biotypes. The endodontic status of teeth adjacent to the recipient site is also evaluated.
- •
Medical evaluation
- •
Dental examination
- •
Radiographic examination: Panorex, periapicals, lateral cephalogram, computed tomography (if available)
- •
Facial and intraoral photographs
- •
Mounted models: diagnostic wax-up
- •
Conference with the restorative dentist or prosthodontist
The radiographic examination consists of plain films to visualize the alveolar defect and potential donor sites. The films are also used to evaluate the surrounding anatomy, including the tooth roots, maxillary sinus, mental foramen, and inferior alveolar neurovascular bundle. Computed tomography (CT) provides three-dimensional visualization of the alveolar defect and potential donor sites ( Fig. 18-1 ). The images have minimal distortion with superior accuracy of the related anatomy. CT scans provide unsurpassed volumetric analysis of alveolar defects in comparison to plain films. Multiple computer-based software programs are available to analyze the CT scans and aid in planning treatment for implants and bone graft requirements. Stereolithic models can be generated from the CT scan to provide replicas of the craniofacial skeleton. Hounsfield units obtained from the CT scan provide a measure of the bone density at the alveolar defect and donor site.
Facial and intraoral photographs provide valuable information about esthetics, facial contours, and symmetry. The soft tissues can also be evaluated at rest and with animation. Photographs provide a permanent record of the pretreatment conditions that can be compared with the final treatment results. Mounted models provide ridge form and interocclusal relationships between arches. Diagnostic waxing allows visualization of the planned prosthetic outcome. Visualizing the proposed tooth position helps in determining ideal implant placement and graft requirements. The wax-up can also be used as a radiographic template for the CT scan and as a surgical guide for placement of the implant ( Fig. 18-2 ).
After the aforementioned examinations have been performed and the diagnostic data have been compiled and analyzed, a treatment plan can be formulated. Treatment planning incorporates the restorative dentist or prosthodontist and the surgeon. The treatment plan addresses the patient’s chief complaint, restorative goals, and any hard or soft tissue deficiencies. The decision to perform bone grafting is driven by the requirements for the prosthesis.
Treatment/Reconstructive Goals
The widespread use of autogenous grafts to reconstruct defects in the maxillofacial region clearly separates oral and maxillofacial surgeons from the other specialties that treat the maxillofacial region. Each alveolar defect is unique and involves specific hard and soft tissue requirements for reconstruction. One of the goals of reconstructing alveolar defects is restoration of alveolar ridge bone height and width to adjacent bone levels. Other reconstruction goals include restoration of osseous bulk to provide strength and soft tissue profile for the implant restoration. Osseous bulk also provides support for facial tissues, including lip support, which can improve facial esthetics. Restoration of the continuity of the maxillary and mandibular arch form is another reconstructive goal because this optimizes the maxillofacial musculature complex. Reconstruction of alveolar defects is imperative to provide support for implants and, ultimately, a functioning prosthesis under loading and occlusal forces.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


