This article reviews the diagnostic process, from the first clinically evident stages of the caries process to development of pulpal pathosis. The caries diagnostic process includes 4 interconnected components–staging caries lesion severity, assessing caries lesion activity, and risk assessments at the patient and tooth surface level – which modify treatment decisions for the patient. Pulpal pathosis is diagnosed as reversible pulpitis, irreversible pulpitis (asymptomatic), irreversible pulpitis (symptomatic), and pulp necrosis. Periapical disease is diagnosed as symptomatic apical periodontitis, asymptomatic apical periodontitis, acute apical abscess, and chronic apical abscess. Ultimately, the goal of any diagnosis should be to achieve better treatment decisions and health outcomes for the patient.
Modern management of dental caries
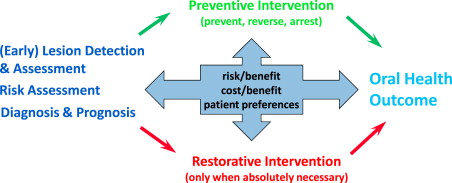
The current practice of dentistry remains weighted toward surgically treating the consequences of dental caries. The importance of accurately diagnosing dental caries has in the past been overshadowed by the need to restore the extensive damage to tooth structure. With the advent of widespread use of fluoride in developed countries, the prevalence, severity, and rate of caries progression have declined. Consequently, practitioners can adopt a more conservative approach and apply the principles of modern management of dental caries. These involve detecting and assessing caries lesions at an earlier stage; determining the caries risk status of the patient; making a diagnosis if disease is actually present; establishing a prognosis; applying intervention strategies focused on preventing, arresting, and possibly reversing the carious process; and delaying restorative treatment until absolutely necessary ( Fig. 1 ). Most studies have evaluated these aspects of caries management as independent processes rather than one system that impacts the long-term health of patients. Ultimately, the usefulness of a diagnosis has to be judged by whether it leads to better treatment decisions and health outcomes for the patient, and thus, other factors, such as the risk/benefit and cost/benefit to the patient as well as patient preferences, need to be considered (see Fig. 1 ).
Challenges of Caries Diagnosis
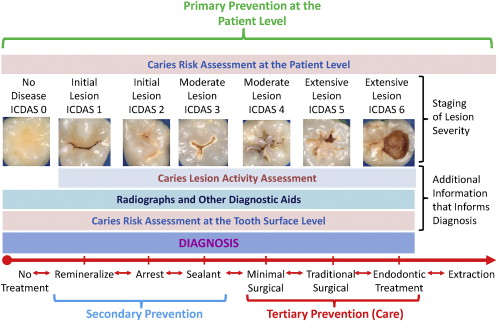
Unlike many medical diseases, the diagnosis of the early stages of dental caries is not informed by the patient’s symptoms, and there is almost complete reliance on the clinical presentation (signs) of the disease. As the disease advances, there can be symptoms of pain and sensitivity to hot, cold, and sweet substances. In its later stages, there can be severe debilitating pain requiring endodontic therapy or tooth extraction. The detection of the signs and symptoms of dental caries is a component of and actually distinct from the caries diagnostic process, which leads directly to treatment decisions. The caries diagnostic process must also include risk assessment at the patient and the tooth surface level and caries lesion activity assessment ( Fig. 2 ). A degree of uncertainty exists when diagnosing the initial (noncavitated) caries lesions, because these early lesions may be active (progressing), inactive (arrested), or regressing (remineralizing). Therefore, a very important aspect of caries diagnosis is assessing the caries activity status of the actual caries lesion. However, making an accurate clinical determination of caries lesion activity status is as challenging as it is important, and new technology-based methods to aid this assessment are needed.
For several reasons, proportionally very little of a dentist’s time is spent on the diagnostic process compared with physicians: (1) Reimbursement mechanisms in the United States reward operative and restorative treatment, whereas accurate diagnosis and disease prevention are not given high priority. (2) The diagnostic tools/procedures and codes for reimbursement are limited compared with medicine. (3) Dental schools spend a substantial portion of curricular time on training to meet the technical demands of the practice of dentistry and proportionally very little on how to accurately diagnosis dental caries and manage it as a disease process, which leads to a continuing exacerbation of the problem.
Dentists vary widely when diagnosing dental caries, with agreement using traditional techniques ranging from poor to moderate (kappa values 0.30 to 0.60). The consequences of misdiagnosis are inadequate treatment or overtreatment. Underdiagnosis leading to inadequate treatment can result in additional destruction of tooth tissue, pulpitis, toothaches, and tooth loss. However, dental caries is generally not an acute disease process but a chronic one that takes many years to progress in the postfluoride era. Overdiagnosis can lead to an unnecessary cascade of costly restorative treatment. Based on data from the dental insurance industry, to maintain a single molar restoration placed in a 10-year-old patient reaches $2197 by age 79 years. In many clinical situations, there is uncertainty about the diagnosis of caries. The paradigm in clinical practice and teaching needs to shift to surgical intervention being the last rather than first course of treatment considered by the dentist.
Role of Caries Risk Assessment and Caries Lesion Activity Assessment in the Diagnostic Process
As mentioned earlier, the caries diagnostic process includes 3 interactive components, namely, carious lesion detection, lesion activity assessment, and caries risk assessment, each informing the rest and all essential to making the best possible treatment decisions. Risk assessment of the patient and the tooth surface can help inform caries lesion detection and activity assessment as well as treatment decisions (see Fig. 2 ). Furthermore, caries lesion detection and activity assessment should help inform caries risk assessment, in that patients with detectable caries active lesions are at a minimum at moderate caries risk for future caries. Patients without clinically detectable caries active lesions may also be at moderate or high risk depending on recent changes in their risk factors/indicators.
Ideally, the goals are to identify patients at risk of developing caries before the disease process progresses to the point of expressing clinically and to use more aggressive primary preventive measures (professionally applied fluoride, preventive use of dental sealants). However, currently available caries risk assessment tools do not have sufficient accuracy to identify patients who eventually develop caries. Based on available evidence, the best predictor of future caries remains past caries experience. This suggests that in addition to recommending primary prevention measures (oral hygiene instructions, dietary advice, and recommending twice-daily fluoride dentifrice use) for all patients (see Fig. 2 ), dental professionals need to be vigilant during routine examinations to carefully detect dental caries at the earliest stages of the disease when secondary preventive measures (professionally applied fluoride, therapeutic use of sealants) are still possible and before surgical intervention is the only choice.
Incorporation of Caries Diagnosis into Patient Caries Management
Ultimately, the value of an accurate diagnosis is that it leads to the best possible treatment decisions and short- and long-term health outcomes. By combining the clinical presentation, including the severity of carious lesions and caries lesion activity assessment, with identifying caries risk factors of the patient and the tooth surface, a caries diagnosis can be made leading to the most appropriate treatment decision (see Fig. 2 ). This diagram is not intended to be prescriptive in recommending a particular level of intervention for each level of caries severity. The arrows pointing in both directions indicate that there is a treatment decision continuum that can be modified by risk factors of the individual patient and tooth surface, lesion activity status, and patient preferences.
Importance of Early Diagnosis of Pupal Pathosis
As the caries process progresses without some type of intervention, the pulp ultimately becomes involved. Being able to distinguish reversible pulpal symptoms resulting from caries from irreversible ones is paramount to deciding on the appropriate treatment. Knowing the early warning signs of pulpal and periapical disease certainly helps the practitioner decide on the most conservative treatment approach. The dental pulp is a resilient organ, and frequently, by removing the causative agent (caries), the pulp has the capacity to heal if there is no irreversible damage. By being alert to the clinical signs and symptoms associated with reversible and irreversible pulpal changes caused by caries, the practitioner can decide on the most appropriate treatment modality that potentially preserves the patient’s natural dentition for a lifetime.
Diagnosing dental caries
Dental caries is a dynamic disease process in which early lesions undergo many cycles of de- and remineralization before being expressed clinically. Its dynamic nature causes uncertainty about whether it is progressing, regressing, or in a state of equilibrium at any given point in time. Once expressed clinically, caries can be detected by several detection methods, conventional (visual, radiographic) or newer technology-based ( Table 1 ).
| Sound (No Disease) | Subclincial Caries | First Clinical Signs of Caries (Initial) | Established Caries (Moderate) | Severe Caries (Extensive) | |
|---|---|---|---|---|---|
| ICDAS Codes | 0 | 0 | 1 + 2 | 3 + 4 | 5 + 6 |
| X-ray | Not detectable | Detectable on proximal surfaces | Detectable | Detectable | |
| Light-Induced Fluorescence , a | Some false positives | Detectable | Detectable | Detectable | Not useful |
| Infrared Fluorescence , b | Not detectable | May detect some lesions on occlusal and smooth surfaces | Detectable | Detectable | |
| Infrared Fluorescence Combined with Photothermal Radiometry , c | Possibly detectable | Detectable | Detectable | Detectable | |
| Transillumination , d | Not detectable | Detectable on approximal surfaces and, in some lesions, occlusal surfaces | Detectable | Detectable | |
| AC Impedance Spectroscopy , e | Not detectable | Detectable | Detectable | Detectable |
a Only Occlusal and smooth surfaces, limited data on root caries, caries around restorations and deciduous teeth.
b Occlusal, smooth, and proximal surfaces; limited data on deciduous teeth, root caries, and secondary caries.
c All surfaces, however, very limited data available only in vitro for occlusal surfaces, root caries, and smooth surfaces.
d Approximal and occlusal surfaces; very limited data available for secondary caries or deciduous teeth.
Current approaches used in dental practice and still taught in most dental schools are inadequate for detecting and diagnosing dental caries at an early reversible/arrestable stage, and a new system to support the modern treatment paradigm is needed. One system that is gaining traction is the International Caries Detection and Assessment System (ICDAS), which is based on visual criteria. ICDAS was developed as a standardized evidence-based system to assess severity stages of dental caries. It consists of 7 categories (0–6) to assess every tooth surface (see Table 1 ). The application of this new system requires a major change in approach toward the clinical oral examination of the dentition. A quick look in the oral cavity for the purpose of detecting teeth requiring operative treatment is not adequate to properly manage the carious disease process. The correct application of ICDAS requires that all surfaces of each tooth are free of plaque and carefully examined under wet and dry conditions. ICDAS has been shown to have good validity and reproducibility in several studies. Fig. 2 provides a summary of how ICDAS can be incorporated as part of a caries management system in which risk assessment of the patient, caries lesion severity and activity assessment, and caries risk assessment of the tooth are used to establish the diagnosis and determine the most appropriate treatment.
Initial Lesion
The initial signs of dental caries involve surface softening, which cannot be detected by conventional visual or radiographic methods but could potentially be picked up by some technology-based methods, such as quantitative light-induced fluorescence (QLF), which has been reported to detect lesions as early as 35 μm deep. Because the chemical composition of the carbonated hydroxyapatite is not uniform throughout the enamel, these variations result in varying enamel solubility. Thus, the caries process starts in the most acid-soluble sites on the tooth surface, leading to small defects (increased porosity) allowing biofilm acids to diffuse below the surface and demineralize the more soluble subsurface tooth structure.
At the individual patient level, even teeth with ICDAS score 0 may be in need of primary preventive intervention (topical fluoride, preventive use of sealants) if caries risk factors/indicators suggest the patient is at risk of future disease. The first visual sign of dental caries as described by ICDAS is ICDAS score 1. These lesions are observed visually only after the enamel surface is dried for a few seconds. At this stage, histologically the early enamel lesions are limited to the outer enamel layer. These lesions first appear as white spots and are sometimes called incipient lesions, white spot lesions, or even demineralization or decalcification areas. The lesion forms a conical shape, with the tip of the cone facing the enamel surface and the base facing the dentin. Enamel lesions tend to progress in the direction of the enamel prisms; thus, the format of the lesion changes according to its location. There is dissolution of the outermost surface of the enamel. The acid can attack the enamel rods or in between the enamel rods, causing an enlargement of intercrystalline diffusion pathways. Carbonate and magnesium are first solubilized, followed by calcium and phosphorus solubilization and dissolution of developmental irregularities.
The 4 distinct stages of porosity in carious enamel lesions are associated with the 4 zones of the early enamel lesion: the surface zone, body of the lesion, dark zone, and primary translucent zone. The surface zone is relatively intact, with a 1% pore volume (compared with 0.1% of sound enamel). The body of the lesion, triangular in shape, has a 5% to 25% pore volume. The dark zone pore volume is 2% to 4%, and the translucent zone, present in 50% of the lesions, has a pore volume of 1% to 4%. The porosity of these early lesions is filled with water, and therefore, when the surface is wet, the difference in the refractive indices of water and air is not seen. However, when the surface is dried, water is replaced by air and the lesion is revealed. The difference in diffraction coefficients of air and water, a physical phenomenon, results in the observed white color. At this stage, the demineralization has not reached the dentin; however, in some instances, a reaction to the injury can be observed by the deposition of minerals in the dentinal tubules, referred to as tubular sclerosis. Tubular sclerosis can be observed even before the bacterial invasion occurs into dentin and is not the lesion spreading laterally. This is stimulated by the presence of the biofilm as a defense mechanism from the pulp-dentin complex.
As the lesions further advance in the enamel, changes can be observed through the whole thickness of the enamel and sometimes affect the outer surface of the dentin (ICDAS 2). Optically and chemically, the changes observed in these lesions are the same as those seen in early enamel lesions. However, the changes are more pronounced and can be seen with the naked eye, even when saliva is coating the enamel surface. Histologically, this can be observed as complete dissolution of the thin perikymata overlapping areas corresponding to developmental irregularities (Tomes’ processes, pits, and focal holes), and there is greater enlargement of the intercrystalline spaces. At this stage, the increased permeability of enamel to acid and various other chemical stimuli leads the dentin-pulp complex to respond by increasing the activity of odontoblasts, which are stimulated to form a tertiary dentin matrix (reactionary dentin). The result may be retraction of their processes and an increase in collagen deposition in the periodontoblastic process space. In advanced enamel/early dentin lesions, color change is seen as a brown tint in the underlying dentin.
Moderate Lesion
When the lesions progress to the point of breaks occurring in the continuity of the enamel surface, forming microcavitations, they are referred to as ICDAS 3. This is a critical stage in the caries process, because once cavitation occurs, bacteria can easily invade the dentin, quickening the process without allowing time for dentinal reaction to occur. Nonsurgical treatment of this stage of caries is still possible, and sealants should be considered as a treatment option depending on individual patient factors (see Fig. 2 ).
In more advanced lesions (ICDAS 4), the lesion spreads along the dentino-enamel junction (DEJ) while destroying the mantle dentin. As the dentin is demineralized, it provides less support for the overlying enamel. These lesions may be non-or microcavitated. The enamel has the same characteristics as in the advanced enamel lesions.
Extensive Lesion
As the lesion advances, bacteria invade the DEJ leading to an enlargement of the gap between enamel and dentin. The lesion become cavitated, when the enamel surface collapses, exposing the dentin (ICDAS 5 and 6). This cavitation fills with food debris and saliva. The area where the bacteria are in direct contact with the dentin forms a leatherlike demineralized zone. The rate of carious lesion progression is reflected in the appearance of the peritubular zone, which is very thin or missing if the lesion progresses quickly. However, if the lesion expands slowly, sclerotic tubules form at the base of the lesion. The sclerotic tubules contain reprecipitated nonapatitic calcium phosphate. Bacterial acids demineralize the dentin and expose the extracellular matrix, which is subsequently degraded by matrix metalloproteinases found in the saliva and the dentin itself. At this stage, the enamel surrounding the dentin has the characteristics of an advanced enamel lesion. Advanced lesions become darker brown or even black as they advance in severity.
Radiography
Radiography has been the primary detection method of established proximal caries. As the carious process proceeds, the mineral content of enamel and dentin decreases, which decreases the attenuation of the x-ray beam as it passes through the tooth; a lesion is then detected by an increase in radiolucency. To detect proximal lesions, the x-ray beam must go through normal tissue before it passes through the lesion and out through normal tissue again. Therefore, at least one-third to one-half of the hard tissue must be affected by the caries process for the lesion to be detected radiographically. Dental radiographs are useful in detecting larger, more advanced, and possibly cavitated lesions (ICDAS scores 2–6 on proximal surface and ICDAS scores 4–6 on occlusal surfaces, although some ICDAS scores 2–3 are detectable). However, because of the limited image resolution and poor contrast of early carious lesions, radiographs are insensitive in detecting early-stage dental decay. New imaging technologies and more sensitive techniques are required in the early detection of such lesions.
Newer Technology-Based Caries Detection Methods
A wide range of technology-based methods can detect dental caries, and their use is recommended as diagnostic adjuncts. These methods are more useful in the early and moderate stages of the dental carious process (ICDAS 1–4), because with increasing severity of the lesion, the visual signs become more apparent and thus reduce the need for additional tools. Although, in the authors’ knowledge, no technology available can determine the activity status of the lesions in one visit, these tools can aid visual detection, diagnosis, and risk assessment. Several methods are currently marketed in the United States for caries detection, most being based on optical properties (Midwest Caries I.D., DENTSPLY Professional, Des Plaines, IL, USA; Microlux Transilluminator, AdDent Inc., Danbury, CT, USA), including fluorescence properties (DIAGNODent, KaVo, Charlotte, NC, USA; FluoreCam, Daraza, Noblesville, IN, USA; Inspektor Pro, InspeKtor Dental Care, Amsterdam, The Netherlands; Spectra Caries Detection Aid, Air Techniques Inc., Melville, NY, USA; The Canary System, Quantum Dental Technology, Toronto, Canada) and alternating current impedance spectroscopy (CariesScan PRO, CariesScan Ltd, Dundee, UK). Several reviews of these methods address principles and performance.
Basically, demineralization of dental enamel causes scattering of light photons leading to optical disruption, which can then be measured by detecting reflectance (Midwest Caries I.D.), a combination of luminescence and heat (The Canary System), differences in light transmission (Microlux), or impedance (CariesScan, PRO). Fluorescence systems are based on the difference in fluorescence observed between sound and demineralized enamel, which is greater when the enamel is illuminated by light in the blue-green range (488 nm).
In summary, fluorescence-based systems using light in the blue range (488 nm) have been reported to detect very early lesions, smaller than visual examination is able to detect, and a greater percentage of noncavitated lesions than visual examination can detect. This system has been investigated for its use on smooth and occlusal surfaces as well as for caries around restorations and root caries. The lesions detected with these fluorescence methods range from ICDAS scores 1 to 4, sensitivity being higher than other methods at the lower end of the spectrum (ICDAS 1–2); however, this is at the expense of specificity (thus a high number of false positives). The vast majority of the data published use the QLF Inspektor Pro software for analyses of the images, and it is not clear if the other systems have the same performance when different software is used for image analysis. However, because of the concerns regarding the noise caused by subclinical lesions that can be detected by QLF, there are reports combining the methodology with a clinical method without using the analyses aspect of the system. Methods based on fluorescence at the infrared range (655 nm wavelength; DIAGNODent) have greater sensitivity for lesions deeper into enamel and dentin (ICDAS 2–4). For caries around restorations, this can lead to many false positives. The recently introduced Midwest Caries I.D. and the Canary System also use the near infrared laser light. The Midwest Caries I.D. is based on detecting changes in reflectance from sound enamel to demineralized enamel. Two published abstracts indicate that this system was able to detect lesions at D3 level (caries in enamel and dentin) and performed better for detection of occlusal caries than proximal caries. On root caries, the system had sensitivities of 0.73 to 0.86 but did not perform better than ICDAS examinations. The Canary System is based on analyses of luminescence and thermal behavior of the emitted infrared photons (noncontacting frequency-domain photothermal radiometry and frequency-domain luminescence). Published data indicate that the sensitivity at the D2 threshold (caries in enamel only) is 0.81, whereas specificity is 0.87 for occlusal caries.
Transillumination methods (ie, Microlux) have at least the same sensitivity and specificity as bite-wing x-rays for detecting approximal and occlusal caries, achieving better performance for lesions into dentin. Impedance (CariesScan PRO) is able to detect lesions on approximal and occlusal surfaces, but limited data are available.
Diagnosing dental caries
Dental caries is a dynamic disease process in which early lesions undergo many cycles of de- and remineralization before being expressed clinically. Its dynamic nature causes uncertainty about whether it is progressing, regressing, or in a state of equilibrium at any given point in time. Once expressed clinically, caries can be detected by several detection methods, conventional (visual, radiographic) or newer technology-based ( Table 1 ).
| Sound (No Disease) | Subclincial Caries | First Clinical Signs of Caries (Initial) | Established Caries (Moderate) | Severe Caries (Extensive) | |
|---|---|---|---|---|---|
| ICDAS Codes | 0 | 0 | 1 + 2 | 3 + 4 | 5 + 6 |
| X-ray | Not detectable | Detectable on proximal surfaces | Detectable | Detectable | |
| Light-Induced Fluorescence , a | Some false positives | Detectable | Detectable | Detectable | Not useful |
| Infrared Fluorescence , b | Not detectable | May detect some lesions on occlusal and smooth surfaces | Detectable | Detectable | |
| Infrared Fluorescence Combined with Photothermal Radiometry , c | Possibly detectable | Detectable | Detectable | Detectable | |
| Transillumination , d | Not detectable | Detectable on approximal surfaces and, in some lesions, occlusal surfaces | Detectable | Detectable | |
| AC Impedance Spectroscopy , e | Not detectable | Detectable | Detectable | Detectable |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


