Figure 4.33 Intraoral photographs of patient showing intercuspal position (a), tooth contacts during right (b) and left (c) lateral excursion as well as maxillary (d) and mandibular (e) occlusal surfaces. Severe wear is noted.
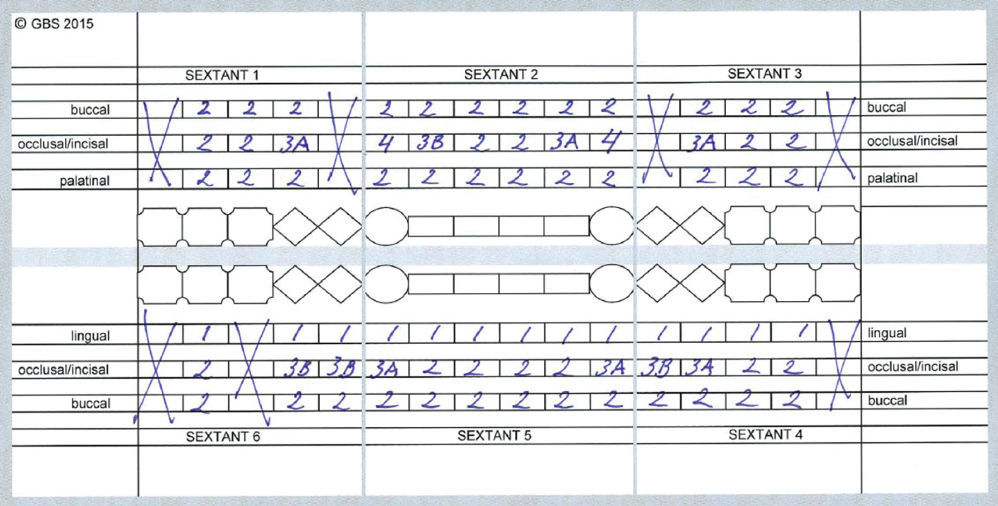
Figure 4.34 Completed chart of tooth wear from clinical examination.
Occlusion
- There was a normal occlusion (Angle class I, both frontal and posterior). Concerning the articulation patterns, the right (Figure 4.33b) and left (Figure 4.33c) lateral movements showed group guidance; in protrusion, frontal guidance existed.
Saliva
- Evaluation of the salivary parameters, like the salivary flow, buffer capacity, and pH, revealed normal values.
H. Additional Examination and Findings
- Panoramic imaging showed three endodontically treated teeth and periapical radiolucent areas for 36 and 46 (Figure 4.35).
- Additional questionnaires regarding oral hygiene products, food diary, reflux, xerostomia. These showed an acidic diet, use of hard toothbrush in combination with abrasive toothpaste, possible reflux, but no xerostomia.
- Patient was referred to a gastroenterologist.

Figure 4.35 Panoramic radiograph.
I. Diagnosis/Diagnoses
Other
- Tooth wear.
- Probable bruxism.
- Asymptomatic apical periodontitis.
J. Case Assessment
- The findings from the tooth wear evaluation system (TWES), Tables 4.5 4.6, 4.7, and 4.8, were in line with the oral history taking and the answers to the questionnaires (OBCL, oral hygiene products, food diary, xerostomia).
Table 4.5 TWES: module “Qualification”
Clinical signs of erosion 1. Occlusal “cupping,” incisal “grooving,” “cratering,”a rounding of cusps and groovesb 2. Wear on non-occluding surfacesa 3. “Raised” restorationsa,b 4. Broad concavities within smooth surface enamel,a convex areas flatten, or concavities become present, width exceeds depthb 5. Increased incisal translucencya 6. Clean, nontarnished appearance of amalgamsa 7. Preservation of enamel “cuff” in gingival crevicea,b 8. No plaque, discoloration, or tartarb 9. Hypersensitivitya 10. Smooth silky-shining, silky-glazed appearance, sometimes dull surfaceb Clinical signs of attrition 1. Shiny facets,a flat and glossyb 2. Enamel and dentin wear at the same ratea 3. Matching wear on occluding surfaces,a corresponding features at the antagonistic teethb 4. Possible fracture of cusps or restorationsa 5. Impressions in cheek, tongue, and/or lip Clinical signs of abrasion 1. Usually located at cervical areas of teetha 2. Lesions are more wide than deepa 3. Premolars and cuspids are commonly affecteda a According to Gandara and Truelove (1999).
b According to Ganss and Lussi (2014).
Table 4.6 TWES: overview of modules
- Diagnostic modules
- Basis diagnostic (general practitioner)
- Module Qualification
- Module Quantification, screening module or
- Module Quantification, clinical crown length module Recording of tooth wear (intraoral photographs, dental casts)
- Extended diagnostic (referral clinic)
- Module Quantification, finer-grained occlusal/incisal and non-occlusal/non-incisal
- Module Oral history, questionnaires
- Module Salivary analysis
- Treatment/management modules
- Module Complaints of the patient versus reasons for the clinician to start treatment/management
- Module Start of treatment/management
- Module Level of difficulty
Table 4.7 TWES: module “Quantification”
Eight-point ordinal scale for occlusal and incisal grading For each tooth the grade is determined 0 = no (visible) wear 1a = (within the enamel) minimal wear of cusps or incisal tips 1b = (within the enamel) facets parallel to the normal planes of contour 1c = (within the enamel) noticeable flattening of cusps or incisal edges 2 = wear with dentin exposure and loss of clinical crown height ≤1/3 3a = wear with dentin exposure and loss of clinical crown height 1/3–1/2 3b = wear with dentin exposure and loss of clinical crown height 1/2–2/3 4 = wear with dentin exposure and loss of clinical crown height of ≥2/3 Three-point ordinal scale for non-occlusal/non-incisal grading For each tooth the grade is determined, both buccal/labial as palatinal/lingual 0 = no (visible) wear 1 = wear confined to the enamel 2 = wear into the dentin Source: Wetselaar et al. (2009).
- Both the oral history taking and the questionnaires revealed that awake and sleep bruxism were present. The intraoral findings of the soft tissues also supported bruxism. Based on this information, and the clinical examination, a diagnosis of probable bruxism was made (Lobbezoo et al., 2013).
- Concerning the dental hard tissues, it was found that, beside chemical tooth wear, mechanical tooth wear was also present. For the diagnosis of bruxism, the clinical findings: “enamel and dentin wear at the same rate” and “matching wear on occluding surfaces or corresponding features at the antagonistic teeth” were present. This can be the reason for the clinical signs of attrition (see earlier).
- Knowledge about the use of oral hygiene products of the patients is important, because these products can be abrasive. The patient is using an abrasive dentifrice and a hard toothbrush; this can be part of the reason for the clinical signs of abrasion (see earlier).
- The food diary revealed an acidic diet; this can be the reason for the clinical signs of erosion (see earlier). The reflux questionnaire revealed that the patient sometimes experienced complaints that could fit with gastroesophageal reflux disease, like heartburn and regurgitation. This also can be the reason for the clinical signs of erosion (see earlier), especially the clinical finding “preservation of enamel cuff in gingival crevice.” Also, during the oral history taking, the patient reported that sometimes he suffers from heartburn and regurgitation.
- The module “Quantification” of the TWES (Table 4.7) showed that the patient could be classified as having both localized extreme (sextant 2) and generalized severe (sextants 1, 3, 4, 5, and 6) tooth wear. Concerning the origin of the tooth wear, this case was classified as tooth wear with a mixed origin: mechanical/intrinsic (attrition), mechanical/extrinsic (abrasion), chemical/intrinsic (erosion), and chemical/extrinsic (erosion). The origin was based on the qualification, the oral history taking, and some questionnaires.
Table 4.8 TWES: module “Start of treatment/management”
| Primary criterion | Treatment/management | Secondary criterion |
|
|
|
K. Evidence-based Treatment Plan including Aims
- The first aim was to eliminate infections in 36 and 46.
- Teeth 36 and 46 were surgically removed.
- The second aim was to determine if the patient had any gastrointestinal condition that could be part of the etiology of the tooth wear. The patient was therefore referred to a gastroenterologist, who diagnosed gastroesophageal reflux disease. Medication with a proton pump inhibitor was prescribed.
- The third aim was to prevent pain/sensitivity, restore esthetics, and prevent further loss of hard dental tissues and breaking of restorations. Restorative treatment was started according to a so-called dynamic treatment plan. This means to start only with the necessary steps, and if possible use reversible techniques. All existing restorations were removed before restoring all teeth with direct composite restorations.
L. Prognosis and Discussion
- There is evidence that a restorative treatment plan with direct composite material has a good prognosis (Milosevic and Burnside, 2015). The biggest advantage of this kind of treatment is to avoid further loss of dental hard tissues by using a nonpreparation or minimal invasive restoration technique. When doing so, the dental clinician can monitor the patient and see if other diagnostic steps or treatments are necessary. Common complications are wear or breaking of the restorations. To avoid these complications, a protective stabilization splint can be made. In this case this was not done, because it was thought that the chemical wear was of greater importance than the mechanical wear. Although the patient used medication for the gastroesophageal reflux disease, it is nevertheless known that (a part of) the reflux can remain. If so, the splint may retain gastric acidic content that may cause an adverse effect.
- When using indirect techniques, preparation of the teeth is necessary; more dental tissue is sacrificed. There is a higher risk for endodontic treatment, and, for example, when bruxism exists, a higher risk of breaking of these indirect restoration, and even worse of the roots themselves. If that were the case, more teeth would have been lost. Making three-unit-bridges to close the existing diastema is a possibility; in this case no improvement in esthetics or masticatory function will be achieved; again, a greater risk of these roots should be the case. Placement of dental implants on the location of teeth 36 and 46 is a better option than the three-unit- bridges. There is no higher risk for complications of the adjacent teeth, but again no gain in esthetics or masticatory function will be achieved.
Background Information
Qualification (intraoral examination)
- Tooth wear is a multifactorial condition, leading to the loss of dental hard tissues; namely, enamel and dentin.
Three subtypes of tooth wear can be present: erosion, attrition, and abrasion. The following signs of erosion (chemical wear) may occur: occlusal cupping, cratering, rounding of cusps, wear on non-occluding surfaces, raised restorations, broad concavities within smooth surface enamel, convex areas flatten, or concavities become present, width exceeds depth, preservation of enamel “cuff” in gingival crevice, and a smooth silky-shining, silky-glazed appearance, and sometimes a dull surface. Signs of attrition (mechanical wear) may be shiny facets, flat and glossy on the incisal surfaces of the incisors, enamel and dentin wear at the same rate, matching wear on occluding surfaces or corresponding features at the antagonistic teeth. Signs of abrasion are usually located on cervical areas of teeth, lesions being of greater width than depth, and commonly affects premolars and cuspids (Gandara and Truelove, 1999; Ganss and Lussi, 2014).
Quantification (intraoral examination)
The severity of the tooth wear may be quantified using the TWES module Quantification into finer-grained occlusal/incisal and finer-grained non-occlusal/non-incisal. The grading scales that are used are an eight-point ordinal scale for the occlusal/incisal surfaces and a three-point ordinal scale for the non-occlusal/non-incisal surfaces (Wetselaar et al., 2009).
Classification
- Filling in the module Quantification, finer-grained occlusal/incisal and non-occlusal/non-incisal, it was revealed that this patient could be classified concerning the distribution and severity as: localized extreme (sextant 2) and generalized severe (sextants 1, 3, 4, 5, and 6) tooth wear. Concerning the origin of the tooth wear, this case was classified as tooth wear with a mixed origin: mechanical/intrinsic (attrition), mechanical/extrinsic (abrasion), chemical/intrinsic (erosion), and chemical/extrinsic (erosion). The origin was based on the qualification, the oral history taking, and some questionnaires.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


