Figure 3.3 Face, frontal, and profile images.
B. Symptom History
- The patient reports pain during rest and function in the left masticatory muscles.
- Pain comes and goes and increases during clenching, chewing, and mandibular movements.
- Pain intensity is 2 (NRS 0–10) at rest but increased to 5 (NRS 0–10) on mouth opening and chewing.
- Pain onset was 2.5 years ago.
- Patient uses chewing gums some of the time and clenches her teeth during the day most of the time (OBCL).
- No functional limitations according to JFLS.
- Mother tells that she and her daughter are concerned about the asymmetry of the daughter’s face.
- Patient chews exclusively with the left posterior teeth.
C. Medical History
- Diagnosed with hypermobility syndrome at the age of 8.
- No known allergies to any food or medication.
- No medications, except for occasional NSAIDs for pain.
- Overall health is very good.
- No sleep-related problems.
- No smoking habits, no use of drugs, no use of caffeine or alcohol.
- Surgeries or hospitalizations: negative.
- Trauma: negative.
- Family medical background: no particular information as reported by the patient or her mother.
D. Psychosocial History
- Parents are married.
- Mother does not work and father works full-time outside the home.
- Middle socio-economic status.
- Patient is a student and a professional swimmer.
- Mother is the primary care giver; patient lives with her parents and a sister aged 12.
- When the patient was evaluated using PHQ-4, -9, and -15 and GAD-7, she expressed she was feeling afraid, as if something awful might happen, several days during the last 2 weeks. She reported no problems at all regarding situations that could have affected her at school, her capacity to take care of things at home, and getting along with other people. However, when the patient was asked about the implications of the face asymmetry, she answered she was concerned about her facial morphology, because the swimming team members have bullied her, so her self-esteem is affected both as an adolescent and as an athlete. She expressed also to be affected by the orofacial pain that sometimes is intolerable, especially after swimming. PSS-10 showed severe stress.
E. Previous Consultation and Treatment
- The patient had undergone comprehensive dental visits each 6 months since she was 5 years old.
- A posterior crossbite was corrected with a fixed orthodontic treatment during the primary dentition in another dental center.
- When the patient was 6 years old, the former dentist told her that, according to the panoramic X-ray at that moment, 46, 47, and 48 were congenitally absent.
F. Extraoral Status
Head and neck
- Normal head and neck morphology.
Hypermobility
- Beighton hypermobility score 7.
Weight and height
- Normal.
- There are no signs of changes in tissue volume or color.
Neurologic findings
- Normal.
Somatosensory abnormalities
- None detected during standard TMJ examination. No additional examination was considered necessary.
Motor function abnormalities
- None noted.
Temporomandibular joint
- Familiar pain in left TMJ during palpation and lateral movements but not familiar pain during palpation of the right TMJ.
Masticatory muscles
- Familiar palpation pain in masseter and temporalis muscles as well as temporalis insertion, bilaterally. Palpation pain, not familiar, in the submandibular region was also detected during palpation.
Jaw movements
- Opening pattern has uncorrected deviation to the left.
- Pain-free opening 40 mm; maximum unassisted opening 45 mm and maximum assisted opening 48 mm, both with familiar pain from masseter and temporalis muscles bilaterally. Horizontal jaw movements are 8 mm to the right, 11 mm to the left, and 8 mm in protrusion; all were pain free.
Neck
- Cervical hypermobility with local pain on movement and palpation but no pain radiation toward the face.
G. Intraoral Status
Dentition
- Full dentition, except that teeth 18, 28, 38, and 46–48 are missing (Figures 3.4 and 3.5).
- Upper left canine in vestibular position without causing any trauma to soft tissues.
- Overbite 2 mm, overjet 1 mm.
- Left molar class I, right molar class cannot be determined, left canine class I and right canine class II. Transversal and vertical asymmetry and crowding in the upper arch; vertical asymmetry in the lower arch and vertical asymmetry in occlusion were noted (Figure 3.5).

Figure 3.4 Dental arches.

Figure 3.5 Occlusion.
Occlusion
- Bilateral contacts premolars and molars in intercuspal position. Canine and anterior guidance.
H. Additional Examination and Findings
- Class II skeletal relationship found in the lateral cephalic X-ray
- Absence of 46, 47, and 48, found in the panoramic imaging.
I. Diagnosis/Diagnoses
DC/TMD
- Myalgia of masticatory muscles.
- Arthralgia of the left TMJ.
J. Case Assessment
- Etiology to the myalgia and arthralgia may be a stress-related muscle hyperactivity.
- Based on the history, overload of the masticatory system may have occurred due to the missing 46, 47, and 48 resulting in mainly unilateral chewing.
- Generalized hypermobility is a risk factor for future musculoskeletal problems and has to be considered in the treatment and follow-up planning.
- The patient has a facial asymmetry, but the asymmetry in itself is not considered as a cause of the myalgia and arthralgia.
K. Evidence-based Treatment Plan including Aims
- Counselling is always the first approach. Provide reassurance regarding the recent state of the disease, explain the nature, the etiology, and the good prognosis of this benign disorder. Thus, detailed information should be given.
- Initial reduction of the pain in the affected muscles with NSAIDs with the aim to put the patient in a better (less pain) position to embrace the coming treatment.
- Reduce repetitive strain of the masticatory system, encourage rest and relaxation, and control the amount of the masticatory activity. Thereafter, ask the patient to undertake stretching exercises for the jaw muscles. In addition, the patient should be instructed to avoid chewing gum and to use the physiological rest position (lips together, teeth apart).
- Exercise therapy is important in the rehabilitation of musculoskeletal disorders, and the model for care is similar wherever the location of the musculoskeletal disease is. The physiotherapy regimen includes “self-management” that facilitates coping for the patient. It has been suggested that these exercises help to relieve musculoskeletal pain and to restore normal function by reducing inflammation, decreasing and coordinating muscle activity, and promoting the repair and regeneration of tissue (Figure 3.6).
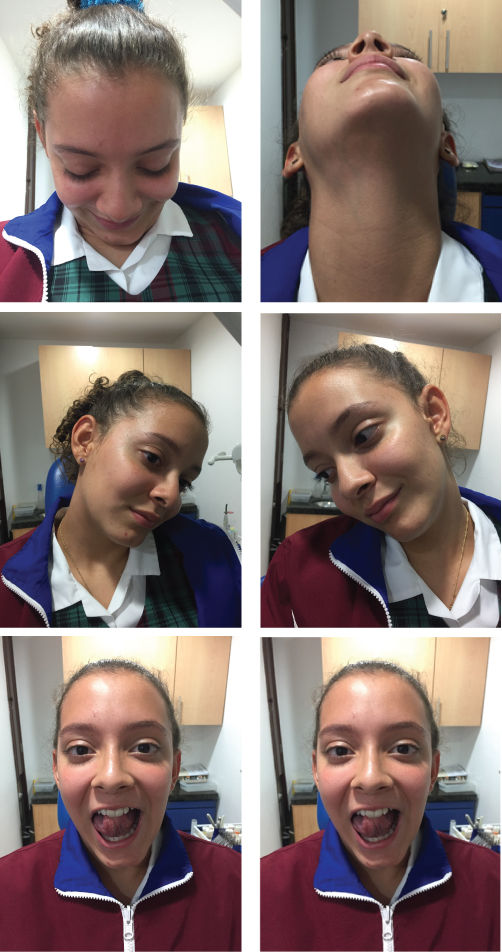
Figure 3.6 Exercises recommended to the patient.
L. Prognosis and Discussion
- The majority of patients respond positively to treatment of myalgia in masticatory muscles and TMJ arthralgia with occlusal splint, massage, exercises, and education to change parafunctional habits, within a short period of time (2–4 weeks).
- After 1 month the patient was pain free. The patient continues to wear the occlusal stabilization splint at nighttime.
- Self-management strategies have been effective and allowed the patient to maintain the results. The patient has been followed up for 8 months and has not reported any TMD sign or symptom.
- Long-term prognosis is good.
Background Information
- Musculoskeletal pain in children and adolescents can be idiopathic or provoked by noninflammatory conditions such as joint hypermobility syndrome. Data from well-controlled epidemiological studies are not available for the prevalence of orofacial myalgia in adolescents, but the available literature reports an estimate of 31%, based on studies in the general population.
- Masticatory myalgia is the most common orofacial pain and is usually accompanied by TMD symptoms. At the same time, TMD is one of the most important causes of pain and disability.
(Yap et al., 2003; Anastassaki and Magnusson, 2004; NICDR, 2014; Romero-Reyes and Uyanik, 2014; Schiffman et al., 2014; Sperotto et al., 2015)
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


