Figure 4.36 Timeline from the start of dystonia symptoms to the examination in the University Clinic for Clinical Oral Physiology.
B. Symptom History
- The condition started 5 years previously with involuntary blinking and spasm of the eyelids.
- Later the patient developed twitches around the mouth and cheeks combined with chewing problems and frequent facial pain (pain intensity 3 on NRS 0–10).
- At the visit to the University Clinic for Clinical Oral Physiology the patient had marked, involuntary oromandibular and perioral activity with high impact on his daily life (7 on an NRS 0–10 for dystonia). Owing to the dystonia the patient often experienced difficult jaw opening as if the teeth were sticking together because of involuntary clenching, biting, or holding the teeth together (score OBCL-21: 13/84). This meant that he could hardly chew or drink from a bottle and had great problems speaking, but no pain-related disability (JFLS). Current pain intensity 2 (NRS 0–10) localized to masseter muscles on both sides.
C. Medical History
- About the start of the eye dystonia the patient suffered from depression treated by the family doctor with citalopram (selective serotonin reuptake inhibitor) over a 1-year period and then discontinued.
- Hypertension diagnosed 3 years ago and since treated with daily intake of amlodipine (calcium channel blocker).
- Weekly intake of paracetamol for relief of facial pain.
D. Psychosocial History
- Married.
- Had to stop his job as a truck driver as a consequence of the eye symptoms.
- Mildly depressed according to PHQ-9, but no anxiety according to GAD-7. Few nonspecific physical symptoms according to PHQ-15, “short of breath” and “feeling tired/having low energy.”
- Has stopped smoking; alcohol on festive occasions.
E. Previous Consultations and Treatments
- Referred to the neurological department from his family doctor.
- In the neurological department the condition was diagnosed and treated with clonazepam (anti-epileptic drug) to relieve the movements, cramps, and seizures.
- As the peroral medication did not offer enough relief of the OMD, the neurologists planned supplementary treatment with intramuscular injections of botulinum toxin (BoNT), but awaited further oromandibular evaluation and suggestions from dental specialists regarding the muscles involved.
F. Extraoral Status
Face
- Frequent eye blinking, grimacing, biting, and lip tightening.
Temporomandibular joint
- No clicking or crepitation at opening and closing movement.
- No pain on palpation.
Masticatory muscles
- Familiar pain on palpation masseter muscles. No referred pain on palpation.
- No pain on palpation of the temporalis muscles.
Jaw movement capacity
- Maximum unassisted jaw opening 52 mm; maximum assisted jaw opening 56 mm. No pain, but with difficulty.
- Laterotrusion to the right and left 6 mm. No pain.
G. Intraoral Status
Soft tissues
- Marginal periodontitis. Else no deviations.
Hard tissues
- Teeth present: 15,13-23,26;47,44-34,37
- Moderate to severe dental attrition and fractured fillings.
Occlusion
- Reduced occlusal stability due to missing teeth, and no contacts on the canines and incisors.
H. Additional Examinations and Findings
- Distorted biting and chewing pattern and increased levels of spontaneous activity during resting posture; see electromyography (EMG) recordings (Figure 4.37) and diagram from surface EMG (Figure 4.38).
- Intramuscular EMG from the masseter, the anterior digastric and the orbicularis oris muscles measured during dystonic activity showed an interference pattern above 100 turns per second.
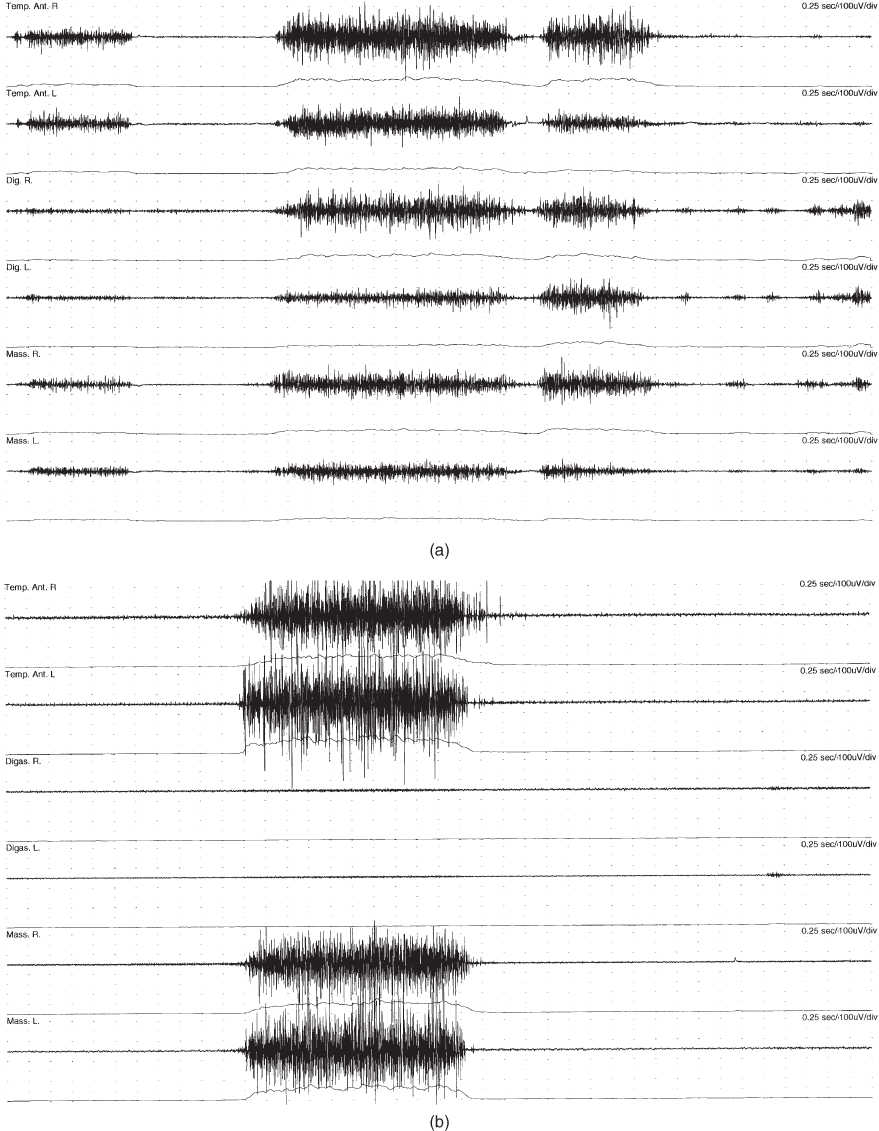
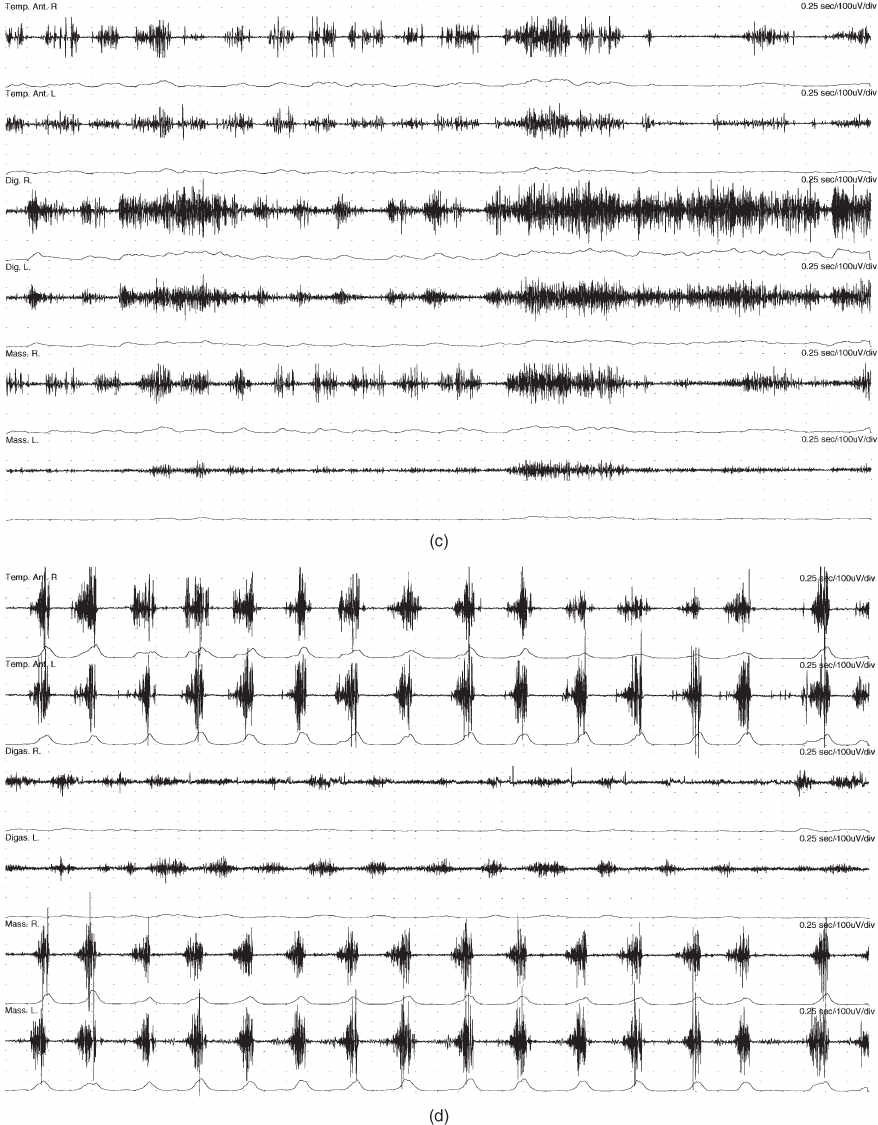
Figure 4.37 EMG recordings with bipolar surface electrodes from masticatory muscles during a short clenching task and during chewing of a piece of apple in the case patient and in a control subject. From top to bottom: anterior temporalis muscles (Temp. R and L), anterior digastric (Digas. R and L) and masseter muscles (Mass. R and L) with same amplification and same timing scale in all recordings. For each muscle the raw signal is shown first and below the rectified mean voltage (Bakke et al., 2013). (a) Patient, voluntary maximum clenching: prolonged and blocked biting with ongoing activity in the jaw closing muscles (temporalis and masseter muscles) and overflow of antagonistic activity in the digastric muscle. (b) Control, voluntary clenching: normal EMG pattern during maximum bite with very high activity in the jaw closing muscles and very low antagonistic activity. (c) Patient, chewing of apple: distorted chewing pattern with high antagonistic activity. (d) Control, chewing of apple: well-defined chewing cycles with much lower activity in jaw opening than jaw closing muscles.
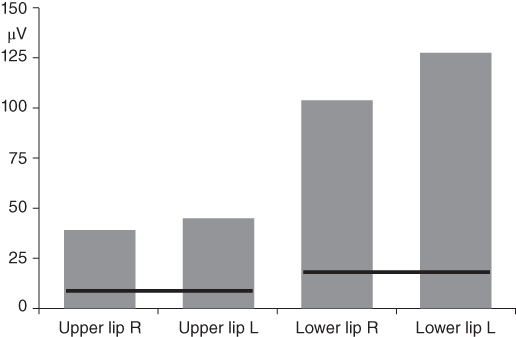
Figure 4.38 High dystonic activity in the lips during resting posture in the case patient. The gray columns represent the average levels of the mean rectified voltages recorded with bipolar surface electrodes over the superior orbicularis (Upper lip R and L) and the inferior orbicularis oris muscles (Lower lip R and L) (Bakke et al., 2013). The black lines indicate the mean plus two standard deviations of corresponding reference values from surface EMG in healthy subjects (Electromyography Laboratory, Clinical Oral Physiology).
I. Diagnosis/Diagnoses
Expanded DC/TMD
- OMD.
DC/TMD
- Myalgia (masseter).
J. Case Assessment
- Only some of the patients with OMD have pain from the TMJ and/or masticatory muscles and most OMD conditions are idiopathic; that is, with no sensory deficits and no peripheral myopathic disease. As a consequence, TMD pain, sensory deficits, and peripheral myopathic disease are not necessarily prerequisites for neurologists to diagnose OMD (see Diagnostic Criteria box). However, the OMD patients may still have dental problems and impeded orofacial function caused by the disease and need treatment from dentists (Bakke et al., 2013; Peck et al., 2014).
- In the present case the dystonia was idiopathic. It was also unclear whether the myalgia was related to the dystonia or other factors, such as the reduced occlusal support. In addition, the patient suffered from depression. Patients with dystonia are more likely to experience mental health conditions such as depression. Here, it seemed to be related to his difficulties in leading an ordinary life and having a job (Conte et al., 2016).
K. Evidence-based Treatment Plan including Aims
- To reduce dystonic activity to improve orofacial function, relieve masseter pain, and prevent further dental deterioration by injections with botulinum toxin (BoNT) in the muscles involved (see Fundamental Points box).
- Later dental treatment.
L. Prognosis and Discussion
-
BoNT does not cure dystonia. When injected into the muscles involved the BoNT alleviates the OMD temporarily, but the treatment has to be repeated at regular intervals. In the present case the treatment reduced the impact of the OMD on his daily life from 7 to 3 (0–10 NRS), and the intake of paracetamol for facial pain was seldom. The maximal active jaw mobility increased from 52 mm to 58 mm and the blockages of the jaw during mastication decreased.
- There was a great need for oral rehabilitation and general dental treatment; however, treatment may be difficult to manage in these cases because of the dystonic activity (especially tooth preparations, dental impressions, etc.) and of the costs of extensive dental reconstructions (e.g., the patient’s financial condition, insurance). Protection of the teeth with splints is seldom used, as the dystonic movements are usually only present during wakefulness.
Background Information
Definition of dystonia
-
Dystonia is a movement disorder characterized by sustained or intermittent muscle contractions causing abnormal, often repetitive, movements, postures, or both. Dystonic movements are typically patterned, twisting, and may be tremulous. Dystonia is often initiated or worsened by voluntary action and associated with overflow muscle activation (Albanese et al., 2013).
Characteristics of oromandibular dystonia
- OMD is a rare focal neurological disorder localized to the lower part of the face and jaws and affecting less than 30 per 100 000 persons.
- Onset is often in the sixth decade of life and more common in women than in men.
- OMD is caused by functional changes in brain areas that contribute to control and performance of conscious and unconscious movements; it may be inherited or acquired, but in most cases OMD is idiopathic.
- OMD is characterized by jaw movements and deviations, restless tongue, and facial grimacing caused by the masticatory, facial, pharyngeal, lingual, and/or lip muscles; consequently, chewing, swallowing, and speech may be hampered.
- OMD is usually associated with a feeling that the face and jaws are never at rest as well as fatigue in affected muscles, but rarely with pain.
- OMD may look similar to sleep bruxism, but it is present when the patient is awake and usually ceases during sleep.
- OMD is incapacitating as it may affect facial expression, resulting in social isolation and lack of acceptance from those around him.
- OMD may cause severe attrition of the teeth and problems with prosthetic reconstructions and dentures.
- OMD may be misdiagnosed as TMDs, dental problems, or as psychiatric manifestations.
-
In most countries, specialists in neurology have the responsibility for the final decision on the diagnosis as well as the treatment of OMD, but dentists should be able to recognize the condition and refer to the proper specialists.
- Presently, there is no general agreement about a precise definition of OMD and the difference between OMD and dyskinesia; however, dyskinesia is in contrast to dystonia most often described as a side effect of medication.
- OMD has currently no cure, but there are treatment options to manage symptoms, such as peroral medication with clonazepam, intramuscular injections with BoNT and in special cases deep brain stimulation with implanted electrodes.
(Bakke et al., 2007, 2013; Balasubramaniam and Ram, 2008)
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


