Figure 2.32 Left side of mandible is shorter than the right.
G. Intraoral Status
- Maximal incisal opening at first visit was 42 mm (Figure 2.33).
- Slight deviation of jaw to right with mouth opening (Figure 2.34).
- Increased condylar movement of the left TMJ.
- Post-normal tooth relation on the left side.
- Stable occlusion.
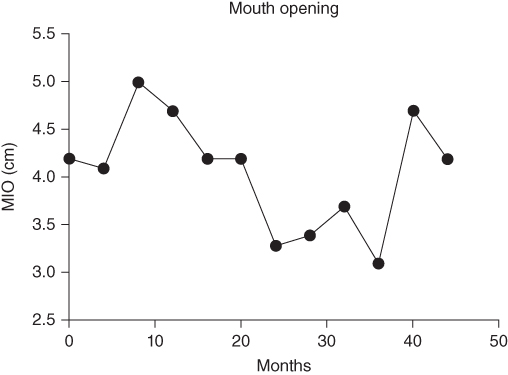
Figure 2.33 Maximal incisal opening over time.

Figure 2.34 Deviation with mouth opening.
H. Diagnosis/Diagnoses
Expanded DC/TMD
- Systemic arthritides.
DC/TMD
- Arthralgia left TMJ.
Other
- Juvenile idiopathic arthritis (JIA).
I. Additional Examinations and Findings
- TMJ MRI with contrast revealed: normal right TMJ; left TMJ with anterior flattening of condyle, small erosions, pannus anteriorly, and mild periarticular contrast enhancement (Figure 2.35).
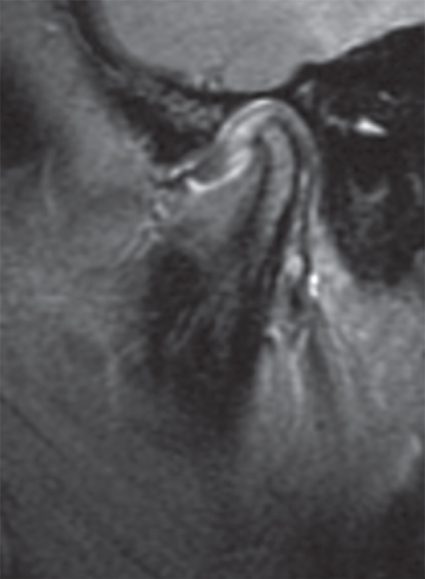
Figure 2.35 TMJ MRI at onset revealing acute and chronic left TMJ arthritis.
J. Case Assessment
- Likely JIA as cause of TMJ pain, based on imaging and history of other joint pain.
- Idiopathic chondrolysis is in differential diagnosis, which may ultimately be JIA.
- TMD with orofacial pain as a cause of parafunctional activity is in differential diagnosis and could be a reason to insert behavioral and relieving treatment as a complement.
- TMJ arthritis in children also occurs in other rheumatic disorders (e.g., sarcoidosis, Sjögren’s, mixed connective tissue disease, dermatomyositis), but for this patient there were no signs/symptoms to suggest these diseases as the cause of her TMJ arthritis (Stoll and Cron, 2015).
K. Evidence-based Treatment Plan including Aims
- Stop progression of ongoing TMJ inflammation.
- Minimize TMJ pain associated with TMJ arthritis.
- Maintain mouth opening and function.
- Systemic anti-arthritis therapy, including biologic agents (e.g., TNF inhibitors) (Stoll et al., 2015).
- Intraarticular long-acting corticosteroids (Ringold and Cron, 2009).
- Oral functional appliances may help to reduce pain, improve jaw movement, and maintain normal mandible and mid-face growth in children with JIA when used routinely over several years (Portelli et al., 2014; Stoll and Cron, 2015).
L. Prognosis and Discussion
- Guarded prognosis in terms of TMJ arthritis in JIA as it remains a difficult-to-treat joint (Stoll and Cron, 2015).
- TMJ arthritis can progress (as noted on MRI) despite aggressive systemic therapy for JIA (Stoll et al., 2015).
- TMJ arthritis may or may not respond to systemic therapy or to intraarticular immunosuppression (corticosteroids or TNF inhibitors) (Stoll et al., 2015).
- Undertreated or unresponsive progressive TMJ arthritis in growing children can lead to micrognathia, mid-face growth disturbances, facial asymmetry, poor mouth opening, and TMJ pain at rest, or with activity (e.g., eating, speaking; Arabshahi and Cron, 2006).
- Over the following 2 years, she received intraarticular corticosteroids to her left TMJ on two occasions.
- In addition, her TMJ arthritis and JIA (other joints) were managed with systemic TNF inhibitors, eventually switch to co-stimulatory blockade (CTLA-4-Ig).
- Two years later, TMJ MRI showed normal right TMJ, left TMJ condyle flattening with erosions over the majority of the articular surface, bone marrow edema, 4 mm effusion, diffuse synovial thickening, increased pannus, and disc displacement anteriorly and medially (Figure 2.36).
- Her TMJ symptoms are markedly improved after therapy.
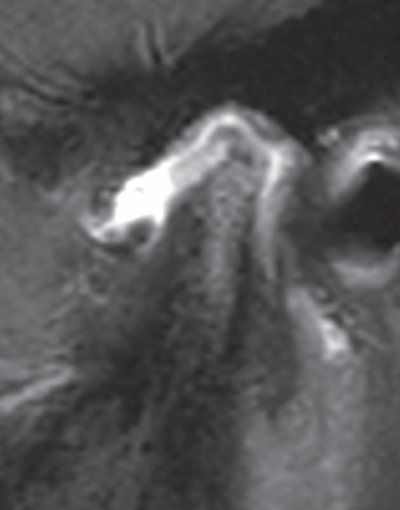
Figure 2.36 Worsening left TMJ arthritis by MRI over time.
Background Information
- As many as 80% of children with JIA have TMJ arthritis, including at disease onset (75%) (Ringold and Cron, 2009).
- TMJ arthritis at onset has often been considered asymptomatic, but TMJ pain or facial pain, as well as decreased TMJ mobility, seem to be important risk factors (Ringold and Cron, 2009; Leksell et al., 2012).
- Deviation to the involved, or more involved, side with mouth opening is a strong predictor of TMJ arthritis. The patient reported herein unusually demonstrated deviation toward the unaffected TMJ with mouth opening despite having a shorter mandible on the affected side (Stoll and Cron, 2015).
- The most sensitive diagnostic tool for detecting TMJ arthritis in children with JIA is MRI with contrast. Ultrasound and clinical exam are neither sensitive nor specific for detection of early TMJ arthritis in children with JIA with current methods (Ringold and Cron, 2009).
- Chronic bony changes (e.g., condylar head flattening and erosions) on MRI are highly specific for TMJ arthritis in the setting of children with JIA, but mild synovial enhancement with contrast may be a normal finding. Pannus seen on MRI, however, is always abnormal (Stoll and Cron, 2015).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


