Figure 4.5 Patient, who co-created this image of herself with an artist.
© Deborah Padfield and AE from the series Face2face.
C. Medical History
- Hernia operation, hypertension.
D. Psychosocial History
- Married with one son. Graphic designer, writer, paints. No significant life events.
- Experiences fatigue, occasionally wakes at night; when severe, pain episodes impact on activities of daily living. No anxiety or depression when pain is controlled.
E. Previous Consultations and Treatments
- First episode: pain in the upper right quadrant while eating. It was thought to be related to an old crown. She had endodontics and then extraction of the tooth, none of which relieved the pain. Everything settled after about 11 days.
- Second episode: 8 months later, pain same location; opioids, diazepam and third molar extraction, no help.
- Nine months later a diagnosis of trigeminal neuralgia (TN) was made and gabapentin started, which reduced the pain. The patient was referred to the facial pain unit.
F. Extraoral Status
- No gross neurological abnormality.
- No TMJ sounds and no TMJ or masticatory muscle pain on palpation. Jaw movement capacity is within normal ranges.
G. Intraoral Status
- Dentate with an extensively restored dentition.
H. Additional Examinations and Findings
- MRI scan shows neurovascular compression of the trigeminal nerve in the region of the root entry zone on the right side (Figure 4.6).
Figure 4.6 MRI showing trigeminal nerve in contact with a vessel.
I. Diagnosis/Diagnoses
ICDH-3 beta
- Classical TN right side.
J. Case Assessment
- This is a typical case of classical TN affecting the maxillary and mandibular branches of the trigeminal nerve. Pain is provoked by oral behaviours such as talking, eating, brushing the teeth and washing the face and is recurring in episodes with full remission in between.
- Although she has classical TN, the major problem is the fear of return of severe pain and how she would cope with it.
K. Evidence-based Treatment Plan including Aims
- As gabapentin had not been effective it is important to use one of recommended drugs, and international guidelines suggest either carbamazepine or oxcarbazepine. She was started on oxcarbazepine, as this drug has improved tolerability.
- She was provided with information leaflets and details of patient support group (www.tna.org.uk) and had a joint consultation with a neurosurgeon and physician to discuss possible surgical options. Recent studies have suggested that fear, lack of confidence and isolation play a role in this condition, so she participated in a psychology pain management group programme with other patients with TN.
L. Prognosis and Discussion
- The patient was pain free 13 months later; low-dose drug only.
- Fourth episode 24 months later, return of pain; used oxcarbazepine for control and stopped when pain free (Figure 4.7).
- Fifth episode 35 months later – recurrence, Brief Pain Inventory showed pain intensity 10/10, quality of life severely affected, anxiety and depression on Hospital Anxiety and Depression scale. On high-dose oxcarbazepine developed hyponatraemia. Unable to control pain medically (Figure 4.8).
- Microvascular decompression to decompress nerve 36 months later and now 1 year on is pain free and off medications.
- One of the main questions posed by patients relates to their prognosis, especially when they are first diagnosed. A systematic review of the epidemiology and diagnosis of this condition shows that there are no studies that provide data on the long-term prognosis. TN is well known to result in natural periods of pain remission, and these seem to be extremely variable in length (Rothman and Monson, 1973). Not all patients require surgery, and some can be managed medically for many years.
- How patients make decisions about treatments is difficult to understand and is compounded by the lack of high-quality evidence. A recent study suggested that surgical management is preferred to medical.
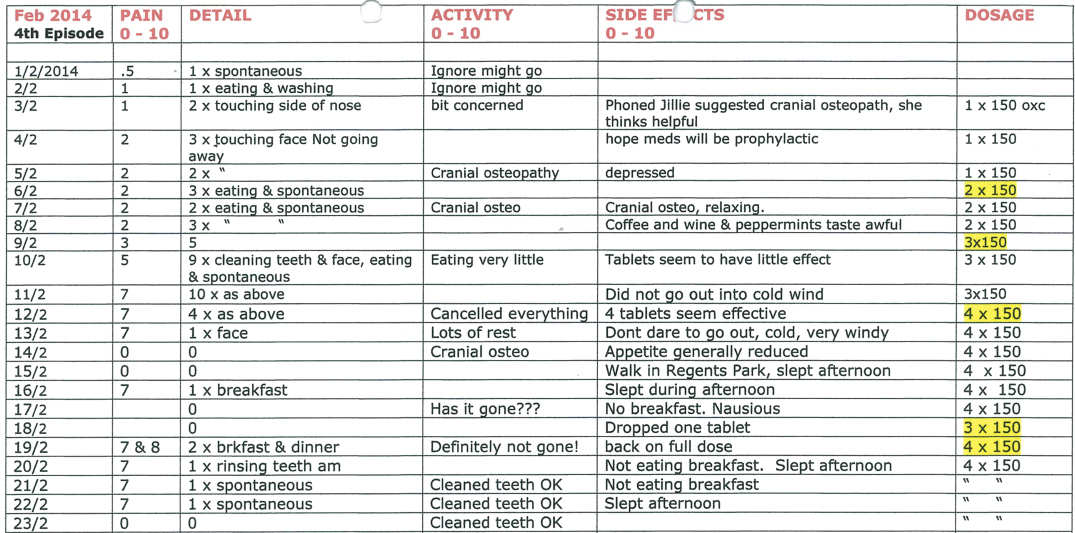
Figure 4.7 Diary kept by patient of fourth episode of pain.
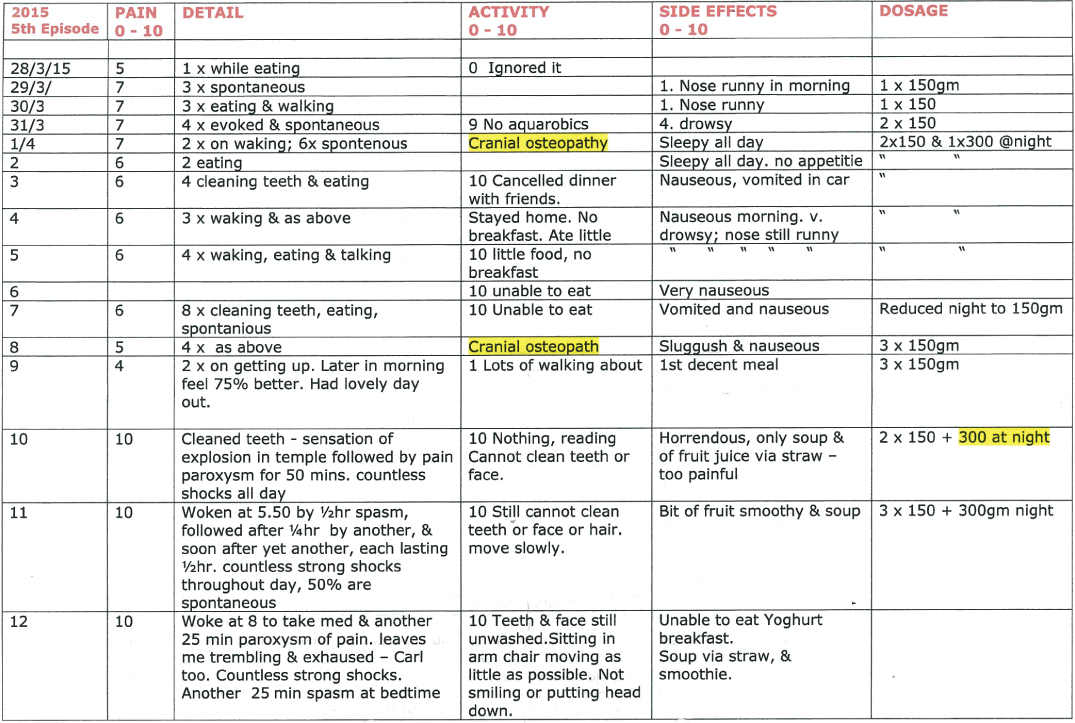
Figure 4.8 Diary kept by patient of fifth episode of pain.
Background Information
Epidemiology
- Older studies have estimate that the prevalence of TN ranges between 0.3% and 4.9% in the general population, with an annual incidence of 2.1 to 4.7 new cases per 100 000 persons, but this is thought to be higher. Females are slightly more frequently affected by TN compared with males. In a recent survey of UK general practitioner practices, it an incidence of 26.8 per 100 000 persons per year was estimated, but the disorder is often misdiagnosed, and in a similar study done in Holland, where neurologists validated the diagnosis, the incidence rate was 12.6 per 100 000 person years (confidence interval 10.5–15.1).
- The disease most frequently linked with TN is multiple sclerosis. Hypertension may be a risk factor, and tumours constitute a very small group of symptomatic cases. No genetic basis has been found, but there are reports of familial occurrence. Wu et al. (2015), in a population-based study in Taiwan, reports that TN was associated with increased depression, anxiety and sleep disturbance, but no other psychosis.
Aetiology and pathophysiology
- TN remains a disease of unknown aetiology and its pathophysiology is not completely understood (Devor et al., 2002). A vascular compression of the trigeminal nerve at its root entry zone in the posterior fossa of the skull is found in many patients. This causes demyelination and ephaptic transmissions, resulting in paroxysmal pain. Up to 20% of the population have neurovascular contact and yet only a small percentage develop TN. There is growing evidence that patients with TN have an abnormality of their sodium channels, which are important in nerve conduction, as well as a potential myelin defect, and central inhibitory pathways are abnormal.
Diagnosis
- The clinical features of TN have been described in a recent series of papers from the Danish Headache Centre (Maarbjerg et al., 2014), but there are very few studies that have evaluated these over a longer period of time.
- More recently it has become increasingly clear that the classical description of TN as suggested in both the International Association for the Study of Pain and ICHD classifications is more complex (Headache Classification Committee of the International Headache Society (IHS), 2013).
- There are two conditions that have many similar characteristics to TN, short-lasting unilateral neuralgiform headache attacks with autonomics (SUNA), or short-lasting unilateral neuralgiform headache attacks with conjunctival injection and tearing (SUNCT). It is now being suggested that all these disorders may be part of a continuum of the same disorder, as autonomic features may be noted not only in these conditions but also with TN.
- Tölle et al. (2006), in their study of 89 European patients with TN, show the significant impact that this condition can have on activities of daily living as reported on the Brief Pain Inventory, a self-completed questionnaire. Using an extended Brief Pain Inventory Facial, neurosurgeons have been able to show how quality of life improves when patients are managed surgically. Phenotyping these patients at baseline is therefore crucial when assessing outcomes.
Management
- The wide range of treatments currently in use for TN is ample evidence that there is no simple answer to how TN should be managed. Trials in TN patients are difficult to conduct for a number of reasons, including; its relative rarity, its unknown aetiology, its natural history of spontaneous remission, its varying severity and the lack of objective diagnostic tests. The condition is in the first instance treated with anti-epileptic drugs, some of which have been evaluated in randomized controlled trials (Zakrzewska and Linskey, 2014).
- There is a wide range of surgical treatments (Zakrzewska and Linskey, 2014). Some are destructive, mostly carried out at the level of the Gasserian ganglion under a short anaesthetic and result in pain relief for a few years but result in variable sensory loss. Microvascular decompression is a non-destructive procedure involving a major neurosurgical procedure linked with a 0.4% mortality rate. The procedure results in the longest pain-free interval. There are very few randomized controlled trials of surgery.
- Patient support groups have provided thousands of patients worldwide with access to improved quality data on which to make decisions about treatment and, more importantl, provide psychological support.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


