Figure 2.49 Preoperative CT-radiographic picture showing a left subcondylar fracture with a lateral displacement of the condylar fragment (C).
I. Diagnosis/Diagnoses
Expanded DC/TMD
- Left condylar fracture. Other mandibular fractures may not be excluded at this point.
DC/TMD
- Masticatory muscle myalgia.
- Left TMJ arthralgia.
Other
- Fractured teeth.
J. Case Assessment
- The combination of an acute trauma, changed occlusion, and painful and reduced mandibular motion capacity with difference in maximal laterotrusive movements between the right and left side prompted a suspicion of a condylar fracture.
- The suspicion was strengthened by the lack of palpable condylar movements on the left side, difference in ramus height between the right and left side, and palpation pain of the left TMJ region.
- A clinical differential diagnosis based on pain, altered occlusion, and impaired laterotrusion after a trauma is an acute traumatic arthritis of the TMJ. When this happens there is usually a swelling in the TMJ on the affected side and changes of the occlusion with primary contacts on the contralateral side, as an edema in the traumatized joint will press the condylar head in a caudal direction. At laterotrusion there is usually a normal range of motion to the affected side and an impaired range of motion to the opposite side. These facts make this differential diagnosis less likely.
- The combination of a trauma, reduced motion capacity, and deviation of the lower jaw and changed occlusion makes an additional radiographic examination indicated in order to check for fractures.
K. Evidence-based Treatment Plan including Aims
- The aim for treatment of condylar fractures is to normalize the occlusion during healing. This can be done by the aid of either closed treatment or open surgery. If a condyle is minimally displaced or not displaced, closed treatment is the method of choice.
- During closed treatment, minor occlusal changes may be initially observed for some days. Usually, the occlusion will be normalized spontaneously. However, if not, it may have to be guided with nonrigid or rigid fixation attached to alternatively arch bars, brackets, or intermaxillary fixation screws (Figure 2.50).
- Major displacement of a fractured condyle resulting in a more disturbed occlusion is nowadays frequently reduced and fixated by open surgery, allowing anatomic repositioning and immediate postoperative function of the jaw. Usually, an extraoral approach is then used. When the fracture is exposed it can be reduced and fixated with titanium plates and screws (Figures 2.51 and 2.52). If so, the occlusion is usually temporarily fixated during the surgical procedure.
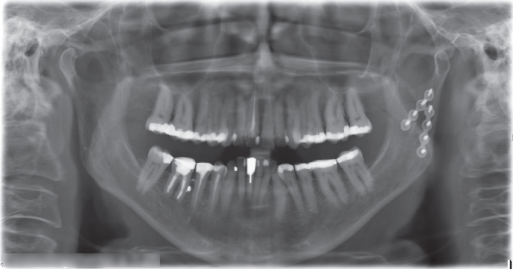
Figure 2.50 Postoperative panoramic radiograph showing repositioned condylar fracture on the left side fixated with two titanium plates and screws.
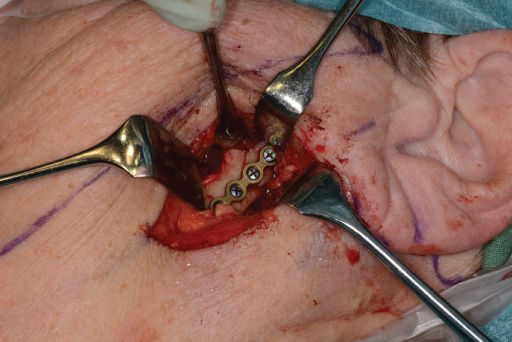
Figure 2.51 Fracture site exposed via a submandibular incision. The subcondylar fracture reduced to correct position (arrow) and fixated with titanium plates and screws.

Figure 2.52 Intermaxillary fixation with elastics attached to screws in the alveolar process for guidance of a bite with a fractured condyle to correct occlusion.
L. Prognosis and Discussion
- The prognosis of closed treatment of condylar fractures as well as for open surgery is, in general, good. In some cases it is not feasible to expect an anatomic reduction of the condylar fracture, but minimal to moderate displacement of the condylar segment generally results in adequate postoperative function and occlusion. A prerequisite for that is that a proper occlusal relationship is established during the period of healing of the fracture.
- Generally, intermaxillary fixation is used in adults for a maximum of 2–3 weeks. In children, intermaxillary fixation is unusual but can in specific cases be used for 10–14 days, followed by a period of aggressive functional rehabilitation (Tucker, 1998). In particular, at intracapsular fractures early mobilization is essential to avoid intraarticular adhesions.
- Patients with displaced fractured condyles should, according to a systematic review and meta-analysis by Al-Moraissi and Ellis (2015), be treated with open reduction with internal fixation as this handling provides a superior clinical outcome compared with closed treatment. A disadvantage with open reduction is the risk of damage to the facial nerve, resulting in paralysis and the risk of formation of scars and infection. In children, open surgery is usually not indicated for treatment of condylar fractures as their capacity to remodel a displaced condyle to normal configuration is excellent.
Background Information
- The incidence of condylar fractures has been estimated to be about 1/1000 persons. In a retrospective analysis of more than 4000 mandibular fractures the majority of patients were men (83%) with a mean age of 38 years, and condyle or subcondylar fractures occurred in 18% of the mandibular fractures. Most injuries occurred in the summer months (Morris et al., 2015). In a study of mandibular fractures treated at a Swedish university hospital from 1999 to 2008, 70% of the patients were men and 50% were aged 16–30 years (Ramadhan et al., 2014).
- According to Ramadhan et al. (2014), the most common reasons for mandibular fractures were interpersonal violence (24%), falls (23%), and traffic accidents (19%), while Morris et al. (2015) reported that low-velocity blunt injuries caused 62% and high-velocity blunt injuries 31% of the mandibular fractures in their study.
- Condylar fractures are divided into three sites: the condylar head (intracapsular), the condylar neck (extracapsular), and the subcondylar region (Zachariades et al., 2006). Unilateral condylar fractures represented two-thirds of the condylar fractures, and 19% of the condyles were nondisplaced, 12% deviated, and 69% displaced.
- Significant differences in treatment outcome have been reported by Al-Moraissi and Ellis (2015) between open reduction and closed treatment with rigid internal fixation regarding maximal interincisal opening, laterotrusive movements, protrusive movement, malocclusion, pain, and chin deviation on mouth opening. Even though the incidence of facial injury is high, it is difficult to collect data, particularly when long-term evaluation is required, as rates of compliance and attendance at follow-up tend to be low (O’Connor et al., 2015). The number of large-scale studies is therefore small. A concerted effort to collaborate nationally and across different specialties to undertake larger studies will help to improve the outcome. Quality of life based on patient satisfaction after open versus closed treatment for mandibular condyle fractures should also be better evaluated (Kommers et al., 2013).
- Ankylosis of the TMJ is a feared complication. Often it is due to hemarthrosis, occurring at condylar head fractures within the joint capsule, that is responsible for the ankylosis (Hackenberg et al., 2014). At these types of fractures early mobilization of the jaw is essential. At subcondylar fractures, fractures situated below the attachment of the joint capsule, closed treatment with intermaxillary fixation can be used with a minor risk of ankylosis.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


