Figure 4.29 Preoperative radiograph.
I. Diagnosis/Diagnoses
Other
- Pulp necrosis tooth 46.
- Symptomatic apical periodontitis tooth 46.
J. Case Assessment
- The source of the patient’s pain in this case is inflammation of the periapical tissues of the mandibular right first molar. The etiology of the patient’s problem is bacteria. The pulp has undergone necrosis, and the periapical tissues are inflamed as result of bacteria, necrotic tissue, and inflammatory mediators in the root canal system. Bacteria likely entered the pulp due to a history of dental caries, but a crack or leaking restoration are other possible etiologic factors.
- The patient’s history, signs, and symptoms are a classic example of pain due to symptomatic apical periodontitis. The differential diagnosis could include an acute apical abscess, chronic apical abscess, or pain of non-odontogenic origin. However, the clinical exam does not indicate evidence of pus formation, and the radiographic findings indicate the presence of apical periodontitis due to endodontic origin.
- The diagnoses in this case were made based on the patient’s reported history of pain, the diagnostic test results, and the radiographic findings. The patient’s history of sensitivity to chewing is suggestive of a periapical diagnosis of symptomatic apical periodontitis. This periapical diagnosis was confirmed clinically by the sensitivity to percussion. The presence of periapical radiolucencies on the radiograph further indicate the presence of apical periodontitis. The pulpal diagnosis of pulp necrosis was made based on the lack of response to the cold test and EPT. All diagnostic test results were assessed in relation to the adjacent teeth in the quadrant.
K. Evidence-based Treatment Plan including Aims
- Treatment options for tooth 46 include: (1) nonsurgical root canal therapy, followed by a definitive build-up restoration and crown, (2) extraction, and (3) do nothing.
- The aim of the treatment is to eliminate the bacteria, necrotic tissue, and inflammatory mediators in the root canal system to eliminate the source of the patient’s pain. This can be accomplished through endodontic therapy or extraction of the tooth. After the bacteria, necrotic tissue, and inflammatory mediators are removed, the inflammation of the periapical tissues should resolve.
- Endodontic treatment plan: nonsurgical root canal therapy (Figure 4.30).
- If the patient elects to maintain the tooth through endodontic therapy, the tooth must be properly restored after root canal therapy. A crown restoration is recommended in order to prevent fracture of the tooth or recontamination of the root canal system through coronal leakage, and to provide long-term function for the patient.
- Restorative treatment plan: build-up and crown.

Figure 4.30 Postoperative radiograph.
L. Prognosis and Discussion
- The prognosis is favorable. After the root canal system is cleaned and disinfected, periapical inflammation and the patient’s pain should resolve. If proper endodontic therapy and restoration are provided, there should be no further bacterial contamination. The apical periodontitis will heal, and the tooth will provide long-term function for the patient. Resolution of apical periodontitis is evidenced by resolution of the patient’s symptoms in the short term, and radiographic evidence of healing in the long term (Figure 4.31).
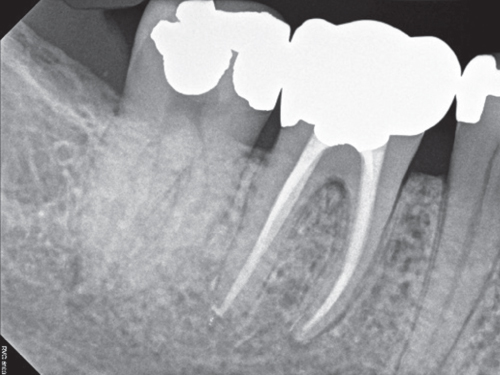
Figure 4.31 The 1 year follow-up radiograph.
Background Information
- Apical periodontitis is inflammation of the tissues surrounding the apex of a tooth. Asymptomatic apical periodontitis is defined as inflammation and destruction of the apical periodontium that is of pulpal origin, appears as an apical radiolucent area, and does not produce clinical symptoms (American Association of Endodontists (AAE), 2015).
- Symptomatic apical periodontitis is defined as inflammation usually of the apical periodontium, producing clinical symptoms including a painful response to biting and/or percussion or palpation. It might or might not be associated with an apical radiolucent area (American Association of Endodontists (AAE), 2015).
- Apical periodontitis is a common condition in the adult population. For research purposes, the prevalence of apical periodontitis is typically measured by detecting the presence of radiographic changes. In a sample of over 5000 adults in Finland, the prevalence of apical periodontitis as detected on panoramic radiographs was 27% of subjects. The prevalence was greatest on teeth with inadequate root canal fillings, and apical periodontitis was more prevalent in males versus females (Huumonen et al., 2016).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


