Figure 2.21 (a) Profile of 18-year-old female with bony ankylosis of left TMJ. (b) No mandibular movements. Teeth had erupted until they met the antagonizing teeth. Manifest caries and endodontic problems.
G. Intraoral Status
- Upper and lower teeth in contact; not possible to move mandible.
- Several remaining roots.
- Loss of upper front teeth.
H. Additional Examinations and Findings
- Panoramic radiograph, lateral cephalogram, CT (Figures 2.22 and x.23).
- Appointment with anaesthesiologist in order to evaluate nasal intubation or tracheotomy before surgery.

Figure 2.22 CT with ankylosis of left TMJ, which also shows deviation of the mandible to affected side and asymmetry.
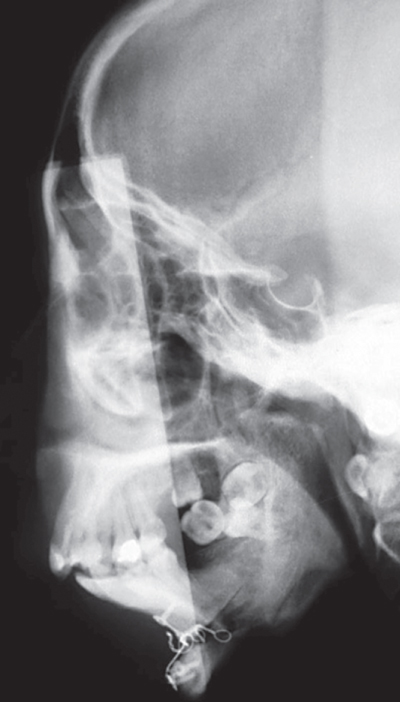
Figure 2.23 Lateral cephalogram after resection of left TMJ ankylotic part, genioplasty and removal of eight roots.
I. Diagnosis/Diagnoses
Expanded DC/TMD
- Left TMJ osseous ankylosis.
Other
- Sequela after mandibular fracture.
- Sleep apnoea.
- Mandibular micrognathia.
- Periodontitis.
- Caries.
J. Case Assessment
- Nutritional challenges. The patient has never had regular meals, only soft liquids. Necessary to give nutritional information and teaching.
- Since the patient should return home shortly after the end of the surgical treatment, there was limited time for dental rehabilitation.
- Only the most necessary treatment will be possible to perform before the patient has to return home.
- In TMJ ankylosis the maxillary artery and other vessels in the TMJ area may be embedded in the ankylosed TMJs. During surgery, excessive bleeding from the ankylosed bone may occur. It is therefore important to evaluate the maxillary artery by CT with angiography.
- Facial paraesthesia is a complication that may occur after all TMJ surgery but is more frequent in ankylosis cases.
- Re-ankylosis may occur. There may, therefore, be a need for another surgical intervention.
- In the treatment planning we have to consider ankylosis resection, interpositional arthroplasty with temporalis myofascial flap or dermis–fat transplantation or reconstruction with a prosthetic total joint in the treatment of this patient.
K. Evidence-based Treatment Plan including Aims
Treatment goals
- Healthy dentition.
- Adequate dental hygiene.
- Normal mandibular movement capacity.
- Normal facial appearance and profile.
Management
- Simultaneous condylectomy with temporalis myofascial flap.
- Removal of infected roots.
- Genioplasty.
- Dental restorations.
- Physical therapy of masticatory muscles.
L. Prognosis and Discussion
- In this case, orthodontic treatment after the condylectomy and removal of dental roots should be considered. Endodontic treatment should also be considered.
- After dental treatment and alignment of teeth, bimaxillary surgery could then have been performed to enhance the facial profile and correct the asymmetry.
- In the present case, only limited time was available for treatment since the patient had to go back to the family for different reasons. The postoperative result, however, was adequate in relation to the patient’s expectations and the preoperative starting point (Figure 2.24).
- Surgical treatment of TMJ bony ankylosis is challenging, and so far the surgical treatments are based on case studies and are not evidence based. Surgical treatment of ankylosed TMJs should preferably be centralized to a few institutions.
- There is a possibility of re-ankylosis. Therefore, care has to be taken to cautiously remove a sufficient volume of the ankylosed condyle. The range of motion has to be checked during surgery to evaluate how much the maximal range of motion can be after surgery. In this case, the masticatory muscles had not been used for chewing and there was a severe atrophy of the muscles. Training and physical therapy are therefore a crucial part of the postoperative treatment.
- The postoperative range of motion was 25 mm at 1 week, and it had increased to 37 mm at 3 months. The profile was acceptable and the patient was happy with the result. No complications such as facial nerve paraesthesia were seen.
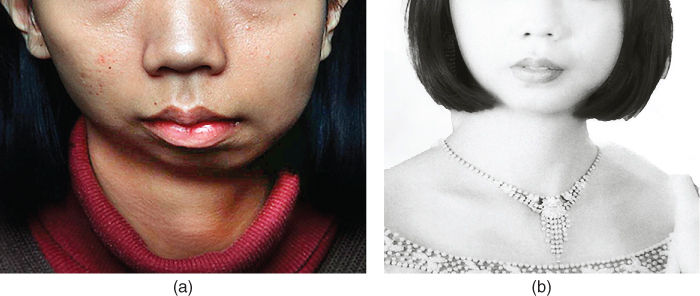
Figure 2.24 (a) Preoperative facial view. (b) Picture sent to surgeon 1 year after surgery from her residential home.
Background Information
- Bony ankylosis of the TMJ is a very rare condition that most often affects one TMJ (Loveless et al., 2010).
- The aetiology may be untreated condylar fractures, other trauma, iatrogenic causes such as previous surgical interventions or inflammatory diseases such as immunological diseases (e.g. rheumatoid arthritis, ankylosing spondylitis, juvenile idiopathic arthritis) (Loveless et al., 2010).
- The ankylosis will in most cases appear gradually with decreased range of motion as one of the clinical signs. Pain may or may not be present.
- Radiographically, a panoramic radiograph may give the first indication of pathology of the TMJs.
- CT or CBCT is the best radiographic examination to detect TMJ bony ankylosis. MRI may give additional information about any active inflammation. CT with angiography is recommended to evaluate possible vessels inside the ankylosed part of the TMJ.
- CT signs of erosion, destruction, bone remodelling and bone formation may be seen in the development of the bony ankylosis.
- Even if there is bony ankylosis, the patients may have some degree of range of motion because of the elasticity of the mandible.
- If bony ankylosis appears in a growing child, severe maxilla–mandibular growth disturbances may appear.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


