A cross-sectional study is an observational study in which the exposure and the outcome are determined at the same time point for each study participant. Cross-sectional studies comprise the simplest individual-level observational study design and are usually relatively inexpensive and easy to conduct compared with case-control or cohort studies.
Cross-sectional studies can be descriptive or analytical depending on whether the outcomes are assessed for potential associations with risk factors or exposures. Another type of cross-sectional study is the serial cross-sectional study, in which more than 1 data collection is conducted in the same study population at different time points.
In a hypothetical example of a cross-sectional study, we can record the prevalence of periodontal disease and investigate the association between periodontal disease and oral hygiene habits in adult patients. The outcome is the presence or absence of periodontal disease, and the exposure is current oral hygiene practices such as frequency of brushing and use of dental floss. This study can be carried out by interviewing participants about their oral hygiene habits and at the same time by assessing periodontal status clinically. Thus, outcomes and exposure data are assessed at the same time.
Cross-sectional studies measure prevalence and therefore are suitable for examining the burden of the disease or condition and are useful for health care services planning, as I discussed previously. A cross-sectional study recording the prevalence of caries in adolescents can provide useful information for determining caries prevention plans.
Analytical cross-sectional studies provide only weak evidence between exposures and outcomes, since it is difficult to separate the cause and effect. For example, in the previous scenario, it is difficult to determine whether periodontal disease preceded or followed the exposure (oral hygiene practice). In fact, an important issue is what is called reverse causality, which in this example could mean that patients who learned that they have periodontal disease might be more diligent with oral hygiene, thus creating an overestimate of the prevalence of periodontal disease among participants with good oral hygiene habits.
Bias in cross-sectional studies
Selection bias occurs when the study participants are systematically different in their characteristics compared with eligible participants who were not selected for the study. Additionally, when the exposed and unexposed groups have differences in important outcome predictors, the results might be biased.
In the periodontal disease study, selection bias can be introduced if the selection of patients was restricted to a group with higher or lower susceptibility for developing periodontal disease and, additionally, if the exposed and unexposed groups differ in ways that predict the outcome. A common type of selection bias is called nonresponse bias and is usually encountered when recruiting is conducted with mailed questionnaires.
When sampling from the study population, ideally random sampling should be implemented because it gives the same probability for each person to be included in the study and thus ensures that the drawn sample represents the study population. Several sampling methods are available, such as simple random sampling, systematic sampling, stratified sampling, and multi-stage sampling.
Since information on exposure and outcome is recorded simultaneously, prior knowledge of the condition might influence the ascertainment of the exposure or the outcome. Both recall and detection biases are likely. For example, if the investigators know the exposure status of the participants, they can be influenced in their decision on correctly classifying the outcome.
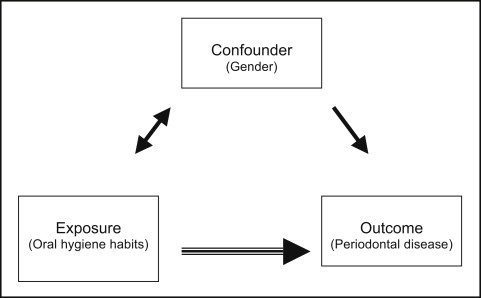
Finally, confounding is an important issue in cross-sectional studies. As explained previously, confounding can confuse the association between an exposure and an outcome. I will use the example study to indicate how confounding can result in incorrect associations. Figure 1 indicates that sex is a potential confounder of the association between oral hygiene and periodontal disease. Let me explain the thought process. Let’s say that female participants are associated with better oral hygiene practices. Let us also assume that women are more likely than men to experience periodontal disease because of a genetic predisposition (sex is an independent risk factor for periodontal disease). Because of the association of sex with exposure, since sex is an independent outcome predictor and not in the causal pathway between the exposure and the outcome (sex is not the result of the exposure), then all conditions are satisfied for sex to be a potential confounder of the association between oral hygiene practices and periodontal disease. Imagine that you have an unequal distribution of female and male subjects in the exposed and unexposed groups. Having more women than men in the unexposed group will tend to overestimate the association ( Fig 2 ), whereas having more men than women in the exposed group will tend to underestimate the association.