Crohn’s disease is a chronic inflammation of the small intestine; it can involve other organs, such as the skin, eyes, lungs, and joints. Oral manifestations are common, especially ulcers and stomatitis, which macroscopically and histologically resemble those found in the gastrointestinal tract. However, orthodontic alterations are not yet known. This article reviews aspects related to the diagnosis of Crohn’s disease and clinical considerations for an orthodontic patient.
Crohn’s disease is a chronic inflammation of the small intestine, and it can involve other organs, such as the skin, eyes, lungs, and joints. Men and women are equally affected, and joint involvement is the most common manifestation of extraintestinal impairment, affecting 20% to 30% of patients. The etiology of this disease is unknown but is thought to be the result of hyperactivity of the digestive immune system. Diagnosis is based on clinical, endoscopic, radiologic, and histopathologic findings.
Oral manifestations are common in Crohn’ disease, represented mainly by ulcers and stomatitis, which macroscopically and histologically resemble those found in the gastrointestinal tract. Development and exacerbation of periodontal disease have also been associated with Crohn’s disease. However, no reports were found in the literature addressing patients with Crohn’s disease in need of orthodontic treatment. Thus, the aim of this article was to discuss aspects related to diagnosis and clinical decision making regarding the treatment of an orthodontic patient with Crohn’s disease.
Case report
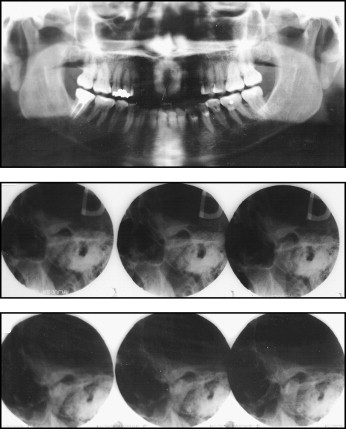
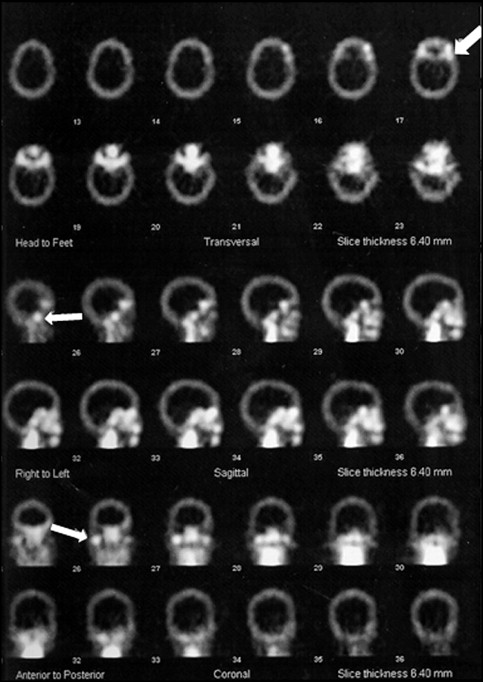
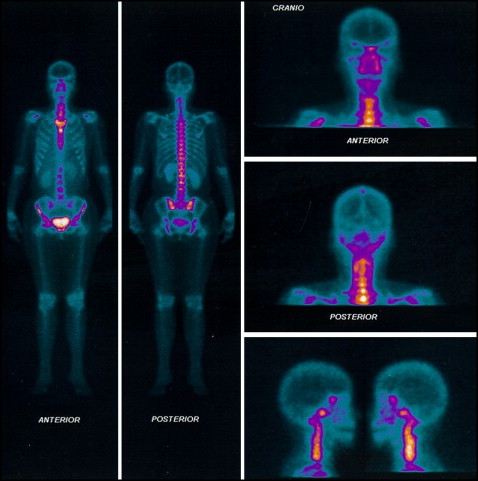
A 43-year-old woman sought orthodontic treatment to correct an open bite. The clinical examination showed an Angle Class I malocclusion with anterior open bite (3 mm), moderate crowding in both arches, lingual interposition, slight gingival retractions, and gingivitis in the region of the mandibular teeth ( Fig 1 ). Clicking and crepitation in the temporomandibular joint (TMJ) were also observed. The patient reported experiencing pain in the TMJ and other joints, such as those in the fingers. She reported that the oral lesions or ulcerations were constant in frequency and caused her considerable discomfort. Furthermore, she acknowledged that she was hesitant about having any type of orthodontic treatment, since the appliances might worsen the oral ulceration problem. The patient had been diagnosed with Crohn’s disease and also reported using anti-inflammatory medications. The cranial and panoramic radiographic evaluations showed abnormalities in the shape of the mandibular condyles ( Fig 2 ). Therefore, the patient underwent triphasic bone scintigraphy with the biodistribution of methyl diphosphonate tagged with technetium (MDP-Tc99m) for the assessment of the involvement of other joints. The examination showed that no joints other than the TMJ were compromised ( Fig 3 ). Static and single photon emission computed tomography images were also obtained; they showed an accentuated increased uptake in the right condyle and a moderately increased uptake in the left condyle, indicating intensive osteoblastic activity in the TMJ ( Fig 4 ). After we analyzed the clinical data and diagnostic examination, the diagnostic hypothesis was a degenerative process of the TMJ associated with Crohn’s disease. The patient was referred to an audiologist and a specialist in TMJ disorders. After advanced joint imaging, a diagnostic decision was made to forego orthodontic treatment.

Discussion
There has been an increase in the incidence of Crohn’s disease, making it a public health problem. The absence of information on the orthodontic management of patients with Crohn’s disease is a potential problem in the clinical practices of orthodontists. Because joints are affected in approximately 30% of patients, it is plausible that the clinical manifestations of the disease are reflected in the TMJ. Thus, a detailed clinical evaluation and patient history are valuable tools for orthodontists so that they can identify patients affected by Crohn’s disease. Inexplicable stomach pain and diarrhea are the first symptoms described. Fever also occurs irregularly, and affected persons complain of weight loss and loss of appetite. The inexplicable symptoms that often occur do not directly indicate Crohn’s disease, and years might pass before a physician makes the correct diagnosis. Crohn’s disease tends to occur more frequently in the same family. As many as 20% of patients have a first-degree relative (parent, sibling, cousin, or other close relative) who is also affected.
Joint impairment is categorized as inflammatory arthritis (rheumatic inflammation of the joints), with an association between the antigen HLA-B27 and human leukocytes. Anti-inflammatory drugs are administered beginning with the first signs of onset and continued through remission of the disease. Corticosteroid (prednisolone and methylprednisolone) drugs are important in the treatment of Crohn’s disease. Orthodontists should be aware of this, because such medications might influence the biology of dental movement, thereby representing a further limiting factor to orthodontic treatment. Currently, infliximab, a chimeric immunoglobulin G1 monoclonal antibody to tumor necrosis factor, dramatically improved the treatment of patients with Crohn’s disease and ulcerative colitis. Infliximab has achieved treatment goals such as mucosal healing and decreasing the need for hospitalizations and surgeries.
Oral lesions in those with Crohn’s disease are generally associated with low serum levels of iron because of the loss or reduced absorption of vitamins and trace elements as a result of diarrhea. It has also been suggested that local immunologic reactions to oral antigens can occur. Since oral lesions frequently occur in people with Crohn’s disease, orthodontists should be cautious with the technical details involved in the selection and adjustment of appliances. In the case described here, the patient was unmotivated with regard to orthodontic treatment and concerned that the orthodontic appliances would increase the frequency and occurrence of oral ulcerations.
After the multidisciplinary evaluation of this patient, the decision was made to forego any orthodontic treatment. This decision was based on the physical limitations posed by the patient. Considerable orthodontic movement with fixed appliances would have been necessary, and this might have aggravated the existing TMJ problems and the oral ulcerations. Moreover, the complexity of her malocclusion was limited and, according to the patient, had been present since adolescence.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


