Like many specialized organs in the head and neck region, the tongue is perhaps the most critical in terms of function, thus making its loss as a result of disease central to functional reconstruction and optimal speech and swallowing rehabilitation.
The tongue is enveloped by mucosa that contains mucous and serous glands, special taste sensory end-organs, and general sensory end-organs. Anatomically, it is composed of extrinsic and intrinsic muscles, all of which are paramount in its ability to perform the complex synchronized movements needed for speech articulation, manipulation of food boluses, and deglutition. There are four paired extrinsic tongue muscles: the genioglossus, hyoglossus, palatoglossus, and styloglossus. The intrinsic muscles consist of an ill-defined network of fiber bundles. The nerve supply is derived from four cranial nerves, the hypoglossal, vagus, lingual, and glossopharyngeal nerves. It is obvious from this anatomy that the specialized tissues in the tongue that control its complex motor and sensory activity make it a far more difficult structure to duplicate than the less specialized and adynamic tissues surrounding it, including the floor of the mouth, cheek, and mandible.
Contemporary tongue reconstruction is now considered to involve more than satisfactory wound healing and flap survival. The complex neuromuscular coordination involved in speech and deglutition is increasingly understood, and impairment in any of these components can result in dysphagia, aspiration, or poorly comprehensible speech. It should be the goal of every reconstructive surgeon to restore function to as close as possible to the preoperative state, which will also translate into significant improvements in patients’ quality of life.
Pathologic Anatomy/Classification Of Defects
The tongue can arbitrarily be divided into the anterior two thirds, which is essentially the mobile tongue, and the posterior third and tongue base, which is the less mobile component. This division is defined by the circumvallate papillae. Furthermore, quantification of ablative defects based on the volume of tissue lost can be divided into longitudinal quarters. Such classification systems are important for uniform reporting of results and, to a lesser degree, for planning appropriate reconstruction. Although division of the tongue in this fashion is useful for descriptive and classification purposes, denervation of the remnant tongue is more important than the volume of tongue resected with respect to ultimate functional outcome.
Ablative defects consisting of less than half the tongue are generally referred to as partial glossectomy defects. Hemiglossectomy results from resection of half the tongue, whereas resections of more than half or all of the tongue are referred to as subtotal or total glossectomy defects. Defining defect volume as just described allows the surgeon to anticipate the type of reconstruction necessary in each instance.
Treatment/Reconstructive Goals
The aims of tongue reconstruction are to achieve wound closure or coverage while minimizing complications and optimizing articulation and deglutition. Although primary wound closure and avoidance of wound complications were major concerns historically for most degrees of tongue defects, contemporary reconstructive surgery rarely fails to attain these basic objectives. However, restoration of optimal articulation and deglutition remain serious challenges for all reconstructive surgeons.
Furthermore, many studies have now confirmed that good functional reconstruction of the tongue provides significant objective and subjective improvements in quality of life.
Despite the method of reconstruction, the ability of the patient to articulate intelligibly and swallow is directly proportional to the amount of tongue resected. Important differences exist in instances in which primary closure as opposed to flap repair is used for tongue reconstruction. Flap tissue, though necessary for large defects, has demonstrably inferior outcomes in terms of speech and swallowing. This is probably a result of the introduction of adynamic bulky flap tissue, which somewhat impairs the function of the remaining tongue. Hence, it is preferable when possible to close partial glossectomy defects primarily.
For larger defects in which primary closure is not possible, it is critical to restore bulk to the tongue and, most importantly, preserve mobility of the remaining tongue. If possible, restoration of sensation to the flap, though variable, may help facilitate speech and swallowing rehabilitation.
Preservation of tongue mobility in patients with large defects in which adjacent tissues such as the floor of the mouth, mandible, and retromolar trigone are also involved can be achieved by independent reconstruction of these units with respect to the tongue defect.
The importance of replacement of tissue volume is of greater concern for subtotal and total glossectomy defects, with or without involvement of the tongue base. In such instances, sufficient tongue bulk in the midline is helpful in directing food and liquids toward the piriform sinuses. The critical role of the tongue base in swallowing is two-fold. The first piston-like action drives the food bolus through the oropharynx and creates positive pressure in the upper pharynx. This requires a competent palate and pharyngeal constrictor muscles and an adequate dynamic tongue base. It becomes apparent in extensive resections involving these additional structures that patients frequently fail to regain swallowing ability and remain dependent on percutaneous gastrostomy tubes for nutrition. The second pump is created by elevation of the larynx and opening of the piriformis, which causes negative pressure and suction action in the hypopharynx.
Finally, a controversial yet important consideration in reconstruction of large tongue defects is restoration of sensation. Kapur and colleagues in 1990 demonstrated the detrimental effects of regional oral anesthesia on mastication. Hence, the use of sensate flaps for reconstruction of the oral tongue may improve manipulation of the food bolus; however, the adynamic nature of flap tissue may offset this benefit. Restoration of sensation at the tongue base has not conclusively been shown to improve the swallowing reflex.
Treatment/Reconstructive Goals
The aims of tongue reconstruction are to achieve wound closure or coverage while minimizing complications and optimizing articulation and deglutition. Although primary wound closure and avoidance of wound complications were major concerns historically for most degrees of tongue defects, contemporary reconstructive surgery rarely fails to attain these basic objectives. However, restoration of optimal articulation and deglutition remain serious challenges for all reconstructive surgeons.
Furthermore, many studies have now confirmed that good functional reconstruction of the tongue provides significant objective and subjective improvements in quality of life.
Despite the method of reconstruction, the ability of the patient to articulate intelligibly and swallow is directly proportional to the amount of tongue resected. Important differences exist in instances in which primary closure as opposed to flap repair is used for tongue reconstruction. Flap tissue, though necessary for large defects, has demonstrably inferior outcomes in terms of speech and swallowing. This is probably a result of the introduction of adynamic bulky flap tissue, which somewhat impairs the function of the remaining tongue. Hence, it is preferable when possible to close partial glossectomy defects primarily.
For larger defects in which primary closure is not possible, it is critical to restore bulk to the tongue and, most importantly, preserve mobility of the remaining tongue. If possible, restoration of sensation to the flap, though variable, may help facilitate speech and swallowing rehabilitation.
Preservation of tongue mobility in patients with large defects in which adjacent tissues such as the floor of the mouth, mandible, and retromolar trigone are also involved can be achieved by independent reconstruction of these units with respect to the tongue defect.
The importance of replacement of tissue volume is of greater concern for subtotal and total glossectomy defects, with or without involvement of the tongue base. In such instances, sufficient tongue bulk in the midline is helpful in directing food and liquids toward the piriform sinuses. The critical role of the tongue base in swallowing is two-fold. The first piston-like action drives the food bolus through the oropharynx and creates positive pressure in the upper pharynx. This requires a competent palate and pharyngeal constrictor muscles and an adequate dynamic tongue base. It becomes apparent in extensive resections involving these additional structures that patients frequently fail to regain swallowing ability and remain dependent on percutaneous gastrostomy tubes for nutrition. The second pump is created by elevation of the larynx and opening of the piriformis, which causes negative pressure and suction action in the hypopharynx.
Finally, a controversial yet important consideration in reconstruction of large tongue defects is restoration of sensation. Kapur and colleagues in 1990 demonstrated the detrimental effects of regional oral anesthesia on mastication. Hence, the use of sensate flaps for reconstruction of the oral tongue may improve manipulation of the food bolus; however, the adynamic nature of flap tissue may offset this benefit. Restoration of sensation at the tongue base has not conclusively been shown to improve the swallowing reflex.
Reconstructive Techniques
Partial Glossectomy Defects
Facial Artery Musculomucosal Flap/Buccinator Flap
The buccinator flap, first described by Bozola and co-authors in 1989, and the facial artery musculomucosal (FAMM) flap, described by Pribaz in 1992, are useful intraoral pedicled axial-pattern musculomucosal flaps. The buccinator flap is based on the buccal artery, a terminal branch of the internal maxillary artery, whereas the FAMM flap is based on the facial artery. Both flaps provide excellent, reliable, and easily accessible reconstructive options for moderate-sized tongue defects. They have a rich vascular supply with a relatively constant anatomic course. Their mucosal nature provides a better surface for relining tongue defects than skin flaps do. Both flaps are easy to raise and their donor sites can be closed primarily with minimal morbidity.
Their limitations include a restricted arc of rotation and the necessity of remaining pedicled for 3 weeks before division of the pedicle, which invariably requires a second procedure.
Submental Artery Island Flap
The submental artery island flap ( Fig. 62-1 ) was first described by Martin and colleagues in 1992. Since then, many other reports in the literature have confirmed its versatile use in head and neck reconstruction, and it is an excellent option for reconstruction of partial glossectomy defects. Its advantages include reasonable flap thickness, tissue pliability, and versatility in design. Its close proximity to the tongue makes it an excellent choice for pedicled flap reconstruction, and the location of the donor site is cosmetically pleasing and frequently allows primary closure. Interestingly, Martin also described its use as a free flap.

The submental artery is a well-defined and consistent branch of the facial artery; it arises deep to the submandibular gland, passes forward and medially across the mylohyoid muscle, either superficial or deep to the digastric muscle, and terminates behind the mandibular symphysis over the anterior belly of the digastric. Along its course, the submental artery gives off several cutaneous branches that pierce the platysma to supply a broad cutaneous distribution of the upper ipsilateral neck extending to the contralateral neck. This allows a large flap to be raised from mandibular angle to mandibular angle, with width being limited by the flaccidity of neck skin in allowing direct closure. Its broad arc of rotation enables easy transfer into tongue defects.
The patient is positioned with the neck extended and the skin flap outlined in the midline submental region. Maximum flap width is determined by a pinch test to allow primary closure. The flap is raised in a distal to proximal direction in the subplatysmal plane, superficial to the contralateral anterior belly of the digastric, but deep to the ipsilateral digastric and superficial to the mylohyoid muscle. Inclusion of the digastric muscle adds a margin of safety to the vascularity of the skin island. The flap is separated from the submandibular gland until the facial vessels become apparent, and the facial pedicle is dissected proximally until adequate pedicle length is achieved. The marginal mandibular branch of the facial nerve, as well as the venous drainage, should be identified and preserved. The isolated flap is now tunneled between the mylohyoid muscle into the oral cavity for inset into the tongue defect.
Hemiglossectomy Defects
Fasciocutaneous Radial Forearm Free Flap
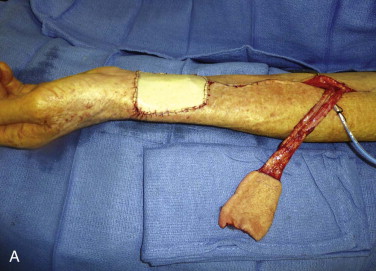
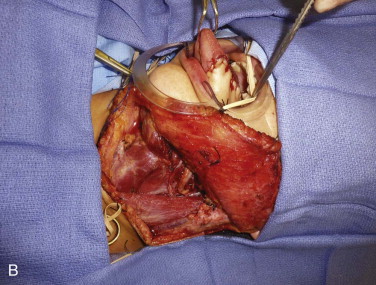
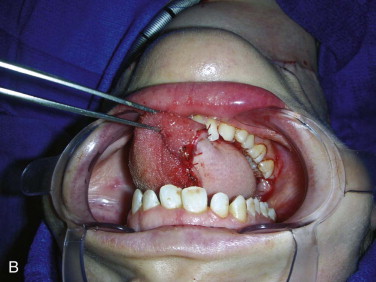
The radial forearm free flap ( Fig. 62-2 ) continues to find widespread use for the reconstruction of substantial glossectomy defects. Since its initial description in 1978 in the Chinese literature and later more comprehensively by Yang and associates in 1981 and Song and co-workers in 1982, this flap remains the workhorse flap for a variety of head and neck defects.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses