Periodontitis is an inflammatory disease of bacterial origin that results in the progressive destruction of the tissues that support the teeth, specifically the gingiva, periodontal ligament, and alveolar bone. The diagnosis of periodontal disease currently relies almost exclusively on clinical parameters and traditional dental radiography. In this article, the authors review current diagnostic techniques and present new approaches and technologies that are being developed to improve assessment of this common condition.
The challenges of periodontal diagnosis
Periodontitis is an inflammatory disease of bacterial origin that results in the progressive destruction of the tissues that support the teeth, specifically the gingiva, periodontal ligament, and alveolar bone. Although there have been significant advances in the understanding of the cause and pathogenesis of periodontal disease over the past 40 years, the traditional methods by which clinicians diagnose periodontal disease have remained virtually unchanged. The diagnosis of periodontal disease relies almost exclusively on clinical parameters and traditional dental radiography. Clinicians use clinical and radiographic findings to diagnose patients according to the classification scheme developed at the 1999 International Workshop for the Classification of Periodontal Diseases and Conditions ( Table 1 ). These traditional diagnostic tools have some significant shortcomings. Clinical assessments such as probing depth (PD) and clinical attachment level (CAL) are somewhat subjective and time consuming and therefore underutilized in general dental practice. Studies of the progression of periodontitis have demonstrated that there are periods of active tissue destruction separated by periods of inactive disease; however, traditional clinical assessments do not enable a practitioner performing a single routine periodontal examination to determine whether active tissue destruction is occurring. There are, for example, no definitive means of determining whether gingival inflammation in a successfully treated case of periodontitis represents early recurrent disease or gingivitis on a stable but reduced periodontium. Demonstrating progressive loss of periodontal support requires longitudinal assessment. Current diagnostic methodologies do not enable us to accurately predict which periodontal sites, teeth, or individuals are susceptible to further periodontal breakdown. Given the limitations of current diagnostic tools, researchers are working to develop techniques that address some of these inadequacies. In this article, the authors review the diagnostic techniques currently used and present new approaches and technologies that are being developed to improve the diagnosis of periodontal disease.
| I. Gingival Diseases | A. Plaque-associated gingival diseases Non–plaque-induced gingival diseases |
| II. Chronic Periodontitis | B. Localized Generalized |
| III. Aggressive Periodontitis | C. Localized Generalized |
| IV. Periodontitis as a Manifestation of Systemic Disease | D. Associated with hematologic disorders Associated with genetic disorders Not otherwise specified |
| V. Necrotizing Periodontal Diseases | E. Necrotizing ulcerative gingivitis Necrotizing ulcerative periodontitis |
| VI. Abscesses of the Periodontium | F. Gingival abscess Periodontal abscess Pericoronal abscess |
| VII. Periodontitis Associated with Endodontic Lesions | G. Combined periodontic-endodontic lesions |
| VIII. Developmental or Acquired Deformities and Conditions | H. Localized tooth-related factors that modify or predispose Mucogingival deformities and conditions around teeth Mucogingival deformities and conditions on edentulous ridges Occlusal trauma |
Current diagnostic strategies
In response to pathogenic bacteria in dental plaque (a biofilm adherent to the tooth surface), an innate inflammatory response as well as cellular and humoral immune responses are mounted locally in the periodontal tissues. The complex host response is aimed at containing the infectious stimulus and preventing bacterial invasion into the tissues. If the infection cannot be contained, the local release of proinflammatory cytokines and tissue degrading enzymes results in damage to the supporting hard and soft tissues of the tooth. The junctional epithelium becomes ulcerated and migrates apically, and there is destruction of the gingival connective tissue, periodontal ligament, and alveolar bone. Although pathogenic bacteria are capable of degrading host tissues, it is the host’s response to pathogenic bacteria rather than the bacteria themselves that is responsible for most of the tissue breakdown associated with periodontitis. The traditional diagnostic methods described in the following sections aim to identify the etiologic factors, assess the clinical signs of the inflammatory process, and determine the degree to which periodontal destruction has occurred.
Assessment of Etiologic Factors
Bacteria are necessary but insufficient by themselves to cause periodontal disease. It is generally accepted that even in the presence of pathogenic bacteria, individuals are variably susceptible to tissue breakdown. Identifying the presence of specific periodontal pathogens in dental plaque is not currently a strategy used to establish a periodontal diagnosis. Nonetheless, because bacteria are the initiating factor (and primary target of most of the present therapeutic modalities), it is important to assess the degree of bacterial plaque present and counsel patients on proper plaque control. It is also important to identify any factor that might make an individual susceptible to the accumulation of dental plaque. Some of these factors include a lack of manual dexterity associated with arthritis or other conditions, a reduced frequency of oral hygiene practices, improper technique, and tooth anatomy that promotes plaque retention.
Susceptibility to periodontitis is conferred by several established risk factors, such as diabetes mellitus and cigarette smoking. Certain genetic syndromes are also associated with periodontal disease. It is for these reasons that a thorough medical history, including a history of cigarette smoking, is an important part of establishing a periodontal diagnosis.
Assessment of Gingival Inflammation
Much information regarding the degree of gingival inflammation can be obtained from a simple visual inspection of the tissues. Healthy gingiva is typically pink and firm and has a knife-edged margin. Inflamed tissues exhibit cardinal signs of inflammation, such as redness and swelling ( Fig. 1 ). Bleeding on probing (BOP) is an important indicator of gingival inflammation within the periodontal pocket. It occurs because of microulcerations in the junctional epithelium. BOP is influenced by repeated probe insertions in a short time as well as by the use of excessive force (>25 N). Purulent exudate can also be an important sign of gingival inflammation; however, true suppuration may be difficult to distinguish from plaque that is expressed from the gingival crevice.

Calor, or heat, is another cardinal sign of inflammation and has been investigated as a diagnostic measure of periodontal status. Haffajee and colleagues used a periodontal temperature probe (Periotemp, ABIO-DENT, Inc, Danvers, MA, USA) to assess subgingival temperature and found that elevated mean subgingival temperature was related to subsequent attachment loss.
Assessment of Loss of Periodontal Attachment
PD assessment is probably the most commonly used clinical measure for detecting loss of periodontal support. It is measured from the free gingival margin (FGM) to the depth of the probable crevice. The depth of a healthy gingival sulcus ranges from 1 to 3 mm. PD is not the most objective measure of loss of periodontal tissues because the position of the FGM is variable. When there is gingival inflammation, the FGM may be located more coronal than normal because of edema in the tissues (the FGM is normally located 1.5–2 mm coronal to the cementoenamel junction [CEJ]). In this situation, there may be a deeper-than-normal PD even in the absence of loss of periodontal attachment. Such a deepened pocket is described as a pseudopocket. A true periodontal pocket occurs when there has been apical migration of the junctional epithelium and loss of supporting tissues of the tooth. The PD may also be normal in the presence of significant attachment loss. This may occur in the case of treated periodontitis or when the disease process manifests with gingival recession rather than pocket formation.
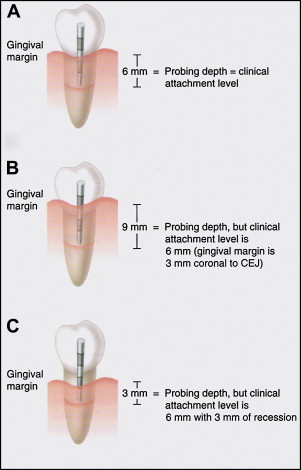
CAL is a more objective measure of loss of periodontal support because it is measured from a fixed point on the tooth, usually the CEJ, if detectable. CAL is defined as the distance between the CEJ and the base of the probable pocket ( Fig. 2 ). Because the apical termination of the junctional epithelium is normally located at the CEJ, there should be no CAL when the periodontal tissues are healthy and there is no history of periodontitis. When the gingival margin is located coronal to the CEJ, CAL is measured by subtracting the distance of the FGM to the CEJ from the PD (PD−[FGM−CEJ]). When there is gingival recession, CAL is calculated by adding the PD and the amount of recession. Calculating the CAL can be challenging, and this variable is more often used in research than in everyday clinical practice. Existing CAL also does not give any indication of current disease activity.
When interpreting the PD and CAL measurements made with conventional periodontal probes, it is important to consider that these values depend on the inflammatory state of the tissues. When probing healthy gingival tissues, the periodontal probe generally stops coronal to the apical extent of the junctional epithelium, which is at the CEJ. When the gingiva is inflamed and the gingival connective tissue has been infiltrated by inflammatory cells, there is less resistance to probe penetration and the periodontal probe generally passes apical to the level of the connective tissue attachment. As a result, PD and CAL values may be overestimated in inflamed sites and underestimated in healthy sites. The depth of probe penetration may also be influenced by factors such as the diameter of the probe tip, insertion force, and angulation of the probe. Electronic probes were developed to overcome some of these technical difficulties. Electronic probes, such as the Florida probe (Florida Probe Company, Gainesville, FL, USA), have the advantage of controlling insertion force, automatic data capture into a computer, and a higher resolution than manual probes. Electronic probes have the disadvantage of underestimating PD and CAL in untreated patients. Despite some acknowledged problems, manual probes are perfectly acceptable for routine periodontal examinations and provide results comparable to those with electronic probes.
Other clinical variables used to assess the degree of existing periodontal destruction include mobility and the degree of furcation involvement. Tooth mobility may be caused by several factors, but loss of periodontal attachment is one of the more common causes. Both mobility and furcation involvement are important determinants of a tooth’s prognosis.
Current diagnostic strategies
In response to pathogenic bacteria in dental plaque (a biofilm adherent to the tooth surface), an innate inflammatory response as well as cellular and humoral immune responses are mounted locally in the periodontal tissues. The complex host response is aimed at containing the infectious stimulus and preventing bacterial invasion into the tissues. If the infection cannot be contained, the local release of proinflammatory cytokines and tissue degrading enzymes results in damage to the supporting hard and soft tissues of the tooth. The junctional epithelium becomes ulcerated and migrates apically, and there is destruction of the gingival connective tissue, periodontal ligament, and alveolar bone. Although pathogenic bacteria are capable of degrading host tissues, it is the host’s response to pathogenic bacteria rather than the bacteria themselves that is responsible for most of the tissue breakdown associated with periodontitis. The traditional diagnostic methods described in the following sections aim to identify the etiologic factors, assess the clinical signs of the inflammatory process, and determine the degree to which periodontal destruction has occurred.
Assessment of Etiologic Factors
Bacteria are necessary but insufficient by themselves to cause periodontal disease. It is generally accepted that even in the presence of pathogenic bacteria, individuals are variably susceptible to tissue breakdown. Identifying the presence of specific periodontal pathogens in dental plaque is not currently a strategy used to establish a periodontal diagnosis. Nonetheless, because bacteria are the initiating factor (and primary target of most of the present therapeutic modalities), it is important to assess the degree of bacterial plaque present and counsel patients on proper plaque control. It is also important to identify any factor that might make an individual susceptible to the accumulation of dental plaque. Some of these factors include a lack of manual dexterity associated with arthritis or other conditions, a reduced frequency of oral hygiene practices, improper technique, and tooth anatomy that promotes plaque retention.
Susceptibility to periodontitis is conferred by several established risk factors, such as diabetes mellitus and cigarette smoking. Certain genetic syndromes are also associated with periodontal disease. It is for these reasons that a thorough medical history, including a history of cigarette smoking, is an important part of establishing a periodontal diagnosis.
Assessment of Gingival Inflammation
Much information regarding the degree of gingival inflammation can be obtained from a simple visual inspection of the tissues. Healthy gingiva is typically pink and firm and has a knife-edged margin. Inflamed tissues exhibit cardinal signs of inflammation, such as redness and swelling ( Fig. 1 ). Bleeding on probing (BOP) is an important indicator of gingival inflammation within the periodontal pocket. It occurs because of microulcerations in the junctional epithelium. BOP is influenced by repeated probe insertions in a short time as well as by the use of excessive force (>25 N). Purulent exudate can also be an important sign of gingival inflammation; however, true suppuration may be difficult to distinguish from plaque that is expressed from the gingival crevice.

Calor, or heat, is another cardinal sign of inflammation and has been investigated as a diagnostic measure of periodontal status. Haffajee and colleagues used a periodontal temperature probe (Periotemp, ABIO-DENT, Inc, Danvers, MA, USA) to assess subgingival temperature and found that elevated mean subgingival temperature was related to subsequent attachment loss.
Assessment of Loss of Periodontal Attachment
PD assessment is probably the most commonly used clinical measure for detecting loss of periodontal support. It is measured from the free gingival margin (FGM) to the depth of the probable crevice. The depth of a healthy gingival sulcus ranges from 1 to 3 mm. PD is not the most objective measure of loss of periodontal tissues because the position of the FGM is variable. When there is gingival inflammation, the FGM may be located more coronal than normal because of edema in the tissues (the FGM is normally located 1.5–2 mm coronal to the cementoenamel junction [CEJ]). In this situation, there may be a deeper-than-normal PD even in the absence of loss of periodontal attachment. Such a deepened pocket is described as a pseudopocket. A true periodontal pocket occurs when there has been apical migration of the junctional epithelium and loss of supporting tissues of the tooth. The PD may also be normal in the presence of significant attachment loss. This may occur in the case of treated periodontitis or when the disease process manifests with gingival recession rather than pocket formation.
CAL is a more objective measure of loss of periodontal support because it is measured from a fixed point on the tooth, usually the CEJ, if detectable. CAL is defined as the distance between the CEJ and the base of the probable pocket ( Fig. 2 ). Because the apical termination of the junctional epithelium is normally located at the CEJ, there should be no CAL when the periodontal tissues are healthy and there is no history of periodontitis. When the gingival margin is located coronal to the CEJ, CAL is measured by subtracting the distance of the FGM to the CEJ from the PD (PD−[FGM−CEJ]). When there is gingival recession, CAL is calculated by adding the PD and the amount of recession. Calculating the CAL can be challenging, and this variable is more often used in research than in everyday clinical practice. Existing CAL also does not give any indication of current disease activity.
When interpreting the PD and CAL measurements made with conventional periodontal probes, it is important to consider that these values depend on the inflammatory state of the tissues. When probing healthy gingival tissues, the periodontal probe generally stops coronal to the apical extent of the junctional epithelium, which is at the CEJ. When the gingiva is inflamed and the gingival connective tissue has been infiltrated by inflammatory cells, there is less resistance to probe penetration and the periodontal probe generally passes apical to the level of the connective tissue attachment. As a result, PD and CAL values may be overestimated in inflamed sites and underestimated in healthy sites. The depth of probe penetration may also be influenced by factors such as the diameter of the probe tip, insertion force, and angulation of the probe. Electronic probes were developed to overcome some of these technical difficulties. Electronic probes, such as the Florida probe (Florida Probe Company, Gainesville, FL, USA), have the advantage of controlling insertion force, automatic data capture into a computer, and a higher resolution than manual probes. Electronic probes have the disadvantage of underestimating PD and CAL in untreated patients. Despite some acknowledged problems, manual probes are perfectly acceptable for routine periodontal examinations and provide results comparable to those with electronic probes.
Other clinical variables used to assess the degree of existing periodontal destruction include mobility and the degree of furcation involvement. Tooth mobility may be caused by several factors, but loss of periodontal attachment is one of the more common causes. Both mobility and furcation involvement are important determinants of a tooth’s prognosis.
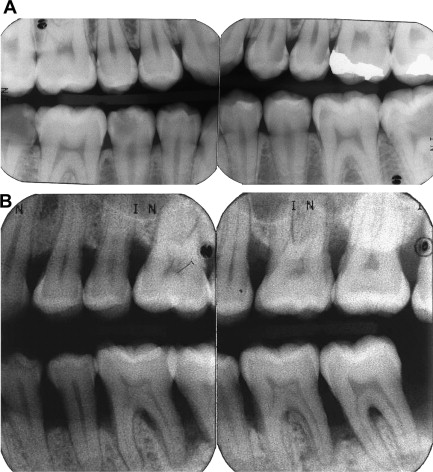
Radiographic assessment of periodontal disease
Radiographs are an essential component of the periodontal examination and indispensable in establishing a periodontal diagnosis. Important information regarding the position and architecture of the alveolar crest of bone is obtained from radiographs. Bite-wings are considered the most accurate intraoral radiographs for determining the height of the alveolar crest. In the absence of bone loss, the alveolar crest is generally located 1 to 2 mm apical to the CEJ ( Fig. 3 A). Vertical bite-wings may need to be taken to visualize the osseous crest in a patient with attachment loss ( Fig. 3 B). Periapical radiographs give the clinician important information regarding crown to root ratio, the periodontal ligament space, and the presence of periapical abnormality. Intraoral radiographs are generally considered preferable to panoramic radiographs for use in periodontal assessment; however, some studies have demonstrated that panoramic radiographs can be used to assess alveolar bone height.