Trauma to the mandible often causes condylar fracture. This article reports the conservative treatment of a 10-year-old girl with a unilateral condylar fracture, highlighting the diagnostic aspects involved and the strategy used. The conservative approach used for this patient—bionator followed by full fixed orthodontic appliances—provided adequate esthetic and functional results. The outcomes throughout the 7-year follow-up and the remodeling process of the condyle observed in the panoramic radiographs proved the success of this treatment.
The proportion of condylar fracture among all mandibular fractures ranges from 17.5% to 52%. Condylar fracture is probably the maxillofacial trauma with the most controversial opinions on the classification, diagnosis, and therapeutic management, which have raised discussions and arguments in the literature.
There are 2 types of fracture—intracapsular and extracapsular—yet for practical purposes, the anatomic level of the fracture is divided into 3 sites: condylar head (intracapsular), condylar neck (extracapsular), and the subcondylar region. Depending on the direction of the causal force, the position of the jaw at the time of the accident, the activity of the lateral pterygoid muscle, and the whole trauma to the mandible, the fractured part can remain in place, or can be partially or completely displaced. Usually, the displaced fragments are directed medially or anteromedially. According to Lindahl, condylar head displacement is more frequent in children.
The principal causes of condylar fractures in growing children vary according to age, with bicycle accidents the most common, especially in patients aged 6 to 12 years. The clinical consequences of condylar trauma directly depend on the child’s age at the moment of the lesion, growth potential, and extent of the fracture. Experimental studies and clinical observations have shown large adaptive changes in fractured condyles, as well as in contralateral condyles, that can cause functional disturbances and alterations in dentofacial growth. The consequences of these fractures on maxillofacial growth and occlusal development might be as severe as mandibular deficiency, asymmetry, retrusion, or ankylosis. It is known that there is a better potential for bone remodeling when fractures affect the higher regions of the mandible; a poor potential is noted in the lower regions, with luxation of the fragment and a greater tendency for facial asymmetry.
The treatment depends on the patient’s age, coexistence of other mandibular or maxillary fractures, whether the condylar fracture is unilateral or bilateral, the level and displacement of the fracture, the state of the dentition, and the dental occlusion. The treatment planning depends on the characteristics of each patient and the type of fracture, varying from conservative treatment comprising observation, analgesia, and a soft diet, to maxillomandibular fixation or functional appliance therapy, up to surgical intervention. In growing patients, with growth potential of the condyle, most authors recommend conservative therapy.
This report describes a pediatric patient with a unilateral condylar fracture who was treated conservatively with functional appliances. Satisfactory remodeling of the condylar process and possible repositioning of the temporomandibular fossa by apposition occurred, and normal occlusion and jaw movements were obtained.
Diagnosis and etiology
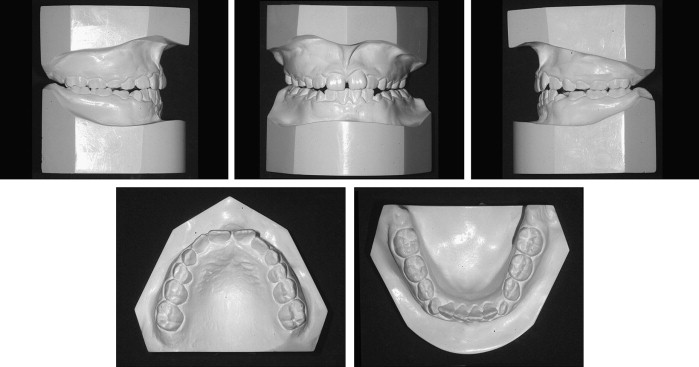
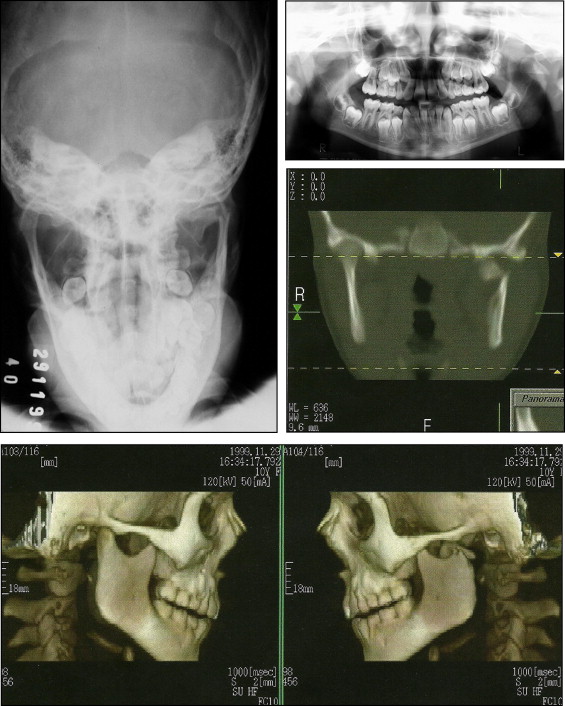
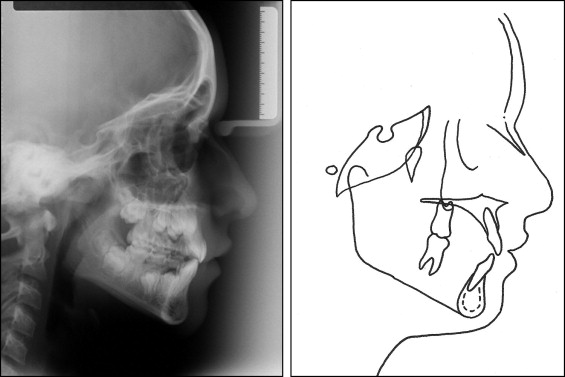
A 10-year-old girl received an orthodontic evaluation for a left condylar fracture resulting from a bicycle accident. The trauma had occurred 12 days earlier and was diagnosed in an emergency service at a hospital. The immediate therapy consisted of antibiotics, anti-inflammatory analgesic medications, a soft diet, and physiotherapy (open-close movements). Clinically, a mild midline shift on opening and occlusal contact on the fractured side were noted ( Fig 1 ). The patient showed a straight profile, facial asymmetry with a mandibular shift to the left side, and articular displacement during opening and closing. Analysis of her occlusion showed a Class I dental pattern and the mixed dentition period ( Fig 2 ). The maxillary incisor midline coincided with the facial midline, and the mandibular midline was shifted to the left by approximately 3 mm, with a functional crossbite on the left side. Overjet was 2 mm, and overbite was 0 mm. Panoramic and posteroanterior radiographs and 3-dimensional reconstructions with computed tomographs confirmed the transverse fracture of the neck of the left mandibular condyle at a 90° angle and medial displacement, without other alterations of the facial bone structures ( Fig 3 ). The cephalometric measurements are presented in Figure 4 and the Table .

| Measurement | Pretreatment | Posttreatment | 7 years posttreatment |
|---|---|---|---|
| SNA (°) | 77 | 78 | 78 |
| SNB (°) | 74 | 76 | 76 |
| ANB (°) | 3 | 2 | 2 |
| 1-NA (mm) | 4 | 6 | 6 |
| 1:NA (°) | 20 | 26 | 25 |
| 1-NB (mm) | 4 | 5 | 5 |
| 1:NB (°) | 27 | 34 | 31 |
| 1:1 (°) | 130 | 118 | 121 |
| Occl:SN (°) | 25 | 24 | 23 |
| GoGn.SN (°) | 34 | 34 | 34 |
| S-LS (mm) | 0 | 0 | −1 |
| S-LI (mm) | −1 | 2 | 2 |
| Y-axis to FH (°) | 61 | 60 | 61 |
| NPog.FH (°) | 86 | 87 | 86 |
| Angle of convexity (°) | 3 | 4 | 3 |
| Wits (mm) | −1 | −1 | −4 |
| FMA (°) | 28 | 28 | 27 |
| FMIA (°) | 58 | 53 | 55 |
| IMPA (°) | 94 | 99 | 98 |
| Nasolabial angle (°) | 102 | 108 | 110 |
| A-NPerp (mm) | −3 | −2 | −2 |
| Co-A (mm) | 80 | 82 | 82 |
| Co-Gn (mm) | 102 | 106 | 107 |
| AIFH (mm) | 63 | 66 | 67 |
| Pog-NPerp (mm) | −8 | −6 | −5 |
Treatment alternatives
According to international guidelines, the indications for nonsurgical treatment include condylar fracture in growing children ; thus, conservative orthodontic treatment was recommended. Since 12 days had already elapsed, maxillomandibular fixation was not indicated anymore. The initial treatment planning comprised placement of an orthopedic asymmetric bionator appliance, followed by full orthodontic treatment with fixed appliances to correct the asymmetry, maintain function, and prevent ankylosis.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


