This case report demonstrates the successful treatment of facial asymmetry with condylar hyperplasia with limited surgical and orthodontic treatment. A high condylectomy was performed to shorten the elongated condyle and to remove its active growth site. The maxillary molars on the affected side were then orthodontically intruded using temporary anchorage devices to improve the occlusal cant and posterior open bite of the unaffected side. This combined surgical-orthodontic treatment provided a satisfactory outcome without additional orthognathic surgery.
Highlights
- •
Facial asymmetry with condylar hyperplasia was successfully treated.
- •
A high condylectomy was performed to shorten the elongated condyle.
- •
Molar intrusion on the affected side improved occlusal cant and facial appearance.
- •
The surgical-orthodontic treatment provided a satisfactory and stable outcome.
- •
It also removed the necessity of additional orthognathic surgery.
Condylar hyperplasia is a developmental malformation characterized by excessive growth of the condyle. The unilateral enlargement of the condyle leads to facial asymmetry, mandibular deviation, malocclusion, and articular dysfunction. The hyperplastic condyle can be expanded to the condylar neck, the ramus, and even the mandibular body. Since the anomaly occurs during puberty and rarely begins after the age of 20, the maxilla usually follows mandibular downward growth as a physiologic response to the affected side. As a result, the occlusal plane tilts toward the affected side, whereas the teeth generally remain in occlusion.
Treatment is primarily surgical and can entail high condylectomy, orthognathic surgery, or both, according to the severity and the status of condylar growth. A high condylectomy is required to arrest active condylar growth. When the mandible grows rapidly, a posterior open bite can occur, indicating no need for maxillary surgery. However, bimaxillary surgery is generally necessary to correct both facial asymmetry and occlusal cant. Several reports have described orthognathic surgery or condylectomy as a treatment option for condylar hyperplasia.
Here, we report a case of combined surgical-orthodontic treatment without orthognathic surgery for a patient with facial asymmetry and condylar hyperplasia. Facial asymmetry and tilting of the occlusal plane was successfully treated orthodontically after a high condylectomy. The condylectomy contributed to improve the patient’s facial asymmetry, and intrusion of the maxillary molars on the affected side successfully corrected the tilted occlusal plane, resulting in a stable occlusal relationship without additional orthognathic surgery.
Diagnosis and etiology
A 26-year-old woman was referred from the Department of Oral and Maxillofacial Surgery of Yonsei University, Seoul, South Korea, for orthodontic treatment combined with future orthognathic surgery. Her chief complaint was facial asymmetry, which she first noticed at puberty. She reported that the condition had become progressively more severe since then. She had a history of surgery for gastric cancer at age 19 and reported that she had a keloid.
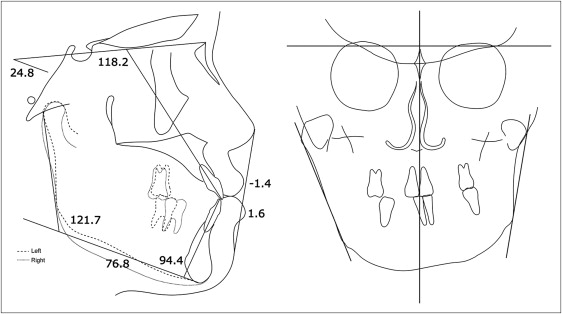
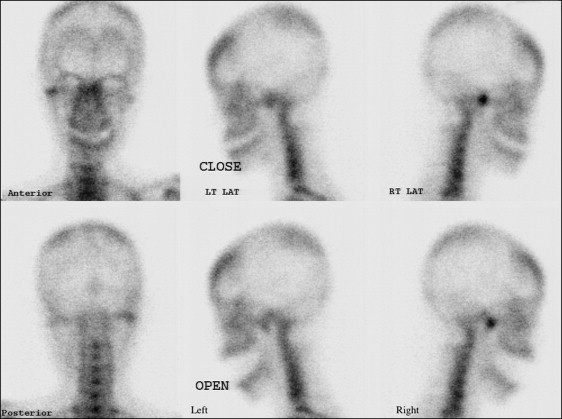
At the initial clinical examination, deviation of the chin to the left side was evident, and canting of the lip and maxillary occlusal plane was also observed ( Figs 1-4 ). The initial radiographic evaluations showed an asymmetric mandible with elongation of the right condyle ( Table I ). A whole body bone scan using Tc-99m hydroxydiphosphonate demonstrated an intense focal uptake in the right condyle, indicating active growth potential ( Fig 5 ). The condylar enlargement appeared to have caused rotation of the maxillomandibular complex to the left side, based on the significant differences in ramus lengths and the frontal ramal inclination, occlusal plane cant, and chin deviation. She reported intermittent clicking with discomfort on the left but not the right temporomandibular joint (TMJ), with no limitation in mouth opening.


| Condyle (mm) | Coronoid (mm) | Con/Cor | ||||
|---|---|---|---|---|---|---|
| Right | Left | Right | Left | Right | Left | |
| Preoperative | 53.84 | 39.42 | 35.63 | 39.23 | 1.511 | 1.005 |
| 6 mo postop | 35.29 | 39.35 | 38.19 | 37.21 | 0.924 | 1.058 |
| 1.5 y postop | 37.76 | 39.78 | 37.54 | 37.23 | 1.006 | 1.068 |
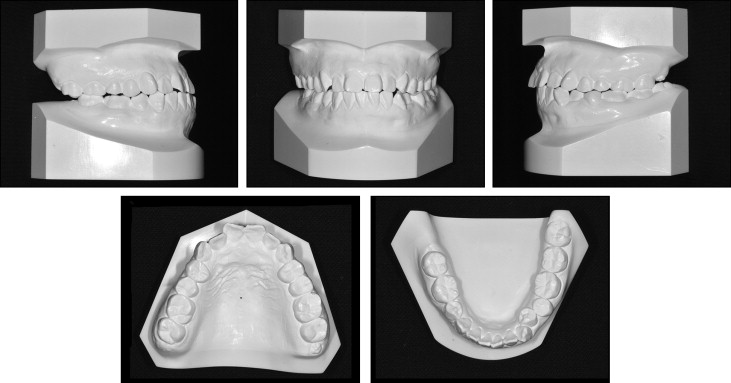
Cephalometric and model analysis showed that she had a skeletal Class III malocclusion (ANB angle, −2.8°) with a hypodivergent facial profile (mandibular plane angle, 25.2°) ( Table II , Fig 4 ). She had Class I canine and molar relationships on the left side, and Class I canine and Class III molar relationships on the right side, with a congenitally missing mandibular second premolar. Consequently, a slight extrusion of the maxillary right second molar, especially the palatal cusp, was observed. The mandibular dental midline was deviated 2.0 mm to the left side; this was smaller than the amount of skeletal discrepancy. Overjet and overbite were 1.3 and 1.0 mm, respectively.
| Variable | Norm | Pretreatment | 6 months after condylectomy | Posttreatment | 3.5 years of retention |
|---|---|---|---|---|---|
| SNA (°) | 81.6 | 83.3 | 83.2 | 83.4 | 83.4 |
| SNB (°) | 79.1 | 86.1 | 82.6 | 82.4 | 82.0 |
| ANB (°) | 2.5 | −2.8 | 0.6 | 1.0 | 1.3 |
| Wits appraisal (mm) | −2.8 | −6.2 | −1.5 | −2.7 | −2.1 |
| Björk sum (°) | 393.3 | 385.2 | 391.0 | 389.6 | 390.6 |
| SN-MP (°) | 34.0 | 24.8 | 31.1 | 29.8 | 30.7 |
| Facial height ratio | 66.0 | 75.2 | 69.8 | 71.0 | 69.9 |
| U1-SN (°) | 106.0 | 118.2 | 121.0 | 110.9 | 108.6 |
| IMPA (°) | 94.0 | 94.4 | 94.1 | 90.1 | 89.2 |
| Interincisal angle (°) | 126.0 | 126.0 | 114.5 | 130.2 | 131.5 |
| Upper lip to E-line (mm) | −1.0 | −1.4 | 1.7 | −1.1 | −0.7 |
| Lower lip to E-line (mm) | 1.0 | 1.6 | 4.2 | 0.4 | 0.7 |
On the basis of these findings, the patient was diagnosed as having facial asymmetry with condylar hyperplasia (possibly in an active state) and a skeletal Class III malocclusion with a missing mandibular right second premolar.
Treatment alternatives
Condylectomy was considered first because of the hot spot on the scintigram at the right condyle. Simultaneous or consecutive orthognathic surgery was also considered for correction of the dentofacial deformity and the malocclusion. Based on these surgical considerations, 3 treatment alternatives were discussed at the surgical-orthodontic conference.
The first option was to perform a condylectomy with simultaneous orthognathic surgery followed by orthodontic treatment. This option would require only 1 surgical procedure to obtain balanced occlusion, TMJs, and jaws in a short time. In addition, the surgery-first approach would reduce the duration of postoperative orthodontic treatment by accelerating tooth movements. However, the postoperative changes were difficult to predict accurately because the extent of TMJ remodeling could not be estimated precisely. Furthermore, the correction of facial asymmetry inevitably called for changes to the preoperative functional occlusion, which could then result in postoperative occlusal instability. Moreover, early mobilization for rehabilitation of the TMJs can be challenging for a patient undergoing the concomitant orthognathic surgery with maxillomandibular fixation, which might compromise the surgical outcome.
The second option was to perform the 2 surgical procedures at different times. After the condylectomy, the occlusion as well as the facial asymmetry might be changed significantly, creating a malocclusion with a posterior open bite. The occlusal, muscular, and TMJ changes would be expected to settle down to a quiescent phase after the remodeling period. This option would allow time to make a precise plan for the orthognathic surgery during the postcondylectomy orthodontic treatment. In addition, rehabilitation of the TMJ and the planning and execution of the orthognathic surgery would be easier if the 2 surgical procedures were performed separately. However, 2 procedures would burden the patient physically and economically, and she could suffer from significant occlusal discomfort between the surgeries.
The last option was a less invasive treatment approach that included the condylectomy and orthodontic camouflage treatment. The tilted maxillary occlusal plane would be corrected by molar intrusion using temporary anchorage devices (TADs). We hoped that this plan would eliminate the need for additional orthognathic surgery; if not, then we could still perform the orthognathic surgery. Minimizing the extent of surgery, early mobilization after the condylectomy, and molar intrusion of the affected side would enhance postoperative recovery in terms of occlusion and TMJ rehabilitation. On the other hand, ideal correction of the facial asymmetry would not be possible with this treatment option. Because clockwise rotation of the mandible would occur after the condylectomy, maxillary premolar extraction might be necessary.
These treatment alternatives were discussed with the patient. Because of her history of gastric cancer, she strongly desired limiting the number and extent of the surgeries. Condylectomy would arrest the active condylar growth, correct the facial asymmetry significantly, provide long-term stability, and remove the necessity of additional orthognathic surgery with postorthodontic treatment. Even though the treatment could take longer with this last option, it was more conservative and would provide circumstances in which the alveolus, which exhibits compensatory growth, could recover the original positioning via functional forces after the condylectomy. Therefore, we selected the last option and started to prepare the patient for treatment.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


