As dentists, we are often faced with the question: to close or not to close? Since maxillary lateral incisors are often congenitally missing, replacement of these teeth raises several important treatment planning concerns. Therefore, it is beneficial to use an interdisciplinary treatment approach to obtain the most predictable outcome. There are multiple treatment options for the replacement of congenitally missing lateral incisors, including canine substitution, single-tooth implants, and tooth-supported restorations.
Drs Zachrisson, Rosa, and Toreskog beautifully illustrated the benefits of canine substitution by presenting the advantages and disadvantages of space closure as well as the functional and esthetic limitations that accompany this treatment choice. Like our European colleagues, our team agrees with the underlying principle to develop treatment plans that are both conservative and functional while maintaining excellent esthetics. However, the esthetic and functional success of canine substitution ultimately depends on variables such as malocclusion, crowding, profile, crown shape and color, and smiling lip level. Also, the amount of crown reduction that is often required to appropriately position these teeth esthetically and functionally in 3 planes of space can be excessive. Therefore, the optimal canine substitution patient is one who has small canines with crowns that match the shade of the central incisors. Ideally, he or she should also have a nice profile, a Class II dental relationship, and no crowding in the mandibular arch. However, many patients do not meet these criteria, and multiple veneers often need to be placed on the anterior teeth to overcome the esthetic compromise that typically arises. Unfortunately, by doing this, we start to lose the conservative nature of the overall treatment. Even though veneers might be considered “conservative” and “ultrathin,” they are nonetheless restorations that will need to be maintained and replaced throughout the young patient’s life. It is our philosophy that for patients who do not meet the specific qualifications necessary to be considered optimal candidates for canine substitution, an alternative form of treatment must be considered.
Restorative treatment alternatives can be divided into 2 categories: a single-tooth implant and a tooth-supported restoration. The 3 types of tooth-supported restorations available today are a resin-bonded fixed partial denture (FPD), a cantilevered FPD, and a conventional full-coverage FPD. The primary consideration when deciding which option to choose is conservation of tooth structure. Ideally, the treatment of choice should be the least invasive option that satisfies the expected esthetic and functional objectives. Although any of the 3 restorative treatment options can be used to achieve predictable esthetics, function, and longevity, if a treatment option is used in the wrong patient, the final result might be less than ideal. Therefore, the orthodontist should know the final restorative treatment plan to position the adjacent teeth properly and facilitate the final restoration.
Implant-supported restorations
Today, the single-tooth implant has become the most popular treatment alternative for the replacement of missing teeth. Various studies have shown the successful osseointegration and long-term function of restorations supported by single-tooth implants. In addition to the high success rates, 1 main benefit of this type of restoration is that it leaves the adjacent teeth untouched. This is particularly important in young patients and unrestored dentitions. It is true that implant-supported restorations are not without potential problems. These problems range from mechanical complications to biologic changes that can impact their long-term predictability. However, if the proper surgical and restorative protocols are followed, potential complications or esthetic compromises are minimal. To achieve a stable esthetic and healthy outcome with dental implants, it is beneficial to understand their effects on the surrounding hard and soft tissues.
In addition to the high success rates, 1 main benefit of this type of restoration is that it leaves the adjacent teeth untouched. This is particularly important in young patients and unrestored dentitions.
Implant-site development
It is now recognized that implant size and position play important parts in achieving a stable, esthetic, and healthy outcome. After implant placement, dimensional changes in the surrounding crestal bone occur in both vertical and horizontal dimensions. If an implant is to be used to replace a missing lateral incisor, the thickness of the alveolus must be adequate to allow for proper implant placement. Without the development and eruption of the permanent lateral incisor, the osseous ridge in this area is typically deficient. If the permanent canine is allowed to erupt mesially through the alveolus into the lateral incisor position, its large buccolingual width will influence the thickness of the edentulous ridge. Then, after the permanent canine is orthodontically moved distally, an increased buccolingual alveolar width is established. Studies have shown that, if a lateral incisor implant site is developed by this orthodontic tooth movement, its buccolingual dimension remains stable over time. This is especially beneficial, since an implant cannot be placed until facial growth is complete.
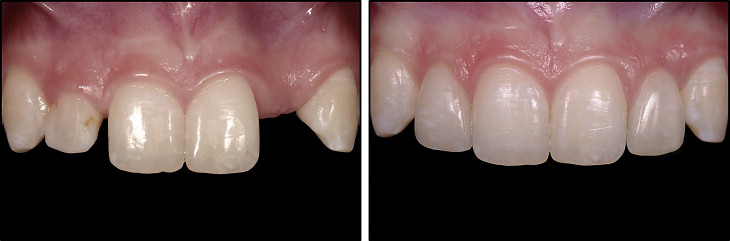
If the alveolar ridge is not developed through guided orthodontic eruption of the canine into the lateral site, then the edentulous site will typically be deficient in the orofacial dimension. Positioning dental implants in a narrow ridge requires deeper placement to prevent a bony dehiscence and also results in a thin layer of bone on the facial aspect, both of which will have a negative impact on the surrounding soft tissues. Establishment of the biologic width or bone remodeling of the thin buccal bone will inevitably lead to show-through of both the implant body and the abutment, resulting in an unesthetic cyanotic color of the soft tissue, gingival recession, and abutment exposure. Esthetic assessments have noted that, for an optimal outcome, the facial contour should mimic that of a natural tooth root eminence and have a similar soft-tissue color and texture. Therefore, alveolar ridge augmentation for both implant support and for what has been referred to as “contour augmentation” is necessary to provide a stable overlying esthetic soft-tissue framework for the implant restoration. If this is not performed, although the implant might be integrated, the esthetic result could be less than ideal. Although darkening of the soft tissues around implants can also be caused by the abutment and crown “shadowing” the gingiva, this effect is minimized with today’s restorative materials. With the new advances in abutments and material selections, customized zirconia implant abutments with all-ceramic restorations can be used in the anterior to allow more light reflection and transmission compared with metal. So, even if the tissue position around implants changes over time, the esthetic impact would be minimal ( Figure 1 ).
To determine the appropriate size of the implant to be used, it is important to evaluate the width of the edentulous space that is created. The deleterious effect of bone remodeling in the proximal region beside a dental implant mentioned by Zachrisson et al has been observed as a loss of periodontal attachment on the adjacent tooth. It is known that the loss of the supporting bone is worse if the implant-to-tooth distance is less than 1.5 mm. This results in apical migration of the papillary tissue, leading to open gingival embrasures and lack of gingival scallop. Mesiodistally, most lateral incisor sites will be between 5 and 7 mm. Historically, because of the lack of options regarding implant sizes, the use of standard diameter 3.75- to 4.0-mm implants was common in implant therapy. This compromise in proximal implant positioning led to unfavorable esthetic outcomes. Today, the use of implants with a narrow diameter or a platform switch design has been shown to have a positive effect on the amount of bone remodeling typically noted with standard implants. In addition, normal papillary dimensions can predictably be achieved with proper surgical management, since papillary support is a result of the periodontal attachment on the adjacent teeth. Our colleagues made a strong attempt to outline the negative esthetic and biologic outcomes of dental implants. However, it is clear that the current knowledge regarding dimensional changes after implant placement can help to avoid these historically noted unfavorable results.
After the appropriate amount of coronal space has been determined, it is necessary to evaluate the interradicular spacing. Inadequate space between the root apices is generally due to improper root angulation. Therefore, it is important to take a periapical radiograph of the edentulous area before removing the orthodontic appliances to confirm the ideal root position and adequate spacing for future implant placement. Implants, however, cannot be placed until facial growth is complete. Therefore, monitoring the eruption in these patients at an early age is important for optimal implant-site development.

Timing of implant placement
The appropriate time to place an implant is based on a patient’s facial growth. As the face grows and the mandibular rami lengthen, the teeth must erupt to remain in occlusion. Implants cannot erupt. If an implant is placed before a patient has completed his or her facial growth, significant periodontal, occlusal, and esthetic problems can be created. Thilander et al noted the development of infraocclusion of implant-supported restorations. The patients in that study were adolescents between 13 and 17 years of age when the dental implants were placed. Nearly all of the infraocclusion that was observed occurred during this period of growth. Historically, hand-wrist radiographs have been taken to assess growth. However, they do not predictably determine the completion of facial growth. The most predictable way to monitor facial growth is by evaluating serial cephalometric radiographs taken 6 months to 1 year apart. These radiographs, when superimposed, illustrate any changes in vertical facial height over the specific time period. If 2 sequential radiographs show no growth, then an implant can be placed, and significant eruption of the adjacent teeth will not be expected. Although changes in tooth position can occur throughout life, these changes both are multifactorial and show significant individual variation. Therefore, to help minimize the long-term impact, the orthodontic treatment should create good incisor stability to prevent continued eruption, long-term retention should be used at night, and the implants should be placed only after growth is complete. The timing for implant placement after the end of growth is generally about 20 to 21 years of age for men and 16 to 17 years of age for girls.
Interim tooth replacement after orthodontics
If implants cannot be placed until facial growth is complete, the edentulous space must be maintained after the orthodontic appliances are removed until the implant can be placed and restored. A removable retainer with a prosthetic tooth is an easy and efficient way to replace the missing tooth as well as to ensure postorthodontic retention. This type of retainer works well when the period of retention before implant placement is relatively short. If it will be years before growth is completed, it is possible to see the roots of the central incisor and canine converge toward each other during the retention phase, making future implant placement difficult or impossible. Therefore, a more appropriate choice might be a bonded fixed retainer. This could be as simple as a traditional lingual wire with a prosthetic tooth or as involved as a laboratory-fabricated resin-bonded FPD. Regardless of the choice, these long-term retainers are excellent for maintaining the final orthodontic position of the canine and the central incisor.
There are certain patients in whom it is not possible to place an implant. This could be because the patient does not want to undergo the necessary preprosthetic treatment of orthodontics and possible ridge augmentation to create an ideal implant site. However, there might also be instances when the appropriate interradicular spacing cannot be achieved through orthodontic treatment, even though the coronal spacing is ideal and the mesiodistal root angulation is acceptable as confirmed on a panoramic radiograph. In this situation, an alternate tooth-supported restorative option is required.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


