Introduction
The aims of this investigation were to evaluate associations between orthodontic space closure (including first premolar intrusion and canine extrusion for esthetic reasons) and periodontal tissue deterioration over a 10-year period in subjects with one or both missing maxillary lateral incisors and to investigate the occurrence of signs or symptoms of temporomandibular disorder (TMD).
Methods
This was a retrospective cohort study comprising patients treated by the same orthodontist. The agenesis group included 26 consecutive adolescent and young adult patients (9 male, 17 female) treated with space closure. The control group consisted of 32 orthodontic patients (12 male, 20 female) with no missing teeth and no need for extractions. In the agenesis group, full-mouth probing pocket depths and bleeding on probing were recorded at 6 locations for each of 657 teeth (3942 periodontal sites). In the control group, comparative data were collected for the maxillary first molars, premolars, canines, and lateral incisors, a total of 264 teeth (1584 periodontal sites). Mobility and gingival recession were also evaluated. Patients in both groups completed questionnaires concerning symptoms related to TMD.
Results
The full-mouth assessments in the agenesis group generally demonstrated periodontally healthy conditions, with probing depths below 4 mm and few bleeding sites. Some slight recessions were found, mostly on molars and second premolars, and there was normal mobility of first premolars that substituted for canines. Comparisons between the agenesis and control groups showed no statistically significant differences for the maxillary teeth regarding increased pocket depth (≥4 mm) or increased mobility. Interproximal sites in the agenesis group showed less bleeding on probing than in the control group; this was statistically significant. Anterior teeth in the agenesis group did not show any more recession than in the controls. In addition, we observed no difference in signs or symptoms between the 2 groups; this might be due to the limited sample size or the drawbacks of the surveys of TMD through subjects’ recall. Thus, the long-term periodontal tissue health and the incidence of dysfunction or TMD signs were similar in the space-closure agenesis group and in the control group of nonextraction orthodontic patients.
Conclusions
Orthodontic space closure including first premolar intrusion and canine extrusion in patients with missing lateral incisors does not incur risks for periodontal tissue deterioration or TMD in the long term.
Highlights
- •
We studied periodontal health after treatment for missing maxillary lateral incisors.
- •
Canine substitution was compared with a matched control group with no agenesis.
- •
No statistical differences between groups were found for periodontal health or temporomandibular disorder.
- •
The long-term periodontal status of intruded first premolars was good.
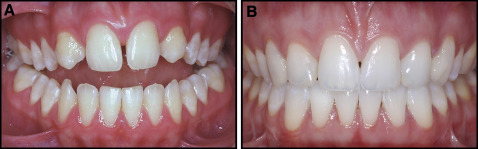
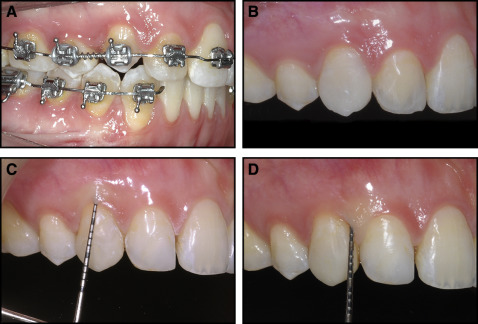
Patients with congenitally missing maxillary lateral incisors often need a challenging interdisciplinary treatment, whether canine substitution, single implants, or tooth-supported restorations are chosen. Ideally, each alternative should fulfill individual esthetic concerns, functional requirements, and periodontal tissue health, not only at the end of treatment but also in the long term. When space closure is selected, premolar intrusion and canine extrusion can remodel the gingival margins so that an optimal, natural-looking result can be achieved. This means that the labial gingival margin of the new canine (the intruded first premolar) will be at the same level as that of the central incisor, whereas that of the new lateral incisor (the extruded canine) will be about 2 mm lower ( Figs 1, B ; 2, A ; and 3, A ). These vertical movements will inevitably generate uneven vertical crestal bone septa, particularly in the first premolar-canine region ( Fig 4, A ).

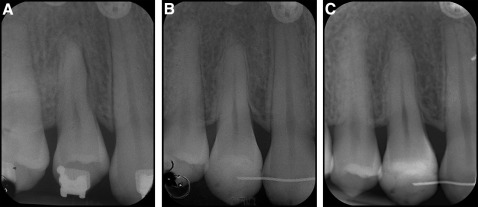
In adult patients with uncontrolled pathologic tooth movements, osseous vertical defects including interproximal craters and 1-, 2- or 3-wall defects may be found around mesially tipped teeth or teeth that have supraerupted. Vertical defects may compromise the patient’s ability to clean his or her teeth adequately and lead to attachment loss on the mesial and distal surfaces of the adjacent roots. If the crater is mild to moderate but the patient cannot maintain the area adequately, it may require resective bone removal and recontouring. However, the uneven vertical bone contours ( Fig 4, A ) in well-performed orthodontic space closure treatment (in which the teeth are aligned with proper angulation and inclination) may not be comparable. Also, the problem of maintaining adequate oral hygiene should be lower in young and healthy patients.
Another potential problem is that the intruded and restored first premolar might create later periodontal problems or might not be able to provide a proper functional occlusion, and therefore possibly predispose the patient to temporomandibular disorder (TMD).
The aims of this investigation were to assess, over a 10-year period, (1) periodontal tissue conditions of intruded first premolars and extruded canines in patients with congenitally missing maxillary lateral incisors compared with their full-mouth periodontal status, (2) periodontal tissue conditions of intruded first premolars and extruded canines in patients with congenitally missing maxillary lateral incisors compared with the corresponding teeth (considering the position) in orthodontic patients treated without extractions, and (3) the functional and occlusal statuses and eventual TMD in patients with congenitally missing maxillary lateral incisors who were treated with space closure, premolar intrusion, canine extrusion, and minimally invasive restorations, compared with a control group of orthodontic patients treated without extractions.
Material and methods
A retrospective cohort study was made of 2 groups of patients consecutively treated by the same orthodontist (M.R.), recruited from the files of his private office.
The inclusion criteria for the agenesis group (AG) were (1) agenesis of at least 1 maxillary lateral incisor, (2) treatment completed at least 60 months before follow-up, and (3) patients who were treated consecutively. Patients with cleft palate or syndromes were excluded.
All patients were consecutively treated by space closure to replace the missing lateral incisors. Full fixed appliances were used at the end of dental arch growth in the permanent dentition by the same clinician (M.R.). The clinical protocol was described previously by Rosa and Zachrisson. It combines first premolar intrusion and canine extrusion ( Figs 2, A ; 3, A ; and 4, A ) to achieve optimal leveling of the labial gingival margins. Minimally invasive supragingival restorations may provide proper esthetics and functions ( Figs 1, B ; 2, B ; and 3, B ). Buildups on the intruded premolars were made with porcelain veneers (4 patients) or composite resin (22 patients). A posttreatment occlusal equilibration was infrequently made to obtain optimal occlusal function. A 0.019-in multibraided stainless steel wire was bonded as a retainer in the maxillary arch, a 0.019-in multibraided stainless steel wire was bonded on the 6 front teeth and left in place for 24 months in 20 patients of the AG. In 6 patients, the bonded retainer was still in place at follow-up (0.0195-in Penta Twist retainer wire; Gold’n Braces, Palm Harbor, Fla).
Thirty-two consecutively treated patients were contacted by telephone and invited to participate in the study; 4 declined for private reasons, 1 had moved away from the area, and 1 could not participate for professional reasons. Thus, the final AG sample consisted of 26 patients (9 male, 17 female). The mean age at the end of orthodontic treatment was 23 years 7 months (SD, 10 years 7 months). The mean time after the completion of treatment was 9 years 9 months (SD, 4 years 2 months). The mean age at follow-up was 33 years 5 months (SD, 10 years 3 months). Nineteen patients had bilateral agenesis, and 7 had unilateral agenesis. Among those 7 subjects, 1 was treated with unilateral space closure, and the others were treated with bilateral space closure after extraction of the contralateral incisors. The total number of teeth analyzed in the AG was 657.
The inclusion criteria for the control group (CG) were (1) no congenitally missing maxillary teeth (except for third molars), (2) no need for extractions and less than 4 mm of crowding, (3) orthodontic treatment finished at least 60 months before follow-up, and (4) no fixed retention on the maxillary teeth at the follow-up. Patients with cleft palate or syndromes were excluded.
The CG consisted of 32 orthodontic patients (12 male, 20 female). The mean age at the end of orthodontic treatment was 17 years 7 months (SD, 5 years 6 months). The mean time after completion of treatment was 9 years 11 months (SD, 3 years 5 months). The mean age at follow-up was 27 years 6 months (SD, 6 years 11 months). The t test was applied regarding the age differences between the 2 groups, with a P value of 0.061.
The ratios between the male and female subjects were 35% to 65% in the AG and 38% to 62% in the CG.
The purposes of this investigation were to (1) assess the periodontal health of all maxillary and mandibular teeth in the AG by recording tissue data at 6 locations on each of the 657 teeth: mesiofacial, facial, distofacial, distolingual, lingual, and mesiolingual (3942 sites altogether); and (2) compare the periodontal status of the maxillary teeth that were moved mesially in the AG with the homologous data in the CG. The comparison sites were the central incisors in both groups, canines replacing lateral incisors in the AG compared with lateral incisors in the CG, first premolars replacing canines in the AG compared with canines in the CG, second premolars in the AG compared with first premolars in the CG, and first molars in both groups, for a total of 8 teeth and 48 sites for each subject (264 teeth, 1584 sites). Any additional data were inserted in the data set for the AG.
All interviews and clinical examinations were performed by 1 examiner (S.F.), who was not involved in the treatment.
Periodontal tissue examination included evaluations of probing pocket depth (distance from the free gingival margin to the bottom of the sulcus or periodontal pocket), bleeding on probing, plaque accumulation, gingival recession (distance between the free gingival margin and the cementoenamel junction), and mobility. Mobility was assessed according to a standard classification, indicating that increased mobility was more than that attributable to physiologic tooth movement (<0.2 mm). Mobility was recorded for all teeth. The mobility of the first premolars in the AG was also compared with that of the first premolars in the CG. This comparison was made to check whether the mobility of the first premolars in the canine position was different from the mobility of the first premolars in the normal position. Six patients of the AG still had a bonded retainer in place at the follow-up and were therefore excluded from the mobility tests. Thus, only 20 patients in the AG (40 first premolars) were considered in the statistical analysis and compared with the CG. Probing pocket depth, bleeding on probing, plaque accumulation, and gingival recession were measured at 6 sites per tooth (mesiobuccal, midbuccal, and distobuccal; mesiolingual, midlingual, and distolingual). Measurements at each site were made using a periodontal probe (PCP 15/11.5B screening probe; Hu-Friedy, Chicago, Ill) along the root surface and angulating it in a mesiodistal direction but parallel to the long axis of the tooth to avoid a buccolingual angulation ( Fig 3, C and D ). Each measurement was rounded to the lower whole millimeter. Data were recorded directly on a periodontal chart developed by the Department of Periodontology, University of Bern, in Bern, Switzerland, that instantly calculated attachment loss as the difference between probing depth and recession. A pocket of 4 mm or greater was considered to be “deepened” (at risk of attachment loss). Bleeding on probing was registered when bleeding occurred within 15 seconds after probing. Plaque accumulation was registered if residuals were present on passing the probe along the gingival margin of each tooth. Plaque index and bleeding index scores were calculated according to the method of Löe and Silness. Gingival margin recessions were registered on each tooth as present or absent. When an apical displacement of the free gingival margin from the cementoenamel junction occurred, recession was recorded, with the final aim of rating its prevalence. A clinical chart was used in both groups to evaluate periodontal risk factors, such as current and former cigarette smoking, history of diabetes, frequency of visits to a dentist, and familial predisposition.
Occlusal and functional examinations were made intraorally in both groups. Discrepancies between centric relation and centric occlusion of more than 1 mm were registered. Tooth contacts were recorded using thin articulation paper (Articheck 40; Bausch, Koln, Germany), as well as occlusal function in lateral excursions (canine-protected or group function) and the presence of balancing contacts. A questionnaire concerning symptoms related to TMD, such as pain, noises, locking, and parafunctions, was completed by all patients of both groups. They were asked to provide answers to 10 questions, including “Do you ever (1) hear a click from the temporomandibular joint (TMJ); (2) feel crepitation sounds from the TMJ; (3) get pain around the TMJ; (4) get pain in the facial muscles; (5) get pain when chewing or opening your mouth; (6) get headaches; (7) have difficulty opening your mouth; (8) grind your teeth; (9) clench your teeth or hold them tightly together when you are not eating; and (10) bite your tongue, lips, nails, or something else?” The possible answers were 0, no, never; 1, in the past; 2, sometimes; or 3, often.
Statistical analysis
Descriptive statistics were used to summarize the percentages and distributions of the measurements. Normal distributions for the values of all variables were verified in both groups with the Shapiro-Wilk test.
A power analysis was done, and the alpha level was fixed at 0.05. Three tests gave a power over 80%, and only one was underpowered (probing >4 mm). However, in this last statistical analysis, the difference in the frequency was low and had no clinical relevance. Therefore, the risk of a beta error would not influence the final conclusion.
The 2 groups comprised different subjects. As a consequence of this, the 2 samples were independent. An independent t test was used to analyze the outcomes; specifically, a comparison was made between the 2 samples and not within the samples. An unpaired t test was performed to detect any significant changes between data in the AG and the CG. Significance was set at P <0.05. The error of the method of each considered variable was calculated by double measurements in 20% of the sample with Dahlberg’s formula. The obtained value was 0.032, considerably lower than the maximum limit of 0.25.
All data were statistically analyzed with Stata 12 software (StataCorp, College Station, Tex).
Results
In the probing depth evaluation ( Table I ), of the 3942 sites probed in the full-mouth evaluation in the AG, only 18 (0.5%) had a pocket depth greater than 4 mm, and 96 (2.4%) sites were 4 mm deep. The sites with deeper probing depths were mainly in the posterior teeth. Among the 1536 sites probed in the CG, 11 (0.7%) had a depth greater than 4 mm, and 60 (3.9%) sites had a depth of 4 mm.
| Teeth (n) | Sites (n) | PD = 4 mm | PD >4 mm | |||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| AG | ||||||
| Full mouth | 657 | 3942 | 96 | 2.4 | 18 | 0.5 |
| Maxilla | 206 | 1236 | 35 | 2,8 | 9 | 0.7 |
| First molars | 51 | 306 | 10 | 3.3 | 5 | 1.6 |
| Second premolars | 52 | 312 | 7 | 2.2 | 3 | 1.0 |
| First premolars | 51 | 306 | 9 | 3.0 | 1 | 0.3 |
| Canines | 52 | 312 | 9 | 2.9 | 0 | 0 |
| CG | ||||||
| Maxilla | 256 | 1536 | 60 | 3.9 | 11 | 0.7 |
| First molars | 64 | 384 | 27 | 7.0 | 6 | 1.6 |
| First premolars | 64 | 384 | 22 | 5.7 | 3 | 0.8 |
| Canines | 64 | 384 | 8 | 2.1 | 2 | 0.5 |
| Lateral incisors | 64 | 384 | 3 | 0.8 | 0 | 0 |
| t test | P = 0.162 | P = 0.856 | ||||
| NS | NS | |||||
When the maxillary segments in the 2 groups were compared, no statistically significant differences were found (power test, 81% for probing pocket depth of 4 mm; power test, 12% for probing pocket depth >4 mm), either for sites with probing pocket depths greater than 4 mm or for sites with probing pocket depths of 4 mm. Notably, 97.1% of the probing pocket depths around the intruded premolars and extruded canines were within normal limits, and almost identical to the probing pocket depths around the intact canines and lateral incisors in the CG.
For bleeding on probing ( Table II ) in the AG, bleeding was observed in 339 (8.6%) of the 3942 examined sites. Most bleeding sites were registered at the first molars (12.7%), followed by the second premolars (8.3%). In the CG, 271 of the 1536 recorded sites (17.6%) had bleeding on probing. Again, most bleeding sites were observed at the first molars and first premolars. No statistically significant differences between the maxillary teeth in the AG and the CG were observed on the labial and lingual sites, whereas the comparisons of the mesial and distal interproximal sites demonstrated more bleeding that was statistically significant in the CG ( P <0.05), as shown in Table II (power test, 100%). The bleeding sites around the intruded first premolars and the extruded canines were few and less frequent than around the intact canines and lateral incisors in the CG.
| Sites (n) | Sites with BoP | ||
|---|---|---|---|
| n | % | ||
| AG | |||
| Full mouth | 3942 | 339 | 8.6 |
| Maxilla | 1236 | 114 | 9.2 |
| First molars | 306 | 39 | 12.7 |
| Second premolars | 312 | 26 | 8.3 |
| First premolars | 306 | 24 | 7.8 |
| Canines | 312 | 25 | 8.0 |
| CG | |||
| Maxilla | 1536 | 271 | 17.6 |
| First molars | 384 | 74 | 19.3 |
| First premolars | 384 | 78 | 20.3 |
| Canines | 384 | 60 | 15.6 |
| Lateral incisors | 384 | 59 | 15.4 |
| t test | P <0.001 | ||
For the evaluation of gingival recession ( Table III ) in the AG, 26.6% of all 657 teeth examined had slight recessions, mostly on the first molars and second premolars, but less than a third (24.7%) of these were found in teeth selected for the intergroup comparisons. In the CG, 43 of the 256 analyzed teeth (16.8%) showed recessions.



