Introduction
We systematically reviewed observational, experimental, and diagnostic accuracy studies to assess the comparisons between cone-beam computed tomography (CBCT) and conventional radiography (CR) in the localization of maxillary impacted canines.
Methods
An open-ended electronic search of PubMed, Web of Science, ProQuest, and other databases for both published and unpublished articles up to May 2016 was performed. The reference lists of the included studies were screened. Two authors performed the searches with no language restrictions. The research questions were outlined based on a hierarchical model. The primary outcomes were diagnostic accuracy, level of intermodalities agreement, effect of these images on treatment planning and treatment outcomes, and societal efficacy between the CBCT and CR in the localization of impacted canines. Two reviewers evaluated the risk of bias assessment by using the Quality Assessment of Diagnostic Accuracy Studies tool and the Newcastle Ottawa Scale.
Results
Eight studies met the inclusion criteria. Two studies reported diagnostic accuracy, 6 reported intermodalities agreement in impacted canine localization, and 3 reported treatment planning agreement between the modalities. No therapeutic and societal efficacy study found. The accuracy of CBCT ranged from 50% to 95%, and the accuracy of CR ranged from 39% to 85%. A wide range of kappa intermodalities agreement from 0.20 to 0.82, with observed agreement of 64% to 84%, was reported in canine localization. Broad kappa treatment planning agreement values from 0.36 to 0.72 were reported. Most studies suffered from a high risk of bias in subject selection.
Conclusions
The fair to moderate intermodalities agreement in maxillary canine localization might mean that the information obtained through these modalities is deviant and ultimately might affect treatment planning. Although there is still a lack of strong evidence, CBCT is more effective than CR in evaluating cases that are difficult to diagnose in the initial evaluation with CR.
Funding
No funding was received for this study.
Highlights
- •
CBCT is more accurate than radiographs for localizing maxillary impacted canines.
- •
Variations between modalities ultimately affect treatment planning.
- •
No robust evidence supports using CBCT routinely for impacted maxillary canines.
- •
CBCT is indicated when radiography does not provide sufficient information.
- •
Information about patient outcome and societal efficacy is lacking.
Maxillary canines are the second most common teeth (after the third molars) with a tendency for impaction and ectopic eruption. The prevalence ranges from 1% to 3%. Aside from creating esthetic and functional issues, canine impaction may also create root resorption of neighboring teeth, which may then necessitate orthodontic and surgical intervention. Determining the correct location of impacted canines and their relationship to the adjacent dentition and anatomic structures is essential for successful orthodontic treatment.
Various diagnostic methods are used to localize impacted teeth. The techniques allow for the practitioner to predict the difficulty of orthodontic treatment, the duration of treatment, and possible treatment options (including observation, interceptive treatment by extracting the deciduous canines, simple surgical exposure or surgical exposure and placement of an orthodontic attachment, auto transplantation, and canine extraction). The diagnostic process begins with a clinical examination and palpation of alveolar bone followed by radiographic assessments.
Despite the historical use of 2-dimensional (2D) conventional radiographs, 2 inherent drawbacks limit the information obtained: anatomic superimposition and geometric distortion. The resulting poor visibility and misrepresentation of structures may ultimately affect the localization and treatment planning of maxillary impacted canines. As a result, many practitioners have resorted to 3-dimensional (3D) imaging technology.
Cone-beam computed tomography (CBCT) was specifically developed for 3D imaging of the head and neck. Moreover, 2D multiplanar images reconstructed from CBCT volumetric data sets can navigate through submillimeter slices in the axial, coronal, and sagittal planes. However, the benefit-to-risk assessment of CBCT imaging is still controversial. Although CBCT exposes the patient to higher levels of radiation compared with conventional modalities, the long-term effects of excessive ionizing radiation above background levels of ionizing radiation remain unknown. Recent risk estimates have reported higher cancer rates based on current exposure levels. As a result, evidence-supported criteria to ensure the responsible application of CBCT should be weighed against the biologic and financial costs to the patient.
Some studies have reported that CBCT imaging is clearly advantageous in the management of impacted canines. Other studies have reported that CBCT allows orthodontists to improve diagnostic capabilities and that it is more accurate at localizing maxillary impacted canines. However, we could not find any comparative systematic review that evaluated the difference in the information yielded between CBCT and conventional imaging in their localization of maxillary canine impaction, the efficacy of these approaches in treatment planning, and their treatment outcomes.
In this study, we aimed to systematically review whether there is any difference in the diagnostic accuracy, the level of intermodalities agreement in impacted canine localization, treatment planning, and therapeutic and societal efficacy between CBCT and conventional radiograph imaging.
Material and methods
The research questions were outlined based on the 6-tiered hierarchical model by Fryback and Thornbury. Therefore, according to clinical usefulness in the decision-making process, we investigated responses to the following questions.
- 1.
What is the difference between the modalities in the accuracy of maxillary impacted canine localization?
- 2.
What is the intermodalities agreement between information obtained by CBCT compared with conventional radiographs for the localization of maxillary impacted canines?
- 3.
What is the level of agreement between the treatment decisions made from CBCT compared with conventional radiographs?
- 4.
What is the difference between the treatment outcomes provided through these modalities?
- 5.
What is the difference between the societal costs incurred with these modalities?
An open-ended electronic search was conducted through PubMed, CINHAL, Web of Science, and Cochrane Library databases up to May 2016 with a wide variety of key words. A search of unpublished literature was also conducted through the Pro-Quest Dissertation Abstracts and Thesis database and Google Scholar by limiting the search by the first 200 hits. Table I provides a detailed summary of the final search key words for each database. A manual search of the included studies’ references was performed to supplement the literature search. There were no language restrictions. Also, to improve the reporting of this systematic review, the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement guidelines were followed. No protocol registration was conducted.
| PubMed: up to May 28, 2016 |
| ((“Cone-Beam Computed Tomography”[Mesh] OR cone beam computed tomography OR CBCT) AND (“Radiography, Panoramic”[Mesh] OR “Cephalometry”[Mesh] OR conventional imaging OR traditional imaging OR panoramic OR periapical OR cephalogram OR “2D image” OR “two dimensional” OR orthopantomogram OR occlusal) AND (canine)) |
| Web of Science: up to May 15, 2016 |
| ((“cone beam computed tomography” OR CBCT) AND (conventional OR traditional OR panoramic OR periapical OR cephalogram OR “2D image” OR “two dimensional” OR orthopantomogram OR occlusal) AND (canine)) |
| CINHAL: up to May 13, 2016 |
| ((“cone beam computed tomography” OR CBCT) AND ((MM “Radiography, Panoramic”) OR (MM “Cephalometry”) OR conventional OR traditional OR panoramic OR periapical OR cephalogram OR “2D image” OR “two dimensional” OR orthopantomogram OR occlusal) AND canine)) |
| Cochrane Library: up to May 15, 2016 |
| ((“cone beam computed tomography” OR CBCT) AND ((MM “Radiography, Panoramic”) OR (MM “Cephalometry”) OR conventional OR traditional ∖OR panoramic OR periapical OR cephalogram OR “2D image” OR “two dimensional” OR orthopantomogram OR occlusal)) AND canine)) |
| Google Scholar: up to May 10, 2016 |
| ((“cone beam computed tomography” OR CBCT) AND (conventional OR traditional OR panoramic OR periapical OR cephalogram OR “2D image” OR “two dimensional” OR orthopantomogram OR occlusal) AND (canine))) |
| ProQuest: up to May 14, 2016 |
| (“cone beam computed tomography” OR CBCT) AND (conventional OR traditional OR panoramic OR periapical OR cephalometry OR “2D image” OR “two dimensional” OR orthopantomogram OR occlusal) AND (canine) |
The Population, Intervention, Comparison, Outcome and Study design (PICOS) framework was followed. The population was defined as the patients or models who had a maxillary impacted canine with or without neighboring lateral incisor root resorption. The intervention and comparison were respectively defined as the CBCT scan data and conventional (2D) radiographs (panoramic, periapical, occlusal, and cephalograms). The primary outcome was described as the diagnostic accuracy between the modalities, intermodalities agreement in impacted canine localization, treatment planning and outcome efficacy, and societal assessment. The secondary outcome included the intermodalities agreement in lateral root resorption detection and intraobserver and interobserver agreement values. All types of study designs such as observational (other than case reports), experimental, and diagnostic accuracy studies were included.
The included studies compared CBCT imaging with conventional 2D radiographs (panoramic, periapical, occlusal, and cephalograms) in maxillary impacted canine localization (with or without associated features: ie, lateral root resorption) that reported any of the following.
- 1.
Accuracy, sensitivity, or specificity between the modalities while applying an appropriate reference test such as a simulated model (ex vivo) or surgical exploration (in vivo).
- 2.
The level of intermodalities agreement in localization of the impacted canine.
- 3.
The level of intermodalities agreement in treatment planning.
- 4.
Treatment outcomes (the primary outcome was defined as the treatment outcomes or complications between the modalities that were compared based on prospective or retrospective studies).
- 5.
Societal efficacy (the primary outcome was defined as direct or indirect costs: capital costs, accommodation costs, provider time costs, operational costs, radiologic costs, radiographic costs, overheads, time costs of patients and accompanying persons, and out-of-pocket costs for the examination fee and visit).
In addition, the excluded studieswere those that assessed conventional tomography scans; case reports, reviews, editorials, commentaries, or conference proceedings comparing CBCT scans with 2D radiographs generated from CBCT volumetric data; or reports by observers in the control group (conventional radiographs) who were exposed to the case group (CBCT) results.
The studies found by electronic and manual searches were selected for inclusion independently by 2 authors (E.E., H.B.). The definitive inclusion of a potentially relevant article was decided by consensus. Data extraction was independently performed by the same reviewers. The reviewers extracted data investigating the response to the research questions. The data extraction items were first author, publication year, imaging systems, sample size, scanning parameters for CBCT systems, number of examiners, study design, outcome variables, and corresponding results. Any discrepancies were resolved by discussion and consensus agreement between the 2 authors.
The quality of the studies was evaluated for a risk of bias independently by the same investigators (E.E., H.B.). The Newcastle-Ottawa Scale was used for the assessment of case-control and cohort studies. This scale assesses 3 domains: selection, comparability, and outcome. The Newcastle-Ottawa Scale tool for the cohort studies was modified for the cross-sectional studies. Three of the 9 items, “demonstration that outcome of interest was not present at start of study,” “was follow-up long enough for outcomes to occur?” and “adequacy of follow-up,” were excluded, because they are not relevant to cross-sectional studies. A study could be awarded a maximum of 1 star for each item of the selection and outcome categories, and a maximum of 2 stars for comparability. The overall quality rating was the sum of the stars (maximum of 9 for case control and cohort studies and 6 for cross-sectional studies).
The Quality Assessment of Diagnostic Accuracy Studies (QUADAS-2) tool was applied to rate the methodologic quality of the diagnostic accuracy studies. This tool consists of 4 key domains: patient selection, index test, reference standard, and flow and timing. The risk of bias was judged as low, high, or unclear.
For the diagnostic studies, accuracy, specificity, and sensitivity outcome variables were reported when available. For the observational studies, any type of agreement between the modalities (Fleiss kappa, Cohen’s kappa, logistic regression model, observed agreement, and so on) in terms of localizing the impacted canine and treatment planning were disclosed. In addition, the intraobserver and interobserver agreements for each modality were reported when available. A meta-analysis was not appropriate because of the heterogeneity in the design, type of intervention, study population, and outcome variables of the included studies. To synthesize and interpret the kappa level of agreement, the kappa classification of Landis and Koch was applied (slight, 0.01-0.20; fair, 0.21-0.40; moderate, 0.41-0.60; substantial, 0.61-0.80; and almost perfect, 0.81-1.00).
Results
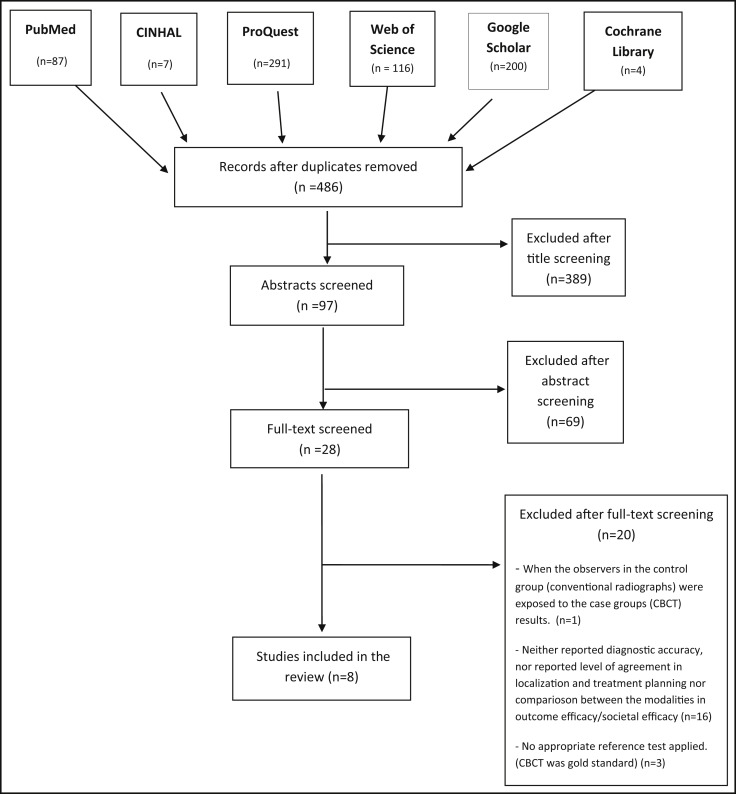
The Figure shows the database search and the study inclusions. The initial review included 705 articles. When duplicate results were excluded, 486 review articles remained. No study was added after a manual review. A total of 28 articles were considered potentially eligible after screening of the title and abstract. Upon evaluation of the full texts, 8 of the 28 remaining studies met all inclusion and exclusion criteria. These studies are listed in Table II .
| Author, year | Imaging systems | Sample size | Imaging parameters for CBCT systems | Examiners | Study design |
|---|---|---|---|---|---|
| Serrant et al, 2014 | CON: horizontal parallax (periapical), vertical parallax (panoramic and occlusal) CBCT: I-CAT |
One extracted tooth mounted in 9 different positions | FOV: 6 cm Scan time: 8.9 sec VS: 0.3 mm |
6 4 orthodontists 1 dentist 2 dental and maxillofacial specialists |
Diagnostic accuracy |
| Pittayapat et al, 2014 | CON: digital OPG CBCT: 3D Accuitomo 170 |
38 patients | FOV: 14 × 10 cm kVp:90 mA; 5 Scan time:30.8 sec VS: 0.25 mm |
8 3 radiologists 5 orthodontic residents |
Observational-cross sectional |
| Lai et al, 2014 | CON: OPG CBCT: Accuitomo XYZ Slice View Tomograph |
60 patients (72 impacted canines) | FOV: 4 × 4, 6 × 6 or 8 × 8 cm mA: 5 kV: 80 |
11 OPG 5 oral surgeons 5 orthodontists CBCT 1 orthodontist |
Observational- cross sectional |
| Wriedt et al, 2012 | -CON: OPG -CBCT: Accuitomo |
21 patients (29 impacted canines) | FOV: 4 × 4 cm NR |
26 10 orthodontists 8 dental surgeons 8 general dentists |
Observational -cross sectional |
| Alqerban et al, 2011 | -CON: OPG -CBCT: Accuitomo-XYZ Slice View Tomograph -CBCT: Scanora |
-Group A (Accuitomo vs CON): 30 -Group B (Scanora vs CON): 30 Total of 60 patient (89 impacted canines) |
Accuitomo-XYZ: VS: 0.125 mm FOV: 3 × 4 cm kV: 80 mA: 3 Scan time: 18 sec Detector type: IIT Scanora: VS: 0.2 mm FOV:75 × 100 mm kV:85 mA:15 Scan time: 3.7 sec |
3 experienced dental practitioners | Observational- cross sectional |
| Botticelli et al, 2011 | -CON: OPG, LC, PA -CBCT: NewTom 3G |
27 patients (39 impacted canines) | Volumetric rendering method | 8 dentists 5 residents 3 specialists with >5 y experience |
Observational-cross sectional |
| Haney et al, 2010 | -CON: OPG, occlusal, and 2 periapical -CBCT: MercuRay |
18 patients (25 impacted canines) | Volumetric rendering method | 7 4 orthodontists 3 oral surgeons |
Observational- cross sectional |
| Herring, 2006 | -CON: panoramic, 2 periapical, 2 occlusal. -CBCT: NewTom 3G |
10 simulated skulls | FOV: 12 in Slice thickness: 0.5 mm |
17 specialists: 11 orthodontists 6 radiologists |
Diagnostic accuracy |
Table III gives the risk of bias assessment of the observational studies. Most studies had a high risk of selection bias, with some difficult-to-diagnose cases to compare between modalities. Table IV also demonstrates the risk of bias in studies with diagnostically accurate study designs.
| Study | Selection (of 3 stars) | Comparability (of 2 stars) | Outcome (of 1 star) | Total (of 6 stars) |
|---|---|---|---|---|
| Alqerban et al | *** | ** | * | ****** |
| Pittapayat et al | ** | ** | * | ***** |
| Haney et al | ** | ** | * | ***** |
| Wriedt et al | ** | * | * | **** |
| Lai et al | ** | * | * | **** |
| Botticelli et al | * | * | * | *** |
| Study | Risk of bias | Applicability | |||||
|---|---|---|---|---|---|---|---|
| Patient selection | Index test | Reference standard | Flow and timing | Patient selection | Index test | Reference standard | |
| Serrant et al | ☹ | ☺ | ☺ | ☺ | ☺ | ☺ | ☺ |
| Herring | ☹ | ☹ | ☺ | ☺ | ☺ | ☺ | ☺ |
We looked at diagnostic accuracy between the modalities. Two studies reported the level of accuracy between the modalities. The accuracy of CBCT ranged from 50% to 95%, and the accuracy of conventional radiographs ranged from 39% to 85%. CBCT showed higher accuracy than conventional radiographs ( Table V ).
| Authors | Outcome variables | Results |
|---|---|---|
| Serrant et al, 2014 | Intermodalities accuracy: | CBCT (94%), horizontal parallax (83%), vertical parallax (65%) ( P <0.01) |
| Interobserver agreement: | Cohen weighted kappa = 0.7528 | |
| Intraobserver agreement: | Cohen weighted kappa = 0.8985 | |
| Pittayapat et al, 2014 | Intermodalities agreement: | CBCT vs OPG: (Fleiss kappa) |
| -canine localization (palatal, buccal, middle) | -k = 0.2, 27.7% unidentified in OPG, P <0.0001 | |
| -canine angulation to midline | -k = 0.3, P <0.0001 | |
| -lateral root resorption | -k = 0.3, P <0.0001, unidentified 24% in OPG and 7% in CBCT | |
| Intraobserver agreement | -3D: k = 0.71, 2D: k = 0.65 P <0.0001. CBCT shows better intra-agreement. |
|
| Interobserver agreement | -3D: k = 0.50, 2D: k = 0.40. P <0.0001 | |
| Lai et al, 2014 | Intermodalities agreement: | CBCT vs OPG: (Pr agreement) |
| -labiopalatal canine localization | -Pr: 0.29, P = 0.04 | |
| -lateral root resoprtion | -Pr: 0.93, P = 0.52 (NSD) | |
| Wriedt et al, 2012 | Intermodalities agreement | Between OPG + study cast vs CBCT + study cast: (Cohens k) |
| -canine localization (total agreement) | -observed agreement: 64%, k = 0.47 agreement with master findings: CBCT: 0.7, OPG: 0.37 |
|
| -therapy proposals (no statement, alignment, osteotomy) | -observed agreement: 82%, k = 0.36. CBCT led to retraction of premature decisions to extract teeth | |
| Alqerban et al, 2011 | Angular distances: | 2 CBCT vs OPG: ( P value) |
| -canine angle to lateral incisor | -NSD | |
| -canine angle to midline | -NSD for A and <0.0001 for B group | |
| -canine angle to occlusal plane | -0.0101 for A and 0.0010 for B group | |
| -canine location: palatal, buccal, arch line) | -0.0074 for group A and P = 0.0008 for B | |
| -root resorption detection | -group A: 53% vs 29%, P = 0.0201 -group B: 50% vs 30%, P <0.001 |
|
| Interobserver agreement | ||
| -canine location | 3D: k = 0.63-0.68 2D: k = 0.31 | |
| -lateral root resoprtion | 3D: k = 0.63-0.65 2D: k = 0.48 Higher in CBCT |
|
| Botticelli et al, 2011 | Intermodalities agreement: | CON (PA, LC, OPG) vs CBCT: (observed agreement and Cohen kappa agreement) |
| -inclination to midline | -NSD, 74% agreement | |
| -mesiodistal position of apex | -0.001 ( P value): 64% agreement, less variation in apex position in 2D | |
| -vertical level of crown | -0.013: 66% agreement, higher vertical level in 2D | |
| -overlap with lateral incisor | -0.001: 70% agreement, less overlap in 2D | |
| -labiopalatal crown position | -0.001: 68% agreement, more palatal position of crown in 2D, k = 0.3 | |
| -labiopalatal apex position | -0.001: 65%, agreement, more palatal position of crown in 2D, k = 0.2 | |
| -root resorption of neighboring incisor | -0.0001, 82% agreement, k = 0.3, 2D indicated less root resorption | |
| -treatment choice (deciduous canine extraction, observation, permanent canine extraction, surgical extraction and orthodontics, surgical transplantation) | -0.0008, 70% agreement CBCT leads more orthodontic and surgical intervention; 2D leads observational intervention |
|
| Haney et al, 2010 | Intermodalities agreement: | Observed and kappa agreement: |
| -mesiodistal cusp tip location | -CBCT vs occlusal: 79%, k = 0.76 | |
| -labiopalatal location | -CBCT vs 2 periapical: 84%, k = 0.82, significant difference | |
| -vertical location | -CBCT vs OPG: k = 0.63 | |
| -root resorption detection | -63%, k = 0.65, P <0.0001 | |
| -treatment plan (extract, leave, recover) | -73% agreement. k = 0.72, <0.0001 | |
| Intra observer agreement | ||
| -canine localization | -2D: k = 0.73-0.92, 3D: k = 0.53-0.77 | |
| -lateral root resorption | -2D: k = 0.73, 3D: k = 0.55 | |
| -treatment planning. | -2D: k = 0.77, 3D: k = 0.64 NSD between 2D and 3D |
|
| Herring, 2006 | Intermodalities accuracy: | CBCT vs CR: (%) |
| Buccopalatal localization- relative to lateral incisor | orthodontists: 95 vs 65 ( P <0.0001) radiologists: 90 vs 85 ( P <0.4) |
|
| relative to central incisor | orthodontists: 54.5 vs 54.5 radiologists: 50 vs 66.6 |
|
| Proximity relative to canine | orthodontists: 60 vs 39 ( P = 0.0005) radiologists: 85 vs 40 ( P <0.0001) |
|
| Lateral root resorption | orthodontists: 70 vs 48 radiologists: 87 vs 55 |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


