This case report describes the multidisciplinary treatment of a male with a dilacerated maxillary left central incisor and transposition of the ipsilateral maxillary canine and lateral incisor. The initial treatment plan involved removal of the dilacerated incisor with mechanical eruption and alignment of the ectopic left canine, aiming to substitute the lateral incisor for the missing central incisor. However, the plan was modified to include eruption of the canine in the central incisor region in response to progressive ectopic development and mesial transmigration of the maxillary left canine. Although substitution of a maxillary canine for a central incisor is comparatively rare, the canines offer a relatively favorable template to simulate a central incisor. For this growing patient with a combination of dental trauma and developmental anomalies, maxillary canine-central incisor replacement was a viable option, offering excellent esthetic results without recourse to prosthetic replacement.
The primary aims of orthodontic treatment are invariably to optimize dental and facial esthetics and occlusal function. Typically, realizing these goals involves alignment of the teeth in their intended natural sequence. Rarely, gross displacements and transpositions that result from ectopic development, occurring either in isolation or together, require compromises to these goals to achieve realistic yet acceptable esthetic and functional outcomes.
Dilaceration is characterized by an abrupt deviation of the axial angulation of a tooth; this can occur anywhere along the crown, cementoenamel junction, root, or apex. It is thought to relate to either traumatic injury or ectopic development of the tooth germ. Dilaceration has been reported in the maxillary deciduous incisors, mandibular permanent incisors, and maxillary canines and premolars, but it most commonly affects a maxillary central incisor. Typically, dilaceration manifests as either failure of eruption or displacement of the affected tooth. Transposition, defined as the positional interchange of 2 adjacent or nonadjacent teeth, has a prevalence of 0.3%. The most common teeth to be transposed are the maxillary canine with the maxillary first premolar, followed by the maxillary lateral incisor and the canine. Maxillary canine ectopia is a more common dental anomaly, with a palatal predilection.
Although these developmental conditions most commonly arise in isolation, co-occurrence of dental abnormalities is well established. This article describes a patient with multiple dental anomalies, including a dilacerated maxillary central incisor and transposed, ectopic maxillary lateral incisor and canine, requiring combined orthodontic, surgical, and prosthodontic management.
Diagnosis and etiology
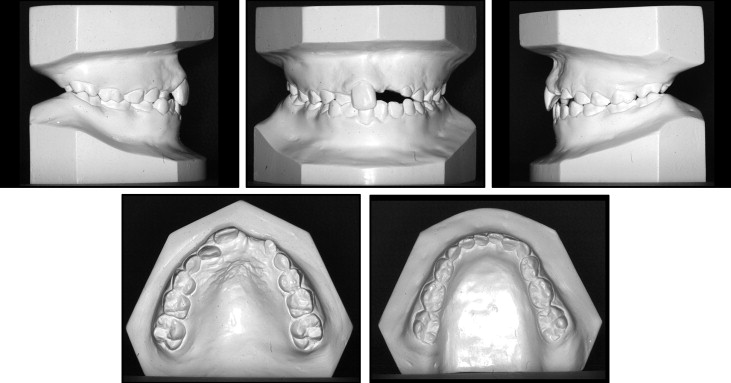
A 7-year-old boy was referred to the orthodontic department of the Kent and Canterbury Hospital by his general dental practitioner regarding an unerupted maxillary left central incisor. The patient was concerned about the apparent absence of the maxillary incisor. The patient and parents reported a history of trauma to both the maxillary right and left deciduous central incisors at 3 years of age, resulting in loss of vitality of the affected teeth. Both teeth were monitored but untreated by the general dental practitioner. The patient had well-controlled asthma. On clinical examination, there was a skeletal Class I pattern with average vertical facial proportions ( Fig 1 ). The lips were competent and protrusive to the E-line, with an acute nasolabial angle, 4 mm of incisor show at rest, and reduced incisor show on smiling. The temporomandibular joints were symptomless.

Intraorally, the patient was in the mixed dentition with good oral hygiene. The mandibular arch was mildly crowded, with the anterior segment of average inclination, with an average curve of Spee. The maxillary arch was spaced, with average inclination of the anterior teeth. In occlusion, the molar relationships were Angle Class I bilaterally; the incisor relationship was also Class I. There was a crossbite without displacement associated with the maxillary right lateral incisor, and overjet was reduced, at 1 mm. Overbite was average and complete with noncoincident centerlines; the maxillary centerline was displaced 2 mm to the left side ( Fig 2 ).
A dentopantomograph confirmed the presence of all teeth and highlighted a root dilaceration affecting the maxillary left central incisor and an ectopic position of the maxillary left lateral incisor ( Fig 3 ). The cephalometric analysis confirmed the clinical findings and also showed the extent of the dilaceration of the maxillary left central incisor ( Fig 4 ).


Treatment objectives
The initial plan involved removal of the dilacerated maxillary left central incisor with a poor prognosis with mechanical eruption and alignment of the ectopic maxillary left lateral incisor, aiming to substitute the maxillary left lateral incisor for the maxillary left central incisor. This was to be followed by space reopening upon eruption of the canines, facilitating prosthetic replacement of the maxillary left central incisor with adhesive bridgework as an interim measure. Other objectives included relief of crowding, alignment of both dental arches, and correction of the anterior crossbite and centerline discrepancy with maintenance of the Class I incisor and molar relationships. However, this plan and some objectives were modified in response to progressive ectopic development and transmigration of the maxillary left canine.
Treatment objectives
The initial plan involved removal of the dilacerated maxillary left central incisor with a poor prognosis with mechanical eruption and alignment of the ectopic maxillary left lateral incisor, aiming to substitute the maxillary left lateral incisor for the maxillary left central incisor. This was to be followed by space reopening upon eruption of the canines, facilitating prosthetic replacement of the maxillary left central incisor with adhesive bridgework as an interim measure. Other objectives included relief of crowding, alignment of both dental arches, and correction of the anterior crossbite and centerline discrepancy with maintenance of the Class I incisor and molar relationships. However, this plan and some objectives were modified in response to progressive ectopic development and transmigration of the maxillary left canine.
Treatment alternatives
The following treatment alternatives were considered and discussed with the patient and his parents.
- 1.
Extraction of the dilacerated maxillary left central incisor and mechanical alignment of the maxillary left lateral incisor and maxillary left canine into their respective positions with prosthetic replacement of the maxillary left central incisor with a Maryland bridge initially, followed by dental implant replacement at skeletal maturity.
- 2.
Extraction of the dilacerated central incisor and mechanical alignment of the maxillary left lateral incisor to substitute for the maxillary left central incisor. To facilitate substitution, the maxillary left lateral incisor would be intruded to harmonize the gingival marginal height with direct composite recontouring. Space closure in the maxillary left quadrant would be directed using a temporary anchorage device for protraction of the buccal segment, finishing to a full-unit Class II molar relationship on the left side.
- 3.
Alignment of all maxillary anterior teeth in their correct developmental positions with attempts to optimally align the dilacerated maxillary left central incisor. Alignment would be resisted by encroachment on the buccal cortical plate. With this approach, provision would be made for an apicoectomy to permit improved alignment of the maxillary left central incisor.
- 4.
Extraction of the dilacerated maxillary left central incisor, in addition to the maxillary right second premolar, mandibular left second premolar, and the mandibular left second premolar with autotransplantation of a mandibular premolar into the maxillary central incisor position. This approach would necessitate restorative treatment to simulate the appearance of the maxillary left central incisor initially with direct composite recontouring.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


