The increased availability of computed tomography (CT) and the development of adjunctive software have provided surgeons with new techniques for planning and placement of dental implants. These procedures provide improvements in safety, predictability, and accuracy. Surgeons, restorative dentists, and patients all benefit from the use of reconstructed images, analysis and planning software, and guides for precise osteotomy and placement of implants. Acceleration of prosthetic reconstruction is often possible.
The combination of CT scanning and planning software has also assisted the shift in treatment planning from one that is implant based to one based on the final restoration. By including the biologic principles of implant integration, bone vitality, and soft tissue response, it is possible to develop a plan of treatment that is more likely to result in pleasing functional and esthetic outcomes. The need for hard or soft tissue augmentation of the implant site and for angulated abutments and the possibility of accelerated provisional restoration may be determined before surgery. All these factors are of benefit to the patient, surgeon, and restorative dentist.
Etiopathogenesis/Causative Factors
Dental implants must be placed in locations that are biologically suitable and acceptable for restorative needs. Frequently, these sites have questionable bone volume and are in proximity to other teeth or anatomic structures. Undesirable outcomes include damage to the inferior alveolar nerve (IAN), fenestration of buccal or lingual bone, collisions with the roots of teeth, and improper angulation. Planning of implant location before surgery and guidance during osteotomy and implant placement reduce the risk for error.
Diagnostic Studies
For optimal benefit, a sequence of planning appointments is required for collection of data and communication between the surgeon and restorative dentist before and during treatment. It is desirable for all dentists and their office staff involved in the process to understand the benefits of CT-guided planning and placement. They must know the sequence and timing of care and the cost for scans, planning software, and service, as well as surgical and restorative fees. By planning the case to completion before beginning treatment it is much more likely that the proposal to the patient will be accurate and that alternatives can be considered realistically.
The primary focus of implant-based restoration is the final prosthesis. The functional and esthetic requirements must be determined early in the planning process, and the expected results of treatment and alternative plans that may be available must be discussed with the patient.
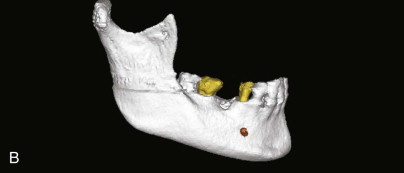
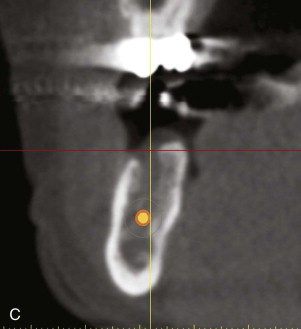
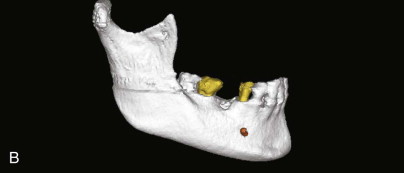
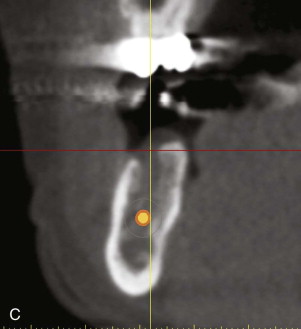
A comprehensive examination of the oral cavity and a review of systemic conditions and medications must be conducted to determine suitability for implant surgery. The examination should also include an assessment of occlusion. Periapical and panoramic radiographs are helpful, but not definitive. It is not always possible to make accurate three-dimensional evaluations from two-dimensional images. A comparison of conventional radiographs and CT scan data shows the difference ( Fig. 25-1 ).

The customary assessments for implant placement are adequate in some instances, typically when esthetic demands are not high, but to take advantage of planning software and to make a plan based on the desired restoration, additional steps are required. These steps involve making an accurate provisional restoration that can be used as a scanning guide during the CT process.
The foundation of planning for guided implant placement is a set of accurate study models precisely articulated in the correct occlusal relationship. It is important to evaluate the occlusion in maximum intercuspation and in lateral and protrusive excursion. Anticipating occlusal forces can help avoid complications after delivery of the restoration. This procedure is valuable for both single-tooth restorations and full-arch prostheses.
It is the choice of the dentist whether to make the impression with an elastomeric material such as polyvinyl siloxane (PVS) or irreversible hydrocolloid (alginate) and whether to pour the casts with improved stone or die stone. One advantage offered by using PVS is that multiple pours may be made from the same impression, which will be more consistently accurate than reproducing casts made from alginate impressions. This benefit outweighs the increased cost of the material. Dental die stone offers some advantages over improved stone. Die stone is less subject to setting expansion and is more resistant to damage during handling or fitting of the surgical guide.
Diagnostic Studies
For optimal benefit, a sequence of planning appointments is required for collection of data and communication between the surgeon and restorative dentist before and during treatment. It is desirable for all dentists and their office staff involved in the process to understand the benefits of CT-guided planning and placement. They must know the sequence and timing of care and the cost for scans, planning software, and service, as well as surgical and restorative fees. By planning the case to completion before beginning treatment it is much more likely that the proposal to the patient will be accurate and that alternatives can be considered realistically.
The primary focus of implant-based restoration is the final prosthesis. The functional and esthetic requirements must be determined early in the planning process, and the expected results of treatment and alternative plans that may be available must be discussed with the patient.
A comprehensive examination of the oral cavity and a review of systemic conditions and medications must be conducted to determine suitability for implant surgery. The examination should also include an assessment of occlusion. Periapical and panoramic radiographs are helpful, but not definitive. It is not always possible to make accurate three-dimensional evaluations from two-dimensional images. A comparison of conventional radiographs and CT scan data shows the difference ( Fig. 25-1 ).

The customary assessments for implant placement are adequate in some instances, typically when esthetic demands are not high, but to take advantage of planning software and to make a plan based on the desired restoration, additional steps are required. These steps involve making an accurate provisional restoration that can be used as a scanning guide during the CT process.
The foundation of planning for guided implant placement is a set of accurate study models precisely articulated in the correct occlusal relationship. It is important to evaluate the occlusion in maximum intercuspation and in lateral and protrusive excursion. Anticipating occlusal forces can help avoid complications after delivery of the restoration. This procedure is valuable for both single-tooth restorations and full-arch prostheses.
It is the choice of the dentist whether to make the impression with an elastomeric material such as polyvinyl siloxane (PVS) or irreversible hydrocolloid (alginate) and whether to pour the casts with improved stone or die stone. One advantage offered by using PVS is that multiple pours may be made from the same impression, which will be more consistently accurate than reproducing casts made from alginate impressions. This benefit outweighs the increased cost of the material. Dental die stone offers some advantages over improved stone. Die stone is less subject to setting expansion and is more resistant to damage during handling or fitting of the surgical guide.
Treatment/Reconstructive Goals
At the completion of implant integration and placement of the final restoration, the patient must have acceptable function, esthetics, and comfort. The goal of using computer-assisted implant surgery is to make the planning process more predictable and to achieve the desired outcomes more easily and with a reduction in risk.
Current understanding, gained through long clinical experience, provides guidelines for the location and dimensions of implants. The general consensus is that the minimum distance between an implant and an adjacent natural tooth should be 1.5 mm. The distance between implants should be no less than 3 mm. The minimal thickness of bone surrounding the implant on the facial and lingual aspects should be a minimum of 1.0 to 1.5 mm.
Specific Treatment And Techniques
The scanning appliance provides the information needed to identify the location of prosthetic teeth and the soft tissue surface. Many popular planning programs use a “double-scan” process. Reference markers are embedded in the appliance or attached to it before the scan is made. The patient is scanned while wearing the appliance, and then the appliance is removed and scanned by itself outside the mouth at a different beam intensity. The software uses the reference markers to correlate the images. With this technique, denture base resin and artificial teeth, which are rendered poorly with scans made at settings to examine bone, can be reconstructed for planning purposes. Soft tissue dimensions may be calculated as the difference between the scan appliance and bone. For this to be accurate, the scan appliance must be well adapted to the soft tissue. One diagnostic model should be used to create an appliance to be worn by the patient during the CT scan. Another model should be left unmodified as part of the patient’s records. The third model may be used for fabrication of a provisional restoration.
The number and location of markers depend on the software program. The specific nature of the markers should be determined before the scanning appliance is fabricated. Often, the markers are small pieces, approximately 1 mm in diameter, of gutta percha or lead foil ( Fig. 25-2 ).

Some planning software can accommodate a radiopaque guide, which is commonly used in a “single-scan” technique. This process can be accurate but is more labor intensive and may introduce scatter into the CT image if too much barium sulfate is incorporated into the guide. Most radiopaque scan guides are composed of a combination of 10% to 20% barium sulfate by weight in methylmethacrylate. Unless carefully controlled, contraction during polymerization can create gaps at the tissue surface, which would result in poor characterization of the soft tissue surface in the reconstructed image. It is also critical to control the distribution of the barium sulfate in the acrylic resin. Poor mixing before addition of the monomer results in a scan appliance that is not homogeneous and has spots of high radiolucency. This may lead to undesired scatter in the scan data and thus mask critical structures ( Fig. 25-3 ).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses



