We report the successful treatment of a woman aged 25 years 3 months with bilateral cleft lip and palate. She had a protruded premaxilla, collapsed posterior segments, wide alveolar defects with oronasal fistulae, a congenital missing tooth, and severe facial asymmetry with a transverse occlusal cant. The comprehensive treatment approach included (1) premaxillary osteotomy combined with alveolar bone grafting to reposition the premaxilla and minimize the wide alveolar defects, (2) autotransplantation of a tooth with complete root formation to the grafted bone region to restore the missing tooth without a prosthesis such as a dental implant or bridge, and (3) 2-jaw surgery to improve facial asymmetry. The premaxillary osteotomy was managed orthodontically, in combination with bone grafting. The results suggest that surgical orthodontic treatment with tooth autotransplantation might be useful to improve the occlusion and facial esthetics without prosthetics.
Patients with bilateral cleft lip and palate (BCLP) often have collapsed posterior maxillary segments, a protruded premaxillary segment, and retroclined maxillary central incisors. The conventional treatment aims to expand the posterior maxillary segment, procline the maxillary incisors, and restore the missing tooth in the region of the cleft with a prosthesis such as dentures or a bridge. However, these approaches often lead to wide alveolar defects. Defect size has been reported to influence the success of alveolar bone grafting. For the best chance of favorable bone grafting results, it is important to minimize the orthodontic expansion and reduce the size of the defect. Surgical repositioning of the displaced premaxillary segment in combination with bone grafting has been effective in treating BCLP. This approach is also effective to minimize alveolar defects and is useful for stabilization of the grafted bone.
Successful alveolar bone grafting enables restoration of the missing tooth in the cleft region with a dental implant or tooth autotransplantation. The restoration of missing teeth through autotransplantation has been reported using teeth with incomplete root formation. Tooth autotransplantation to a noncleft region, with movement of the tooth adjacent to the cleft into the bone-grafted region, has also been reported. However, there are few reports of tooth autotransplantation using teeth with complete root formation in adults with cleft lip and palate.
In this case report, we describe a comprehensive treatment approach in an adult patient with BCLP.
Diagnosis and etiology
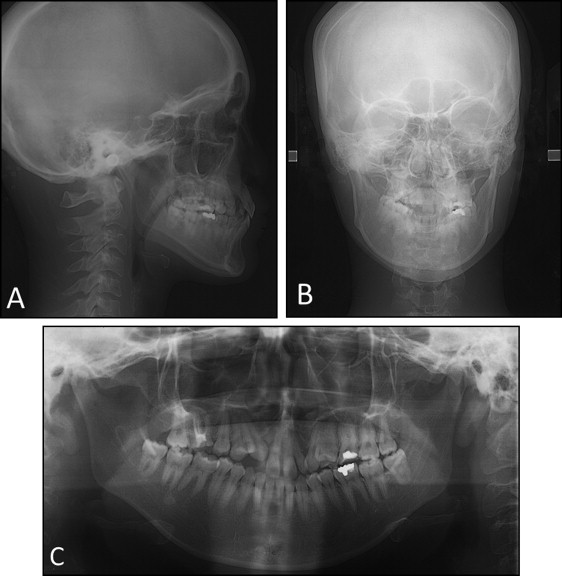
A 25-year-old woman with complete BCLP was referred to our department at Tokyo Medical and Dental University in Japan with the chief complaint of dissatisfaction with the appearance of her teeth, lips, and nose ( Fig 1 ). The patient had congenital BCLP and had undergone cheiloplasty at 6 and 8 months of age, palatoplasty at 1.2 years of age, and lip repair by the Abbe method at 18 years of age at other institutions.

Her facial profile was concave, with a flat nose and protrusion of the upper and lower lips. She had facial asymmetry with mandibular deviation to the right and upward canting of the occlusal plane on the right. The molar relationships were Angle Class III on the right side and Angle Class I on the left side because the maxillary left molar was in mesioversion ( Figs 1 and 2 ). The patient’s maxillary arch was remarkably constricted, with lateral crossbites on both sides. The maxillary right lateral incisor was congenitally missing, and the maxillary left second premolar was located lingually. Alveolar defects with oronasal fistulae were present on both sides, with the nasal opening wider than the oral opening.

Averaged values from the lateral cephalometric analysis indicated an ANB angle of 2.0°, an SNA angle of 80.5°, and an SNB angle of 78.5°, with an excessively protruded premaxilla and retroclined maxillary central incisors ( Fig 3 ; Table ). The posteroanterior cephalometric analysis showed mandibular deviation toward the right of approximately 8.0 mm at the mental spine. The occlusal plane was canted up approximately 5.0 mm on the right. Computed tomography (CT) showed that the base of the premaxilla protruded excessively, and the alveolar defects were markedly wide on the nasal side ( Fig 4 ).
| Pretreatment | Posttreatment | 3 years postretention | |
|---|---|---|---|
| SNA angle (°) | 80.5 | 77.0 | 77.7 |
| SNB angle (°) | 78.5 | 76.5 | 76.9 |
| ANB angle (°) | 2.0 | 0.5 | 0.8 |
| Facial angle (°) | 85.9 | 85.5 | 85.7 |
| Mandibular plane angle (°) | 29.2 | 29.4 | 30.3 |
| Gonial angle (°) | 133.9 | 132.3 | 132.3 |
| U1-FH (°) | 100.4 | 113.7 | 111.1 |
| L1-MP (°) | 90.0 | 87.2 | 83.2 |
| Interincisal angle (°) | 140.3 | 129.7 | 135.4 |
| Occlusal plane angle (°) | 15.3 | 8.6 | 10.4 |

Treatment objectives
The patient was diagnosed with an Angle Class III malocclusion with skeletal Class I, facial asymmetry with a canted occlusal plane, and BCLP. Based on the diagnostic records and consultation with the patient, the following objectives were developed: (1) reconstruct the alveolar defects by bone grafting, (2) reposition the premaxilla by osteotomy to reduce the size of the alveolar defects and improve the retroclined maxillary incisors, (3) transplant the maxillary left second premolar into the right cleft region, (4) correct the mandibular deviation and the canted occlusal plane with facial asymmetry with 2-jaw surgery, and (5) establish a stable, functional occlusion.
Treatment objectives
The patient was diagnosed with an Angle Class III malocclusion with skeletal Class I, facial asymmetry with a canted occlusal plane, and BCLP. Based on the diagnostic records and consultation with the patient, the following objectives were developed: (1) reconstruct the alveolar defects by bone grafting, (2) reposition the premaxilla by osteotomy to reduce the size of the alveolar defects and improve the retroclined maxillary incisors, (3) transplant the maxillary left second premolar into the right cleft region, (4) correct the mandibular deviation and the canted occlusal plane with facial asymmetry with 2-jaw surgery, and (5) establish a stable, functional occlusion.
Treatment alternatives
The patient had an excessively wide alveolar bone defect with oronasal fistulae in the bilateral cleft regions. We considered the conventional treatment approach, which was to expand the posterior maxillary segments, procline the maxillary incisors with orthodontic treatment, and perform alveolar bone grafting. However, both alveolar defects were wider on the nasal side than on the oral side. Orthodontic maxillary expansion would lead to widening of the alveolar defects. We also considered multisegmented osteotomy of the maxilla, which would reposition the premaxillary segment, and performing alveolar bone grafting to correct the transverse occlusal cant simultaneously. However, this approach had risks, including poor blood flow to the maxilla. Therefore, we chose a step-by-step approach, consisting of combined premaxillary osteotomy and alveolar bone grafting, followed by 2-jaw surgery.
For orthodontic alignment of the maxillary arch after bone grafting, we considered 3 options.
- 1.
Extraction of the maxillary left lateral incisor with mesial movement of the maxillary left canine and first premolar, alignment of the lingually displaced maxillary left second premolar, and closure of the residual spaces of the cleft regions by retraction of the maxillary incisors.
- 2.
Tooth autotransplantation of the maxillary left second premolar to the right cleft region and crown restoration to repair the morphology of the maxillary left lateral incisor.
- 3.
Extraction of the maxillary left first molar under endodontic treatment with alignment of the lingually displaced maxillary left second premolar, closure of the residual space of the maxillary left first molar by mesialization of the maxillary left second molar, and closure of the spaces at the cleft regions by retraction of the maxillary incisors.
Among these options, we selected plan 2 because the grafted bone was maintained with sufficient height and width to serve as a recipient site for tooth autotransplantation. Plan 2 also required a shorter treatment period than the other plans and preserved the remaining teeth.
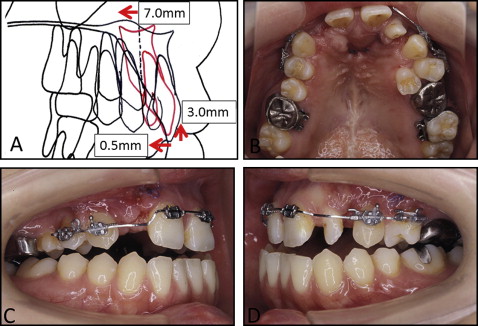
Treatment progress
Treatment was started by placing a modified transpalatal arch to expand the maxillary posterior segments. The transpalatal arch was fabricated with a hybrid soldered wire made of nickel-titanium and stainless steel (Dentsply-Sankin K.K., Tokyo, Japan). Fifteen months later, we performed a premaxillary osteotomy and bone grafting at the bilateral cleft region with cancellous bone harvested from the right iliac crest ( Fig 5 ). After maxillary expansion, the widths of the alveolar defects were 10 mm on the right side and 3 mm on the left side at the level of the alveolar crest, and 12.5 mm on the right side and 7.5 mm on the left side at the level of the nasal cavity. The premaxilla was set back for decreasing the excessively wide alveolar defects, and cancellous bone was grafted to the cleft regions: 5.1 g on the right side and 3.4 g on the left side.

Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


