The maxillary posterior edentulous region presents a challenge when planning for restoring missing teeth with a dental implant. The available bone in such cases is often not dense and not adequate for the placement of a properly sized implant because of maxillary sinus pneumatization and alveolar bone loss. Maxillary sinus lift is a predictable procedure to provide adequate bone height for the purpose of implant placement. However, complications are encountered during or after the execution of the sinus lift procedure. In this article, the prevention and management of maxillary sinus complications are discussed.
Key points
- •
Sinus augmentation is considered a successful procedure to provide adequate vertical bone augmentation in the maxillary posterior atrophic alveolar ridge for the placement of dental implant.
- •
Complications of maxillary sinus augmentation may occur during or after the surgical procedure.
- •
The most frequent intraoperative complication of maxillary sinus lift is perforation of the sinus membrane.
- •
The most common postoperative complication is sinus infection.
Introduction
Definition of Problem
A discussion of augmentation of the posterior maxilla is inadequate in view of therapeutic capabilities. Increasing the vertical dimension of bone alone should no longer be considered a successful treatment outcome. Rather, the clinician must look toward reconstruction of the posterior maxilla in a three-dimensional manner. Such reconstruction must have specific goals, which are attainable and address the multilevel concerns of both the clinician and the patient regarding comfort, function, aesthetics, and long-term predictability.
Sinus augmentation was once considered successful if adequate bone was present posttherapeutically for placement of at least a 10-mm-long implant. No consideration was given to the buccopalatal positioning of the implant, nor its diameter. The definitions of success often used after sinus augmentation, and subsequent implant placement and restoration, are flawed at best.
The surgical rehabilitation of the atrophic maxillary has been established as a predictable treatment. Several recent reviews have shown implant survival rates using lateral window and transcrestal techniques for sinus elevation surgery to be more than 95%. Jensen, in a review of 85 studies, reported survival rates for the rough-surfaced implants of 88.6% to 100%. These rates were found to be comparable with nongrafted sites.
The concept of implant success versus implant survival is still debated. Initially, all implants that attained osseointegration and fulfilled the criteria of Albrektsson and colleagues regarding immobility, lack of suppuration, or tissue inflammation, and so forth were considered successful. As has long been evident through a historical analysis of the development of knowledge, concepts once believed revolutionary become foundational building blocks on which to evolve a more nuanced understanding and outlook. Although the Albrektsson criteria were an invaluable starting point, such criteria do not assess the stability of bone on the buccal or palatal/lingual aspects of an implant.
Any discussion of implant success must include an implant assessment, which combines the Albrektsson and colleagues’ criteria with buccal and lingual/palatal bone assessment to ensure peri-implant marginal bone stability. Once these measurements are taken, the clinician can truly claim a successful implant therapeutic outcome. Such considerations are not purely semantic. To appropriately assess therapeutic efficacy in the long-term, criteria must be used that separate true success from mere survival. Unless the clinician is to assume the role of an actuarial, success is the only true goal.
As already mentioned, reconstruction of the posterior maxilla should always be viewed in a three-dimensional manner. Adequate bone must be present after regenerative efforts to place an implant in the ideal, prosthetically driven position. However, such a regenerative outcome is not in itself adequate. Although the concept of prosthetically driven implant placement is popular and well intentioned, it does not take into account the diameter of the tooth being replaced, or the fact that functional and parafunctional forces have their greatest effect on the peri-implant crestal bone. The greater the implant diameter, the greater the potential surface area of the osseointegrative bond at the crest of bone, to help better dissipate these forces. Therefore, buccopalatal/lingual regenerative efforts should be aimed at rebuilding adequate bone for prosthetically driven placement of an implant of the ideal diameter for the tooth being replaced ( Fig. 1 ). Of course, when such placement results in a thin patina of bone on the buccal or palatal/lingual aspect of the implant, treatment should not be deemed successful. The likelihood of this thin patina of bone resorbing under function over time is high. Such resorption results in significant compromise of the osseous support of the implant. Buccopalatal/lingual regeneration should be considered successful if the following criteria are met.
An implant of ideal dimensions for the tooth being replaced may be placed in a prosthetically driven position, and show a minimum of 2 mm of bone buccally and palatally/lingually at the osseous crest. Such a treatment result helps ensure long-term stability of the bony support of the implant under function. Another and most important criterion for success is a maximization of treatment outcomes in conjunction with a minimization of therapeutic insult to the patient. The most conservative treatment approach possible must always be used, assuming that the final treatment outcome is not compromised. A treatment approach that is easier or faster is of no use if the final treatment outcome is not equal in all respects to the therapeutic result after a more complex approach.
Treatment Options
When reconstructing the posterior maxilla, regenerative options include the following:
- a.
Lateral wall Caldwell-Luc sinus augmentation
- b.
Lateral wall Caldwell-Luc sinus augmentation in conjunction with buccal or palatal ridge augmentation
- c.
Trephine and osteotome use in anticipation of implant placement at a second stage
- d.
Trephine and osteotome use with simultaneous implant placement
- e.
Trephine and osteotome use followed by a second procedure of trephine and osteotome use, with simultaneous implant placement
Although complications may arise with any of these procedures, it is imperative to understand that an appropriate consideration of complications goes beyond surgical or postsurgical problems. Complications may occur before active therapy, during the surgical procedure, immediately after the surgical procedure, before implant loading, after implant loading, and after months or years of implant loading.
Pretreatment Evaluation
Complete medical, dental, social, and habit histories are required. The avoidance of complications must include addressing both absolute and relative contraindications. Absolute contraindications include systemic conditions such as radiation therapy, poorly controlled diabetes, hypertension, immune compromise, neoplasm, and associated polypharmacies. However, it is valuable to know that well-controlled type 2 diabetics have shown implant survival rates comparable with nondiabetics. Tawil and colleagues treated 45 well-controlled and fairly well-controlled (hemoglobin A 1c <7% vs 7%–9%) diabetic patients (143 implants) and 45 nondiabetic controls (142 implants) with classic protocol sinus elevation and bone grafting. Followed for 1 to 12 years the overall implant survival for the diabetic patients was 97.2% versus 98.8% for the nondiabetic control group.
Other significant risk factors for complications include active periodontitis, active sinusitis, large cysts, and history of chronic sinus disease. Active periodontics has been shown to reduce the survival rates for dental implants and, prospectively, even if successfully treated, as a risk for peri-implantitis. Acute or chronic sinusitis must be resolved before sinus elevation. Brook suggested that 10% to 13% of maxillary sinusitis is attributable to odontogenic infection. Conventional dental and medical treatment should be undertaken to eliminate these factors.
Smoking is a relative risk factor and has been linked to reduced implant survival outcomes. In an 8-year follow-up study of 13,147 implants placed in 4316 patients, Busenlechner and colleagues, found a 3-fold failure rate in the smokers compared with nonsmokers. In a recent systematic review, Pjetursson and colleagues found that there was almost twice the rate of implant failures in smokers compared with nonsmokers.
Assuming a noncontributory medical history, a thorough clinical examination must be carried out to assess both the patient’s regenerative needs and the feasibility of performing the proposed regenerative therapy. An accurate assessment of the condition of the soft tissues, not only of the site to be regenerated but throughout the mouth, must occur. A full occlusal examination must also be carried out.
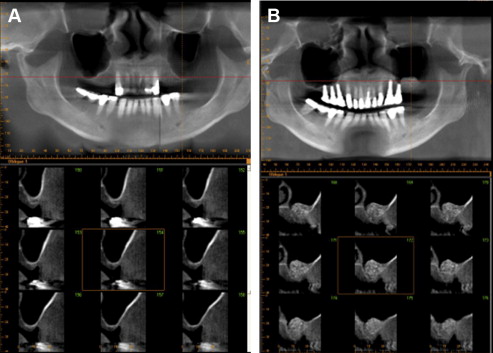
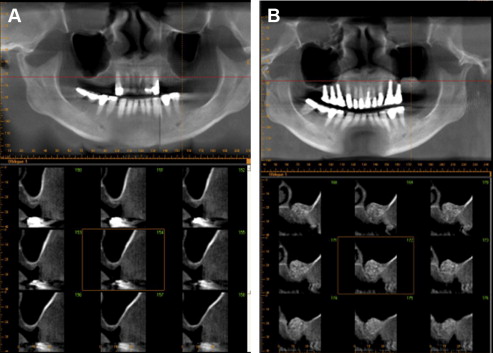
At the least, digital clinical photographs must be taken, including photographs in various lateral and protrusive positions. A formatted computed tomography (CT) scan is usually necessary in addition to properly angled individual digital radiographs, to assess the presence or absence of various diseases and the morphology of the site to be treated. Face bow mounted models are a key component in facilitating an accurate diagnosis and helping to formulate a comprehensive treatment plan. In addition, face bow mounted models allow for fabrication of regenerative and implant placement stents, to help guide the clinician in assessing regenerative needs, and thus rebuilding the necessary hard and soft tissues.
Failure to perform a thorough examination and accomplish a comprehensive diagnosis often lead to either use of a less than ideal surgical approach, selection of an inappropriate restorative modality, postoperative complications, or implant loss after restoration and varying lengths of time in function. In addition, failure to identify either the etiologic factors, or cofounding factors that must be managed to ensure long-term maximization of treatment outcomes, compromises patient care. For example, an undiagnosed parafunctional habit often leads to loss of bony support around implants under function and a poorer prognosis.
All treatment plans must be grounded in biological principles and therapeutic possibilities. Such treatment plans must strive to attain the most optimal treatment outcomes possible with the available technologies and techniques. To do so, the treating clinician(s) must constantly visualize ideal treatment outcomes and strive to attain them. For example, the determination of whether or not buccal or palatal ridge augmentation therapy is necessary should be based on neither specific clinician’s limitations nor manufacturer’s claims. Rather, an implant of the ideal diameter for the tooth being replaced must be able to be inserted in a restoratively driven position and show 2 mm of bone buccally and palatally, at the alveolar crests.
Introduction
Definition of Problem
A discussion of augmentation of the posterior maxilla is inadequate in view of therapeutic capabilities. Increasing the vertical dimension of bone alone should no longer be considered a successful treatment outcome. Rather, the clinician must look toward reconstruction of the posterior maxilla in a three-dimensional manner. Such reconstruction must have specific goals, which are attainable and address the multilevel concerns of both the clinician and the patient regarding comfort, function, aesthetics, and long-term predictability.
Sinus augmentation was once considered successful if adequate bone was present posttherapeutically for placement of at least a 10-mm-long implant. No consideration was given to the buccopalatal positioning of the implant, nor its diameter. The definitions of success often used after sinus augmentation, and subsequent implant placement and restoration, are flawed at best.
The surgical rehabilitation of the atrophic maxillary has been established as a predictable treatment. Several recent reviews have shown implant survival rates using lateral window and transcrestal techniques for sinus elevation surgery to be more than 95%. Jensen, in a review of 85 studies, reported survival rates for the rough-surfaced implants of 88.6% to 100%. These rates were found to be comparable with nongrafted sites.
The concept of implant success versus implant survival is still debated. Initially, all implants that attained osseointegration and fulfilled the criteria of Albrektsson and colleagues regarding immobility, lack of suppuration, or tissue inflammation, and so forth were considered successful. As has long been evident through a historical analysis of the development of knowledge, concepts once believed revolutionary become foundational building blocks on which to evolve a more nuanced understanding and outlook. Although the Albrektsson criteria were an invaluable starting point, such criteria do not assess the stability of bone on the buccal or palatal/lingual aspects of an implant.
Any discussion of implant success must include an implant assessment, which combines the Albrektsson and colleagues’ criteria with buccal and lingual/palatal bone assessment to ensure peri-implant marginal bone stability. Once these measurements are taken, the clinician can truly claim a successful implant therapeutic outcome. Such considerations are not purely semantic. To appropriately assess therapeutic efficacy in the long-term, criteria must be used that separate true success from mere survival. Unless the clinician is to assume the role of an actuarial, success is the only true goal.
As already mentioned, reconstruction of the posterior maxilla should always be viewed in a three-dimensional manner. Adequate bone must be present after regenerative efforts to place an implant in the ideal, prosthetically driven position. However, such a regenerative outcome is not in itself adequate. Although the concept of prosthetically driven implant placement is popular and well intentioned, it does not take into account the diameter of the tooth being replaced, or the fact that functional and parafunctional forces have their greatest effect on the peri-implant crestal bone. The greater the implant diameter, the greater the potential surface area of the osseointegrative bond at the crest of bone, to help better dissipate these forces. Therefore, buccopalatal/lingual regenerative efforts should be aimed at rebuilding adequate bone for prosthetically driven placement of an implant of the ideal diameter for the tooth being replaced ( Fig. 1 ). Of course, when such placement results in a thin patina of bone on the buccal or palatal/lingual aspect of the implant, treatment should not be deemed successful. The likelihood of this thin patina of bone resorbing under function over time is high. Such resorption results in significant compromise of the osseous support of the implant. Buccopalatal/lingual regeneration should be considered successful if the following criteria are met.
An implant of ideal dimensions for the tooth being replaced may be placed in a prosthetically driven position, and show a minimum of 2 mm of bone buccally and palatally/lingually at the osseous crest. Such a treatment result helps ensure long-term stability of the bony support of the implant under function. Another and most important criterion for success is a maximization of treatment outcomes in conjunction with a minimization of therapeutic insult to the patient. The most conservative treatment approach possible must always be used, assuming that the final treatment outcome is not compromised. A treatment approach that is easier or faster is of no use if the final treatment outcome is not equal in all respects to the therapeutic result after a more complex approach.
Treatment Options
When reconstructing the posterior maxilla, regenerative options include the following:
- a.
Lateral wall Caldwell-Luc sinus augmentation
- b.
Lateral wall Caldwell-Luc sinus augmentation in conjunction with buccal or palatal ridge augmentation
- c.
Trephine and osteotome use in anticipation of implant placement at a second stage
- d.
Trephine and osteotome use with simultaneous implant placement
- e.
Trephine and osteotome use followed by a second procedure of trephine and osteotome use, with simultaneous implant placement
Although complications may arise with any of these procedures, it is imperative to understand that an appropriate consideration of complications goes beyond surgical or postsurgical problems. Complications may occur before active therapy, during the surgical procedure, immediately after the surgical procedure, before implant loading, after implant loading, and after months or years of implant loading.
Pretreatment Evaluation
Complete medical, dental, social, and habit histories are required. The avoidance of complications must include addressing both absolute and relative contraindications. Absolute contraindications include systemic conditions such as radiation therapy, poorly controlled diabetes, hypertension, immune compromise, neoplasm, and associated polypharmacies. However, it is valuable to know that well-controlled type 2 diabetics have shown implant survival rates comparable with nondiabetics. Tawil and colleagues treated 45 well-controlled and fairly well-controlled (hemoglobin A 1c <7% vs 7%–9%) diabetic patients (143 implants) and 45 nondiabetic controls (142 implants) with classic protocol sinus elevation and bone grafting. Followed for 1 to 12 years the overall implant survival for the diabetic patients was 97.2% versus 98.8% for the nondiabetic control group.
Other significant risk factors for complications include active periodontitis, active sinusitis, large cysts, and history of chronic sinus disease. Active periodontics has been shown to reduce the survival rates for dental implants and, prospectively, even if successfully treated, as a risk for peri-implantitis. Acute or chronic sinusitis must be resolved before sinus elevation. Brook suggested that 10% to 13% of maxillary sinusitis is attributable to odontogenic infection. Conventional dental and medical treatment should be undertaken to eliminate these factors.
Smoking is a relative risk factor and has been linked to reduced implant survival outcomes. In an 8-year follow-up study of 13,147 implants placed in 4316 patients, Busenlechner and colleagues, found a 3-fold failure rate in the smokers compared with nonsmokers. In a recent systematic review, Pjetursson and colleagues found that there was almost twice the rate of implant failures in smokers compared with nonsmokers.
Assuming a noncontributory medical history, a thorough clinical examination must be carried out to assess both the patient’s regenerative needs and the feasibility of performing the proposed regenerative therapy. An accurate assessment of the condition of the soft tissues, not only of the site to be regenerated but throughout the mouth, must occur. A full occlusal examination must also be carried out.
At the least, digital clinical photographs must be taken, including photographs in various lateral and protrusive positions. A formatted computed tomography (CT) scan is usually necessary in addition to properly angled individual digital radiographs, to assess the presence or absence of various diseases and the morphology of the site to be treated. Face bow mounted models are a key component in facilitating an accurate diagnosis and helping to formulate a comprehensive treatment plan. In addition, face bow mounted models allow for fabrication of regenerative and implant placement stents, to help guide the clinician in assessing regenerative needs, and thus rebuilding the necessary hard and soft tissues.
Failure to perform a thorough examination and accomplish a comprehensive diagnosis often lead to either use of a less than ideal surgical approach, selection of an inappropriate restorative modality, postoperative complications, or implant loss after restoration and varying lengths of time in function. In addition, failure to identify either the etiologic factors, or cofounding factors that must be managed to ensure long-term maximization of treatment outcomes, compromises patient care. For example, an undiagnosed parafunctional habit often leads to loss of bony support around implants under function and a poorer prognosis.
All treatment plans must be grounded in biological principles and therapeutic possibilities. Such treatment plans must strive to attain the most optimal treatment outcomes possible with the available technologies and techniques. To do so, the treating clinician(s) must constantly visualize ideal treatment outcomes and strive to attain them. For example, the determination of whether or not buccal or palatal ridge augmentation therapy is necessary should be based on neither specific clinician’s limitations nor manufacturer’s claims. Rather, an implant of the ideal diameter for the tooth being replaced must be able to be inserted in a restoratively driven position and show 2 mm of bone buccally and palatally, at the alveolar crests.
Sinus anatomy
Any discussion of treatment of complications related to sinus elevation procedures must include sinus anatomy. The maxillary sinus is a pyramidal cavity, volume of 12 to 15 mL, contained within the maxillary bone. It is bounded superiorly by the orbital floor, inferiorly by the alveolar process, medially by the lateral nasal wall, and laterally by the zygomatic process and buccal alveolus. The sinus is lined with a thin layer of mucoperiosteum, the Schneiderian membrane, of variable thickness, with an average of approximately 1.0 mm. The sinus drains medially and superiorly into the nasal cavity via the ostium. The maxillary artery and nerve provide blood supply and innervation. The posterior superior branch of the maxillary artery may pass through the area of the posterior lateral window preparation, with average distance from the artery to the alveolar crest 16.9 mm. However, this distance has been found to be as little as 11.25 ± 2.99 mm (standard deviation) mean vertical distance from the lowest point of the bony canal to the alveolar crest.
Complications after various treatment approaches
Complications may be divided into intraoperative and postoperative events, and they may be interrelated ( Table 1 ).
| Article | Aim | Materials | Criteria | Results | Conclusion |
|---|---|---|---|---|---|
| Maxillary sinus functions and complications with lateral window and osteotome sinus floor elevation procedures, followed by dental implants placement: a retrospective study in 60 patients | Evaluate maxillary sinus functions and complications by using lateral window and osteotome sinus floor elevation then implants placement | 60 patients sinus floor elevation using lateral window with residual subsinus alveolar bone height (RSABH) of 3 mm and osteotome with RSABH of >4 mm No bone grafting with osteotome procedures followed by implants (ITI implants) Implants were placed immediately at time of lateral window, or after 9 mo using surgical guides Bio-Oss graft was used with lateral window Retrospectively evaluated clinically and radiographically for 24 mo |
Dizziness Nausea Sinus membrane perforation |
More dizziness and nausea with osteotome than lateral window, which disappeared within 2–4 wk 4 of 79 sinus perforation cases (2 osteotome and 2 lateral window) |
No obvious maxillary sinus complications for 24 mo after sinus floor elevation using osteotome and lateral window, followed by implants placement Clinical assessment of individual risk and modifying factors before procedures |
| A retrospective study of the effects on sinus complications of exposing dental implants to the maxillary sinus cavity | Investigate whether dental implant exposure to the maxillary sinus cavity increased the risk of maxillary sinus complications | 9 patients 23 implants inserted into the maxillary sinus >4 mm No sinus membrane lift 6–10 mo evaluation using questionnaire and CT Astra implants and 1 Osstem implant used |
Nasal congestion Obstruction Pathologic secretion Pain and tenderness in the sinus region |
No clinical signs of sinusitis CT scans showed postoperative sinus mucus thickening around 14 of the 23 implants |
This study showed that implant exposure to the maxillary sinus cavity can cause sinus mucus thickening around the implants Implant exposure to the sinus cavity might contribute to the development of maxillary sinusitis in patients with a predisposition for sinusitis Implant extension into the nasal cavity can give rise to rhinosinusitis (Raghoebar and colleagues) |
| A case of massive maxillary sinus bleeding after dental implant | A case of maxillary sinus bleeding during dental implant | Maxillary sinus osteoplasty with a vascularized pedicled bone flap through a maxillary sinus approach General anesthesia |
Signs of posterior nasal bleeding Swelling of the gingival 1 d after admission, the bleeding was not controlled Hemoglobin level measured 7.1 g/dL |
The patient was discharged 3 d after surgery, and 6 mo after surgery, there were no signs of rebleeding with normal use of the dental implant | Surgery is needed in cases in which nasal bleeding is not conservatively controlled Cauterization of the bleeding site using a nasal endoscope is the most common operative technique Vascularized pedicled bone flap allows a shorter length of hospital stay and fewer outpatient clinic visits because it causes minimal swelling of the isthmus and minimal injury to the maxillary mucosa |
| Fungal infection as a complication of sinus bone grafting and implants: a case report | Report a case of a middle-aged male patient along with the clinical, radiographic, and histologic findings | 48-y-old man 10 cigarettes/d Failed sinus bone grafting (irradiated cancellous bone) and osseointegration of implants (Nobel Biocare), which were placed after 6 mo of sinus graft Surgical exposure of the maxillary sinus Systemic prophylactic antibiotics used Removal of infected bone graft Sinus membrane elevation Perforation sealed with bioresorbable membrane and fibrin glue (to stabilize the membrane) Demineralized bone matrix paste with cancellous bone was grafted into the sinus and covered by Tutoplast pericardium Postoperative systemic antibiotics, nonsteroidal antiinflammatory drugs for 10 d and antifungal drug Implants placed after 8 mo |
Increased radiopacity of the right maxillary sinus Sphere-shaped foreign body mass composed of dark brown and red material curetted from maxillary sinus Caused by Aspergillus and polypous mucosa |
Newly grafted allograft in the sinus showed no specified inflammation or fungal hyphae | First case report of fungal sinusitis that developed after maxillary sinus bone grafting followed by implant placement Surgical treatment of noninvasive fungal sinusitis produced good results, and no recurrence was observed |
| Oroantral communication as an osteotome sinus elevation complication | Case report of an oroantral communication that developed as a complication to a sinus elevation surgery performed with the crestal approach | 54-year-old woman History of sleep apnea and smoking (1 pack/d) Patient has a bridge from 2 to 4 with missing 3 Extraction of tooth 2 and freeze-dried bone allograft socket preservation After 3 mo, exploratory surgery was performed Amoxicillin and methylprednisolone for 7 d before surgery There were no bone fills inside the socket Freeze-dried bone allograft mixed with platelet-rich plasma to elevate the sinus using osteotome over tooth 3 space Collagen membrane used Postoperative instructions and chlorhexidine 0.12% used |
6 d later the patient returned to the clinic and claimed the surgical site had “opened up” Water coming through her nose while drinking The sutures were broken and the flaps open |
De-epithelization of buccal and lingual flaps, and rotating buccal flap mesially, to cover the site Postoperative instructions, and patient instructed to stop using continuous positive airway pressure mask Patient was followed every 2 wk for 2 mo, and the area appeared to be healed, with complete closure by the end of the first month After 4 y, patient presented with normal healing, no smoking, and a new lateral window sinus lift was performed to restore 4 successfully |
Use of a positive pressure mask may have complicated a sinus elevation surgery. Other factors that may have contributed to this complication include smoking and delayed healing of the area |
| Potential adverse events of endosseous dental implants penetrating the maxillary sinus: long-term clinical evaluation | Evaluate the nature and incidence of long-term maxillary sinus Adverse events related to endosseous implant placement with protrusion into the maxillary sinus |
70 patients with 83 implants placed into maxillary sinus (<3 mm) with membrane perforation Minimum of 5 y follow-up Perioperative prophylactic clindamycin Straumann implants were placed after 1-stage procedure Postoperative antibiotics for 4 d Prosthetic rehabilitation after osseointegration from 2–6 mo |
Clinical and radiographic assessment monitoring signs of sinusitis, and by asking the patients about any symptoms, including nasal bleeding, congestion or obstruction, nasal secretion, and pain or tenderness in the infraorbital region | 12 patients had >1 implant penetrating the sinus 7 had bilateral perforation Implants were localized in premolar/molar area 2/83 implants diagnosed with peri-implantitis were treated without recurrence Radiologic follow-up showed a normal bone healing process in all patients |
No sinus complication was observed after implant penetration into the maxillary sinus (≤20 y) Absence of complications was related to maintenance of successful osseointegration |
| The management of complications after displacement of oral implants in the paranasal sinuses: a multicenter clinical report and proposed treatment protocols | Study retrospectively analyzed paranasal sinus complications after displacement of oral implants in the maxillary sinus treated according to clinical situation by functional endoscopic sinus surgery (FESS), an intraoral approach, or a combination of both procedures | 27 patients (13 male; 14 female) Age: 27–73 y More than 5 y treatment of complications involving the paranasal sinuses after displacement of oral implants in the maxillary sinuses Patients were treated with FESS (functional endoscopic sinus surgery), intraoral approach to the sinus, or FESS associated with an intraoral approach |
Implant displacement Implant displacement with or without reactive sinusitis or with or without associated oroantral communication |
26 patients recovered completely 1 patient underwent reintervention with FESS and an intraoral approach 2 y after implant removal followed by complete recovery |
The results show that a rational choice of surgical protocol for the treatment of complications involving the paranasal sinuses after displacement of implants in the maxillary sinuses may lead to reliable results |
| Effect of Schneiderian membrane perforation on posterior maxillary implant survival | To assess the survival rate of implants placed in the posterior maxilla by intentionally perforating the Schneiderian membrane and protruding the implant up to 3 mm beyond the sinus floor in cases of reduced crestal bone height | 56 patients with 63 implants intentionally penetrated the Schneiderian membrane engaging sinus floor cortical bone (Nobel Biocare) Implants were placed using 2-stage technique 1 y follow-up after implant restoration (12–14 wk) Postoperative antibiotics |
1 implant failure 7 patients experienced mild epistaxis during the immediate postoperative period, with no associated implant loss 1 patient developed sinusitis secondary to the surgical procedure, which was treated by antibiotic therapy and the patient improved clinically, with no associated implant loss |
Intentional perforation of the Schneiderian membrane using a 2-mm twist drill at the time of implant placement and protrusion of the implant up to 3 mm beyond the sinus floor does not alter the stability and outcome of dental implants, 1 y after restoration | |
| Transcrestal sinus floor elevation with osteotomes: simplified technique and management of various scenarios | Understand the structure of the maxillary sinus region Describe a simplified transcrestal sinus floor elevation technique Manage issues and factors that may be encountered when performing a sinus floor elevation |
Implant success rate after osteotome sinus lift is 90.9%–92.8% Septa are present 31.7% at premolar area Pneumatization of the sinus occurs within 6 mo after tooth extraction <4 mm of bone subantral then a lateral window is recommended >5 mm of bone is needed to place an implant with osteotome sinus lift If only 4 mm of bone is present, then implant needs to be submerged under the gum >4 mm of subantral bone leads to 96% survival rate compared with only 84.7% when bone is <4 mm Simplified osteotome technique: used for medium and soft dense bone Assume there is only 4 mm subantral bone Using Straumann system and the corresponding osteotome Periapical radiograph is taken, for subantral bone determination considering 14% error 2-mm drill used till 1 mm short of the subantral floor Guide pin insertion Then subsequent drills are used to widen the osteotomy An osteotome corresponding to the last drill is used to upfracture the sinus floor A metal stop is placed on the osteotome at 4 mm in this case and the tip of osteotome is dipped in saline Few gentle malleting taps facilitate the infracture Some hemorrhage occurs once penetrating the sinus floor Bone graft material could be used before infracture to act as cushion, although might reduce the tactile perception After placing bone grafting material in the osteotomy, using an amalgam carrier, the same osteotome is used to push the bone substitute and elevate the membrane This provides 2 mm of bone height Repeat till desired length is reached Bone forms at the sinus floor at a rate of 1 mm Slanted sinus floor: Drill is stopped 1 mm short of the most inferior sinus wall Drills are increased in size normally, then, a small osteotome is used angled toward the thicker bone to break the bone Any sinus perforation should be verified using the Valsalva maneuver Some clinicians recommend abortion and healing for 4 wk, then, redoing the procedure Implant platform should be placed supracrestal when there is minimum subantral bone to achieve supracrestal biological width |
Complications: most frequently encountered complication is Schneiderian Membrane perforation (38%) Infection 0.8% In case of extensive malleting, postoperative headache or benign paroxysmal positional vertigo can occur |
Simplified technique to perform sinus floor elevation in medium dense bone has been presented Enhances patient comfort and reduces the need to mallet osteotomes |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


