Introduction
We compared the effectiveness of 2 canine retraction springs and anchorage systems (direct and indirect skeletal anchorage) in patients requiring first premolar extractions and maximum anchorage in the maxilla.
Methods
Thirty-six patients were included (17 male, 19 female; mean age, 16.8 ± 2.4 years). A mini-implant–supported Nance appliance with indirect skeletal anchorage system was used in 18 patients and a mini-implant–supported direct skeletal anchorage system in the remaining patients. In each patient, a segmental retraction arch with a reverse closing loop was applied to a maxillary canine, and a Ladanyi spring (Dentaurum, Ispringen, Germany) was applied to the other canine randomly after extraction of the maxillary first premolars. The retraction process was continued until a Class I canine relationship was obtained. Lateral cephalometric films and orthodontic casts taken before and after retraction in the distalization process were used to evaluate changes during canine distalization. The measurements were statistically evaluated using paired and independent t tests with 95% confidence intervals.
Results
The reverse closing loop and the Ladanyi spring were found to be effective in canine distalization ( P ≤0.001). There were no statistically significant differences between the reverse closing loop and the Ladanyi spring with regard to canine distalization rates ( P ≥0.05). Both systems were effective in providing maximum anchorage ( P ≥0.05); no statistically significant differences were detected in molar anchorage loss rates between the 2 methods ( P ≥0.05).
Conclusions
These 2 systems can be used during segmental distalization of canines requiring maximum anchorage with no significant anchorage loss.
Highlights
- •
Orthodontic mini-implants provide direct or indirect skeletal anchorage.
- •
Indirect systems are preferred in patients with proximity of the roots.
- •
MaxVP-U6 did not differ in the skeletal anchorage and spring groups.
- •
Retraction speed did not differ in the retraction and skeletal anchorage groups.
- •
Total tooth movement did not differ in the retraction and skeletal anchorage groups.
Loss of anchorage is a common problem faced during maximum anchorage orthodontic treatment, and prevention of this plays a significant role in the design of the orthodontic appliances. For a patient with a Class II occlusion, if the treatment plan is the extraction of the premolars, the maxillary canines must be distalized completely to the extraction sites. Therefore, anchorage reinforcement of the posterior teeth must be ensured using intraoral or extraoral appliances.
Previously, extraoral appliances were the only way to provide maximum anchorage, but their use was limited because they required patient cooperation. As a result, intraoral appliances became increasingly popular among clinicians for obtaining anchorage. However, popular intraoral appliances, such as palatal and lingual bars, Nance appliances, and intermaxillary elastics, have undesired side effects: protrusion, extrusion, and tipping.
Anchorage problems encountered during the use of intraoral mechanics led to increased use of implant-borne mechanics. However, these had several limitations, such as excessive waiting times for osseointegration. These limitations were prevented by the introduction of orthodontic mini-implants as intraoral anchorage units. These implants were developed as an alternative to conventional molar and other intraoral anchorage units.
Orthodontic mini-implants can be used either directly or indirectly. Direct anchorage refers to the movement of teeth using orthodontic mini-implants, whereas indirect anchorage refers to the stabilization of certain teeth in the dental arch and subsequent use of these stabilized anchors to move other teeth. Indirect skeletal anchorage systems are preferred by clinicians when the direct skeletal anchorage system is not applicable, such as in patients with proximity of the roots.
In extraction patients, canine retraction can be carried out with fixed appliances using frictional or nonfrictional methods. The popularity of the nonfrictional method increased when Burstone reported its advantages. Thereafter, many canine retraction springs were introduced and tested for reliability and efficiency.
The aim of this study was to compare the efficiency of direct and indirect skeletal anchorage systems combined with 2 canine retraction springs in patients requiring maximum anchorage for maxillary canine retraction.
Material and methods
After receiving ethical approval from the ethics council of Karadeniz Technical University (protocol number, B302KTU0200000/637), we conducted a pilot study to calculate the total sample size. Twenty patients were recruited for the pilot study at the beginning of the treatment, and a number from 1 to 20 was assigned to each patient. Using a randomization Web site, 4 columns of the random array of numbers were created. According to the 4 randomized number strings, patients were assigned to the following groups: (1) direct skeletal anchorage, Ladanyi spring (LS) (Dentaurum, Ispringen, Germany) on the left side; (2) direct skeletal anchorage, LS on the right side; (3) indirect skeletal anchorage, LS on the left side; and (4) indirect skeletal anchorage, LS on the right side. After randomization, the canine distalization method was applied to every patient according to the patient’s assigned group. As the distalization finished, all cephalometric and cast materials were measured, and the power of the study was determined. Meanwhile, we continued to recruit new patients for the study. According to our pilot study, power calculations with G*Power (version 3.1.3; Franz Faul, Christian-Albrechts-Universitat, Kiel, Germany), group sample sizes of 16 achieved 82% power to detect a difference of 1.5mm between the null hypothesis that both group means were 1.7mm and the alternative hypothesis that the mean of group 2 was 0.1mm, with estimated group standard deviations of 1.2mm and 1.7mm at a significance level (alpha) of 0.05 using a 2-sided, 2-sample t test. Thus, 16 additional patients were recruited to guarantee the exact power with a total of 36 patients (17 male, 19 female; mean age, 16.8 ± 2.4 years). The aforementioned randomization method was applied to these patients as well.
Patients receiving maximum anchorage with extraction of the maxillary first premolars were included in the study. The inclusion criteria were (1) permanent dentition, (2) good oral hygiene, (3) Class I or Class II skeletal pattern, (4) no anomaly in the transverse direction, (5) no maxillary canine with supraposition or excessive rotation, (6) no systemic disorder that contraindicated orthodontic treatment, and (7) no systemic or allergic disorder that contraindicated the application of skeletal anchorage units.
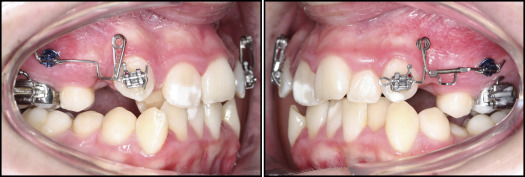
The maxillary first premolars were extracted to resolve the crowding in all patients. In the direct skeletal anchorage group, 2 mini-implants (Aarhus; American Orthodontics, Sheboygan, Wis; 1.5-mm diameter, 8-mm length) were inserted into the buccal aspect between the roots of the maxillary first molars and second premolars at an angle of 15° to 20°. In the indirect skeletal anchorage group, after determination of the insertion areas using cephalometric radiographs and dental casts, 2 of the same mini-implants were inserted into the paramedian section of the palatal area ( Fig 1 ).
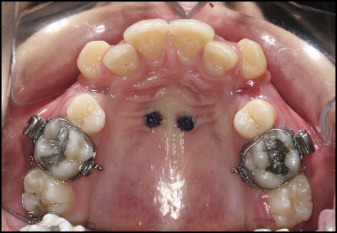
Appropriate molar bands (3M Unitek, Monrovia, Calif) were chosen and adapted to the maxillary molars. After the construction of banded casts of the maxilla, custom Nance appliances were built over the mini-implant sites ( Fig 2 ).

Guide wires, made from 0.021 × 0.025-in stainless steel wires (American Orthodontics), were used for assessing the movements of the teeth on cephalometric radiographs ( Fig 3 ). In both groups, 0.022 × 0.028-in slotted Roth brackets (Gemini; 3M Unitek) were bonded to the maxillary canines before application of these wires. Guide wires with rounded ends were applied to the right canines and molars, and wires with straight ends were applied to the left canines and molars in all patients. Lateral cephalometric radiographs were taken after installation of the wires before and after the canine distalization process.
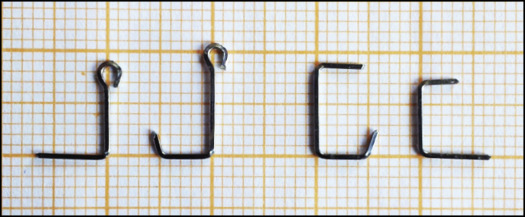
Remaloy wires (Dentaurum, Ispringen, Germany), 0.016 × 0.022 in diameter, were used to prepare the reverse closing loop (RCL) retraction springs. The RCL retraction springs were given the same dimensions as the prefabricated LS to obtain standardization, and 45° antitip and 15° to 20° antirotation bends were incorporated into the springs before installation. Additional step bends were also included in the springs of the direct skeletal anchorage groups to prevent intrusion of canines because of differences in the vertical levels of the mini-implants and the canine bracket slots ( Fig 4 ). The application of the retraction springs was completed by activating each spring by about 2 mm to obtain 120 to 150 g of retraction force. Prefabricated LS were applied on 1 side, and RCL retractor springs were applied to the other side of the patients randomly.
The retraction springs were activated at 4-week intervals, and the retraction process was continued until the canines achieved a Class I relationship.
The ANS-PNS line extended from the anterior nasal spine (ANS) to the posterior nasal spine (PNS) along the maxillary plane (MaxP). Local superimpositions were carried out along this line and at the PNS point. MaxP, derived from the ANS-PNS points, was used as a horizontal reference plane, and MaxVP, derived from the vertical line extending from the pterygomaxillary fissure to the MaxP, was used as the vertical reference plane for dental changes ( Fig 5 , B ).
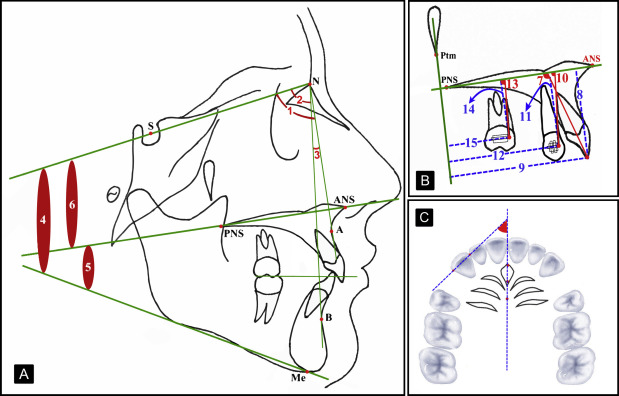
The mesial and distal contact points of the canines were marked on the dental casts and transferred to the computer via a scanner (Perfection V700; Epson America, Long Beach, Calif). Digital images were then transferred to cephalometric tracing software (Facad, trial version; Ilexis, Linköping, Sweden), and the amounts of predistalization to postdistalization rotation of the canines were measured ( Fig 5 , C ).
Statistical analysis
The measurements were then analyzed using SSPS software (version 15.0; SPSS, Chicago, Ill). Kolmogorov-Smirnov tests indicated approximately normal distributions, and paired t tests and independent-sample t tests were used to compare the intragroup and intergroup changes.
Three weeks after the first evaluation, the tracings and measurements were repeated by the same investigator (S.O.) on 15 preretraction and 15 postretraction lateral cephalograms as well as 15 dental models of randomly selected patients. The intraclass correlation coefficients ( r ) were calculated for each variable to assess the reliability of the measurements, and they ranged from 0.967 to 1.00.
Results
In the cephalometric findings, although there were no statistically significant changes in skeletal measurements, there were significant reductions in the values representing protrusion of the incisors ( Table I ; Fig 5 , A ).
| Variable | Direct skeletal anchorage group | Indirect skeletal anchorage group | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| T1 | T2 | P | T1 | T2 | P | |||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |||
| Skeletal | ||||||||||
| SNA (°) | 79.46 | 4.03 | 79.55 | 4.22 | 0.423 | 80.66 | 2.50 | 80.64 | 2.67 | 0.829 |
| SNB (°) | 76.07 | 4.37 | 75.96 | 4.29 | 0.546 | 76.03 | 2.22 | 75.81 | 1.94 | 0.093 |
| ANB (°) | 3.44 | 2.56 | 3.59 | 2.83 | 0.432 | 4.65 | 1.79 | 4.83 | 1.75 | 0.102 |
| SN/ManP (°) | 36.56 | 5.54 | 36.55 | 5.32 | 0.981 | 35.28 | 3.54 | 35.44 | 3.61 | 0.376 |
| MaxP/ManP (°) | 28.67 | 4.61 | 28.72 | 4.50 | 0.829 | 27.75 | 4.60 | 27.81 | 4.97 | 0.768 |
| SN/MaxP (°) | 7.88 | 2.92 | 7.89 | 2.92 | 0.855 | 7.54 | 3.95 | 7.63 | 3.91 | 0.035 ∗ |
| Wits (mm) | 3.11 | 3.49 | 3.12 | 3.93 | 0.969 | 5.45 | 3.30 | 5.06 | 2.35 | 0.466 |
| Dental | ||||||||||
| MaxP-U1a (°) | 115.90 | 9.59 | 113.60 | 9.80 | 0.001 ‡ | 111.28 | 8.44 | 109.59 | 7.77 | 0.009 † |
| MaxP-U1 (mm) | 28.02 | 2.36 | 27.97 | 2.36 | 0.705 | 28.76 | 3.29 | 28.65 | 3.50 | 0.531 |
| MaxVP-U1 (mm) | 51.32 | 5.68 | 50.51 | 5.14 | 0.008 † | 51.16 | 5.32 | 50.49 | 5.12 | 0.009 † |
There were no statistically significant changes in the value of MaxVP-U6, representing the horizontal distance from maxillary molars to the maxillary vertical plane ( Table II ), for all skeletal anchorage and spring groups.
| Direct skeletal anchorage group | Indirect skeletal anchorage group | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| T1 | T2 | P | T1 | T2 | P | |||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |||
| Reverse closing loop | ||||||||||
| MaxP/U3a (°) | 90.19 | 9.33 | 73.37 | 8.39 | 0.000 † | 82.78 | 8.86 | 67.12 | 9.18 | 0.000 † |
| MaxP-U3 (mm) | 21.12 | 3.28 | 20.40 | 3.06 | 0.078 | 23.04 | 3.60 | 23.44 | 3.57 | 0.318 |
| MaxVP-U3 (mm) | 46.30 | 3.67 | 39.79 | 4.38 | 0.000 † | 47.08 | 5.73 | 40.88 | 5.52 | 0.000 † |
| MaxP/U6a (°) | 80.06 | 9.06 | 80.64 | 8.73 | 0.534 | 77.47 | 6.54 | 77.84 | 6.44 | 0.145 |
| MaxP-U6 (mm) | 20.85 | 2.59 | 20.51 | 3.05 | 0.273 | 21.40 | 2.50 | 21.02 | 2.94 | 0.089 |
| MaxVP-U6 (mm) | 24.18 | 3.18 | 25.38 | 3.61 | 0.055 | 21.08 | 4.77 | 22.09 | 3.87 | 0.162 |
| Ladanyi spring | ||||||||||
| MaxP/U3a (°) | 84.28 | 7.75 | 68.04 | 9.00 | 0.000 † | 84.49 | 8.62 | 68.59 | 10.23 | 0.000 † |
| MaxP-U3 (mm) | 22.50 | 3.14 | 20.96 | 2.51 | 0.002 ∗ | 22.40 | 4.18 | 23.27 | 3.26 | 0.103 |
| MaxVP-U3 (mm) | 46.61 | 4.97 | 38.84 | 3.77 | 0.000 † | 46.36 | 5.05 | 40.33 | 5.62 | 0.000 † |
| MaxP/U6a (°) | 78.14 | 10.91 | 78.54 | 11.63 | 0.577 | 77.64 | 7.76 | 77.83 | 6.50 | 0.837 |
| MaxP-U6 (mm) | 20.84 | 3.06 | 20.27 | 2.61 | 0.100 | 21.44 | 2.77 | 21.39 | 2.77 | 0.847 |
| MaxVP-U6 (mm) | 24.29 | 4.17 | 24.32 | 3.23 | 0.967 | 21.15 | 4.28 | 22.05 | 4.13 | 0.117 |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


