Introduction
The purpose of this study was to determine the influence of self-tapping and self-drilling placement techniques on the stability of miniscrews.
Methods
We included 70 orthodontic patients who received miniscrews (140 screws). Miniscrews measuring 1.6 mm in diameter and 8 mm in length were placed using the self-tapping (35 patients, 70 screws) and self-drilling (35 patients, 70 screws) methods. We examined the success rates, placement torque values, Periotest (Medizintechnik Gulden, Bensheim, Germany) values, rates of root contact, and influence of root contact on mobility. Cone-beam computed tomography was used to evaluate root contact. Miniscrews that endured an orthodontic force for 6 months or more were considered successful.
Results
The success rates of the miniscrews were approximately 96% with either placement technique. The placement torques were 7 and 7.5 N cm in the self-tapping and self-drilling miniscrews, respectively ( P >0.05). The Periotest values of the self-drilling method were significantly greater than those of the self-tapping method. The Periotest values of the self-drilling miniscrews with root contact were significantly greater than those with no root contact.
Conclusions
Both placement techniques showed high stability in the maxillary bone, although the self-drilling miniscrews with root contact had greater mobility. Special attention to root contact further improves the stability of the self-drilling miniscrews.
Self-tapping miniscrews have been used as orthodontic anchorage devices. This miniscrew requires the preparation of a pilot hole before insertion; this is time-consuming and might result in drill-bit breakage and thermal necrosis of bone. On the other hand, the design of self-drilling miniscrews enables them to be inserted without drilling. Several animal studies have compared the 2 methods. With a dog model, Yadav et al demonstrated greater microdamage to the cortical bones of both the maxilla and the mandible using self-drilling compared with self-tapping, but they did not report the failure rate. Shank et al quantified the bone damage associated with the insertion of both types of miniscrews in dogs and found no difference in the damage parameters in the maxilla, which has similar conditions to human alveolar bone in terms of cortical bone thickness. Gupta et al evaluated the stability of self-tapping and self-drilling screws when used as anchorage units for en-masse retraction of maxillary anterior teeth; they demonstrated that both the self-tapping and the self-drilling screws were effective anchorage units. Moreover, they described the advantages of self-drilling screws, which included decreased operative time, little bone debris, less thermal damage, lower morbidity, and minimal patient discomfort because predrilling is not required. Thus, if both the self-tapping and the self-drilling methods result in placement with equal stability, then the self-drilling method should be preferred because of its clinical advantages. However, Park et al stated that self-drilling screws are not recommended for placement in dense and thick cortical bone such as the mandibular molar region; instead, the self-tapping method is preferred to prevent fracture of the screw or the bone. Thus, the self-drilling method might be preferred in thin cortical bone areas such as maxillary alveolar bone in interradicular spaces.
Placement, removal torque and the mobility of the screw are clinical indices of the stability of miniscrews. Miniscrew stability is thought to be related to overloading, inflammation, cortical bone thickness and bone density, screw design, and adjacent root proximity. Root proximity is an important risk factor because of its relationship with failure. Technical biases related to the self-tapping and self-drilling methods might affect root proximity.
The aim of this clinical trial was to identify the influences on miniscrew stability of the self-tapping and self-drilling placement techniques. To determine the differences between the self-tapping and self-drilling methods, we focused on (1) success rate, (2) placement torque, (3) mobility, (4) root contact frequency, and (5) the influence of root contact on mobility. In this study, 70 patients who received miniscrews were randomly selected and evaluated; 35 patients had the self-tapping method, and 35 had the self-drilling method. Placement torque was evaluated using a torque tester, mobility was measured with a Periotest device (Medizintechnik Gulden, Bensheim, Germany), and the placement sites were shown using cone-beam computed tomography (CBCT).
Material and methods
This study included 70 orthodontic patients from 2010 to 2011 who received miniscrews (140 screws) in the maxillary buccal alveolar bone between the second premolar and the first molar. All miniscrews were used as anchors for anterior retraction for first premolar extractions. The subjects were randomly divided into 2 groups: the first group comprised 35 patients (25 female, 10 male; average age, 23.2 ± 7.7 years) who had self-tapping for miniscrew placement, and the second group comprised 35 patients (24 female, 11 male; average age, 22.3 ± 7.4 years) who had self-drilling. This study was approved by the ethical review board of Nihon University School of Dentistry, Tokyo, Japan, and all patients consented to participate.
All patients received miniscrews of the same design, measuring 1.6 mm in diameter and 8 mm in length (ISA self-drill type anchor screw; Biodent, Tokyo, Japan) to prevent any effects of screw design ( Fig 1 ). In the self-tapping group, after administration of local anesthesia, a pilot hole (1.0-mm diameter, 8.0-mm length) was drilled using a bone drill under physiologic saline solution flow into the buccal alveolar bone in an area of keratinized gingiva between the second premolar and the first molar of the maxilla. In the self-drilling group, local anesthesia was administered, and the miniscrews were placed with no pilot hole. The sole difference was whether there was a pilot hole, and no punch or incision of the surrounding gingiva was made in either method. To reduce the likelihood of root contact, the miniscrew was placed so that it inclined 45° to 60° vertically with respect to the adjacent tooth axis and was perpendicular horizontally to the bone surface. Examiners (Y.U. and S.S.) measured the maximum placement torque during terminal rotation of all miniscrews using a torque tester (DIS-RL05; nominal accuracy, ±0.5%; Sugisaki Meter, Tokyo, Japan) and recorded the mobility (Periotest value) using the Periotest device after placement.

Miniscrew mobility has been assessed with the Periotest and Osstell devices. The Periotest is used to assess the damping capacity, and the Osstell uses resonance frequency. The Osstell instrument requires a SmartPeg attachment containing a magnet. Because SmartPeg modification and the use of miniscrews with inner screw threads would have been difficult in this study, we used the Periotest device. A greater Periotest value indicated more mobility.
For each screw, Periotest values were obtained by holding the tip of the handpiece parallel to the bone surface according to the manufacturer’s instructions. Each measurement was repeated 3 times, and the average value was calculated. Immediately after placement, an orthodontic force of approximately 2 N was applied to the miniscrews, and CBCT (3D Accuitomo; J. Morita, Kyoto, Japan) imaging for each subject was performed for postplacement diagnosis. All miniscrews were used as anchors for orthodontic treatment at Nihon University School of Dentistry Dental Hospital, Tokyo, Japan. Each patient was prescribed an antibiotic for 3 days after placement to control infection.
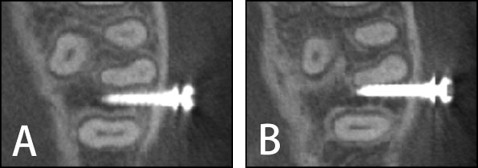
The following parameters were used for CBCT diagnostic imaging of the placement site: field of view of 60 × 60 mm, voxel size of 0.125 mm 3 in super high-resolution mode, x-ray tube voltage of 80 kV, and current of 5.5 mA. A 3-dimensional viewer program (One Volume Viewer, version 1.6.1.13; J. Morita) was used to define the tomographic cross-sections that corresponded to the long axis of the miniscrew and to simultaneously observe cross-sections of the adjacent roots. The distance between the root and the miniscrew was ascertained, and then we judged the root proximity to each miniscrew ( Fig 2 ). Root contact was defined as the absence of radiolucency between the screw and the adjacent root surface.
A miniscrew was considered a success when it endured an orthodontic force applied for 6 months or more without clinical mobility. To determine the difference between the self-tapping and self-drilling methods, we compared the success rates, placement torques, Periotest values, rates of root contact, and Periotest values according to root contact.
To evaluate measurement error, we randomly selected the CBCT images of 10 subjects and reevaluated their root proximity 2 weeks after the initial evaluations. The chi-square or Fisher exact test was used to compare the results of the self-tapping and self-drilling methods; the Fisher exact test was used when there were more than 20% of cells with an expected value of less than 5 in a contingency table. Analyses were performed using SPSS statistical software (version 16.0; SPSS Japan, Tokyo, Japan), and P <0.05 indicated statistical significance.
Results
Miniscrews that endured an orthodontic force for 6 months or more were considered successful. No screws loosened after 6 months or more because these subjects were patients who had been having orthodontic force applied for more than 2 years.
To evaluate the root proximity judgment error, the CBCT images of 10 subjects were randomly selected and reevaluated 2 weeks later. There was no difference between the first and the second judgments in these subjects.
The success rate of the miniscrews was approximately 96% for either placement technique. The respective success rates of male and female subjects were 95.9% and 95.2% in the self-drilling group, and 96.0% and 95.0% in the self-tapping group ( P >0.05). The success rates of the self-tapping and the self-drilling methods in the right side were 94.3% and 91.4%, respectively; the success rates in the left side were 97.1% and 100%, respectively ( Table I , P >0.05). The placement torque values of both methods were 7 to 7.5 N cm, with no significant difference ( Table II ). The Periotest value of the self-drilling method was 3.8, and this value was significantly greater than that of the self-tapping method ( Table III ). The rate of root contact on the right was 22.9% and that on the left was 17.1% ( P >0.05), with no significant difference between the 2 methods ( Table IV ). The Periotest value of the self-drilling miniscrew with root contact was significantly greater than that with no contact ( Table V ).
| Success rate (%) | n | |
|---|---|---|
| Self-tapping | 95.7 | 67 |
| Right | 94.3 | 33 |
| Left | 97.1 | 34 |
| Self-drilling | 95.7 | 67 |
| Right | 91.4 | 32 |
| Left | 100.0 | 35 |



