Introduction
In this prospective study, we compared differences in the diagnosis and treatment planning of impacted maxillary canines between 2 imaging modalities.
Methods
Twenty-five consecutive impacted maxillary canines were identified from the pool of patients seeking orthodontic treatment. The first set of radiographs consisted of traditional 2-dimensional (2D) images including panoramic, occlusal, and 2 periapical radiographs. The second set comprised prints of 3-dimensional (3D) volumetric dentition images obtained from a cone-beam computed tomography (CBCT) scan. Seven faculty member completed a questionnaire for every impacted canine and diagnostic radiographic modality (2D and 3D).
Results
The data show that the judges produced different decisions regarding localization depending on the x-ray method. There were 21% disagreement (or discordance) in the perceived mesiodistal cusp tip position and 16% difference in the perceived labiopalatal position. In the perception of root resorption of adjacent teeth, there was 36% lack of congruence. Twenty-seven percent of the teeth that were planned to be left, recovered, or extracted with the 2D radiographs had different treatment plans when the judges viewed the 3D CBCT images (McNemar test, chi-square, 4.45; P = 0.035). The clinicians’ confidence of the accuracy of diagnosis and treatment plan was statistically higher for CBCT images ( P <0.001).
Conclusions
These results showed that 2D and 3D images of impacted maxillary canines can produce different diagnoses and treatment plans.
Most permanent teeth erupt into occlusion unassisted. Occasionally, some permanent teeth become impacted and fail to erupt. This situation often requires intervention by both an orthodontist and an oral and maxillofacial surgeon. The decision for interceptive treatment takes into account several factors, including how to expose, recover, extract, or not treat. Some factors include location of the impaction, prognosis of intervention on the impacted tooth and adjacent teeth, surgical accessibility, impact of treatment on the final functional occlusion, and possible surgical morbidity. This treatment decision has traditionally been based on planar 2-dimensional (2D) radiographs. Medical technology offers 3-dimensional (3D) volumetric images, but these are expensive and expose patients to higher doses of radiation. New imaging techniques are now available in dentistry with cone-beam computed tomography (CBCT), which provides low radiation, rapid image scanning with radiographic and 3D volumetric data for each patient. This 3D technology will improve the dental provider’s ability to diagnose and treat patients with impacted teeth. In this study, we aimed to determine if using 2 imaging modalities, 2D and 3D systems, would result in a different diagnosis or a different treatment plan for impacted maxillary canines.
The maxillary canine is the second most commonly impacted tooth, after the third molars. The reported incidence ranges from 0.8% to 2.8%, depending on the population examined. It has been reported that the incidence of impaction is twice as likely in female patients. Even though maxillary canine tooth buds develop labially to adjacent tooth roots, the ratio of palatal impactions to labial impactions is at least 3:1. Other investigators have found impacted canines to be positioned palatally 85% of the time compared with labial positioning 15% of the time.
Proper localization of an impacted tooth is required to make an accurate diagnosis, determine proper surgical access, and plan the direction of orthodontic recovery forces. In the past, diagnostic radiographs included periapical, occlusal (normal and topographic), and panoramic radiographs. In orthodontics, knowing the exact location of an impacted canine is paramount, since the decision about whether it should be exposed, extracted, recovered, or left untreated influences the treatment plan.
For a labial impaction, the tooth can often be located by palpation. If the tooth is positioned in the middle of the alveolus or palatally, it is necessary to determine its labiopalatal location by taking 2 or more periapical radiographs at different horizontal angles. Clark’s rule enables the practitioner to determine the location of these impacted teeth. When radiographs are taken at different horizontal angulations of a pair of objects, the image of the palatal object moves in the same direction as the x-ray beam, whereas the labial object appears to move in the opposite direction. With this periapical film technique, the clinician can evaluate the labiopalatal position of the canine with sufficient accuracy in 92% of patients.
Additional radiographic images are often required to ascertain the exact location of an impacted tooth in all 3 dimensions. To aid in determining the vertical position and horizontal angulation, a panoramic radiograph is used. Normal occlusal or topographic occlusal radiographs help to determine the relative positions of adjacent teeth. In addition, they help to determine the labiopalatal position of the impacted canine in conjunction with the periapical films if the image of the impacted canine is not superimposed on other teeth. Frontal and lateral cephalograms often elucidate the proximity to other facial structures, such as the maxillary sinus and nasal floor.
Orthodontists and oral surgeons have always needed to precisely locate teeth and tissues in all 3 planes of space. To date, only planar radiographs have been available. 3D information has been available with medical x-ray computed tomography scanners, but limitations include exposure dose, cost, and access to CT imaging service providers. A new system, CBCT, has been developed and designed for 3D imaging of the craniofacial field. The unique feature of this system is that it uses a low-energy, fixed-anode tube, which produces a cone-shaped x-ray beam, a special image intensifier, and a solid-state sensor or an amorphous silicon plate for capturing the image. CBCT systems vary in their radiation, depending on the machine, the size of the radiated region, and the amounts of milliamps and kilovolts of the system, but the doses are lower than medical computed tomography systems.
CBCT images are inherently more accurate than traditional x-rays, since beam projection is orthogonal; this means that the x-ray beams are approximately parallel to one another, and the object is near the sensor. This explains why there is little projection effect and no magnification. In addition, the computer software addresses the projection effect, resulting in undistorted 1:1 measurements. This contrasts with traditional imaging, which always has some projection error because the anatomic regions of interest are at varying distances from the film. For example, panoramic radiographs have an unusual projection error because the main path of the x-ray beam comes from a slightly negative angulation. In this situation, the dental provider must account for these imaging artifacts when reading the images.
Another likely advantage of the CBCT scan is that the data acquired include information for the entire craniofacial region. Additional views such as lateral cephalograms, panoramic radiographs, occlusograms, airway evaluations, and volumetric images are available from the original acquisition data. These images can be manipulated with imaging software to aid the dental provider in diagnosis and treatment planning. The costs, efficiency, and benefits of CBCT imaging are favorable, because 1 imaging session can provide many views.
Material and methods
Eighteen consecutive patients (12 female, 6 male) with impacted maxillary canines were identified in the orthodontic clinic at the School of Dentistry, University of California at San Francisco. Twenty-five impacted canines were identified they included 7 bilateral impactions. Six canines were unilateral on the right, and 5 were unilateral on the left. The subjects ranged in age from 12.3 to 34.6 years (mean, 16.9 ± 5.8 years). Exclusion criteria included presence of deciduous teeth, craniofacial anomalies, incomplete root formation, and existing orthodontic appliances. For each subject, traditional 2D diagnostic radiographs and CBCT scans (Hitachi MercuRay, Hitachi Medical Technology, Tokyo, Japan) in digital imaging and communications in medicine (DICOM) format were obtained.
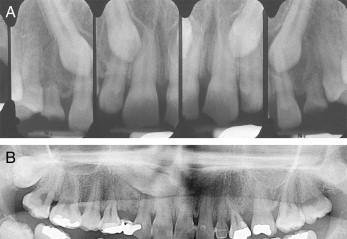
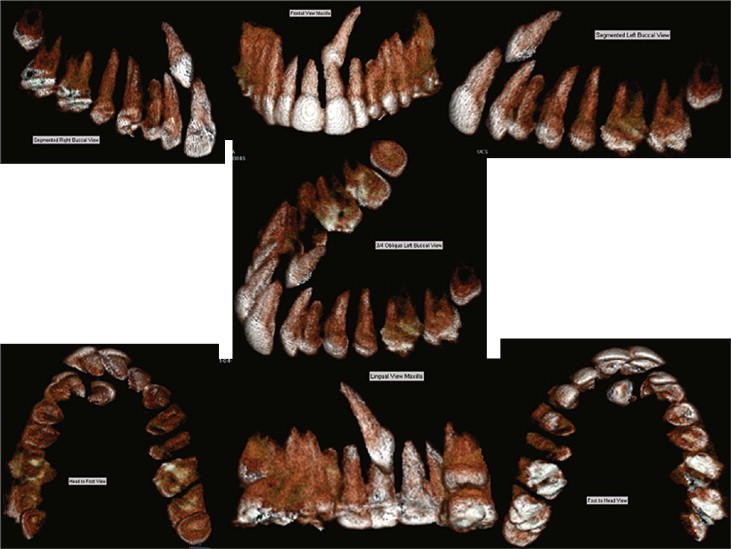
The 2D traditional radiographs included a panoramic radiograph to evaluate the vertical position, an occlusal x-ray to evaluate the proximity to adjacent teeth, and 2 periapical radiographs ( Fig 1 ) to determine the labiopalatal position. Volumetric images of the maxillary dentition were obtained from a CBCT scan. CBWorks software (CyberMed, Seoul, Korea) was used for the segmentation process. The volume operation and sculpt features eliminated all soft tissues and hard tissues except the maxillary dentition ( Fig 2 ). One operator (E.H.) performed segmentation of the maxillary dentition. Three-dimensional images included anterior, posterior, rostral-caudal, caudal-rostral, labial, and palatal views. The images were illustrated on 1 sheet of glossy photo paper (Epson, Long Beach, Calif). All identifying patient information was removed, including name, sex, age, and race. The institutional review board of the University of California at San Francisco, the Committee on Human Research, approved this study. Informed consent to participate in this study was obtained from each subject or, for minors, a guardian.
The presentation of the impacted maxillary canines was ordered with a random number generator ( www.randomizer.org ). In addition, 5 impacted maxillary canines were randomly selected for replicates and were interspersed randomly to be evaluated a second time to determine intraoperator reliability. A total of 60 stations were prepared; they included 30 sets of traditional 2D radiographs and 30 CBCT 3D volumetric renderings.
Seven faculty members participated in the study: 4 orthodontists (including J.H. and E.J.) and 3 oral surgeons (including J.S.L.); 4 had less than 10 years of clinical experience, and 3 had more. All impacted canines were evaluated in one session. Before starting, each judge reviewed the questionnaire as part of the calibration process. At each station, the judge was asked to complete the questionnaire for that tooth. Each clinician was randomly assigned a starting point. The time to complete all 60 questionnaires ranged from 1.5 to 2.5 hours.
After collection, the data were analyzed by using StatView (version 5, SAS Institute, Cary, NC) to evaluate differences between traditional radiographs and CBCT volumetric renderings. Statistical analyses were performed, accounting for the clustering in patients, by using SAS software (version 9.1.2). Repeated measures tests were used to examine the different results between using traditional 2D and CBCT 3D images. Mean confidence and 95% confidence intervals were estimated. Paired t tests compared confidence level differences. McNemar tests compared differences in dichotomous (ie, yes or no) questions between the 2D and 3D methods. Intraclass correlations with random case effects were estimated to determine continuous measure reliability of the replicates overall and separately for the 2D and 3D methods. Kappa statistics were used to measure reliability for categorical measures.
Intrarater reliability for all questions was acceptable, with a range from moderate to perfect for categorical measures, and moderate for continuous ones, depending on the question ( Tables I and II ). Orthodontic treatment plans (overall, and for recovery and extraction) had substantial agreement; recovery vectors had moderate agreement. It appears that raters have greater agreement with traditional 2D radiographs compared with CBCT images, but there was no significant difference between the 2 modalities.
| Variable | 2D and 3D | 2D | 3D |
|---|---|---|---|
| Mesiodistal location | 0.76 | 0.92 | 0.61 |
| Labiopalatal location | 0.82 | 0.87 | 0.77 |
| Vertical location | 0.63 | 0.73 | 0.53 |
| Root resorption | 0.65 | 0.73 | 0.55 |
| Orthodontic treatment plan | 0.72 | 0.77 | 0.64 |
| Orthodontic treatment plan (recover) | 0.75 | 0.75 | 0.75 |
| Orthodontic treatment plan (extract) | 0.81 | 0.85 | 0.72 |
| Number of recovery vectors | 0.54 | 0.53 | 0.54 |
| Initial recovery vector | 0.47 | 0.46 | 0.46 |
| Second recovery vector | 0.57 | 0.58 | 0.55 |
| Expect will erupt unassisted | 0.78 | 1.0 | 0.59 |
| Expect additional root resorption | 0.70 | 0.59 | 0.79 |
| Request for additional images | 0.62 | 0.46 | 0.80 |
| Variable | 2D and 3D | 2D | 3D |
|---|---|---|---|
| Confidence of diagnosis | 0.55 | 0.60 | 0.50 |
| Confidence of treatment plan | 0.41 | 0.41 | 0.43 |
Results
There were differences in the identified location of the impacted cusp tip depending on the radiographic modality. For the mesiodistal tip position, there was 79% agreement among the 7 judges’ responses on 25 teeth (175 total responses; Fig 3 ) between the 2 methods. In 21% of the responses, there was a difference between the 2 methods. The combined methods, traditional 2D radiograph and 3D CBCT volumetric views, had a range of agreement from 43% to 100% for each tooth based on the 7 judges’ responses (14 total responses for each tooth; Fig 4 ). There was 84% agreement for the labiopalatal position as assessed in 175 responses ( Fig 5 ). The combined methods had a range of agreement from 50% to 100% for each tooth. Fifty percent of the teeth had 100% agreement, and 76% had one or no clinician in disagreement. However, there were no statistically significant differences between the 2D and 3D methods (chi-square test, P >0.5). There was 50% agreement when localizing the cusp in the vertical dimension.




