Introduction
Hemifacial microsomia is a deformity of variable expressivity with unilateral hypoplasia of the mandible and the ear. In this study, we evaluated skeletal soft tissue changes after bimaxillary unilateral vertical distraction.
Methods
Eight patients (4 preadolescents 4 adolescents) each with a grade II mandibular deformity underwent a LeFort I osteotomy and an ipsilateral horizontal mandibular ramus osteotomy. A semiburied distraction device was placed over the ramus, and intermaxillary fixation was applied. Anteroposterior cephalometric and frontal photographic analyses were conducted before and after distraction. Statistics were used to analyze the preoperative and postoperative changes.
Results
Cephalometrically, the nasal floor and the occlusal and gonial plane angles decreased. The ratios of affected-unaffected ramus and gonial angle heights improved by 15% and 20%, respectively. The position of menton moved toward the midline. The photographic analysis showed a decrease of the nasal and commissure plane angles, and the chin moved to the unaffected side. The parallelism between the horizontal skeletal and soft tissue planes improved, with an increase in the affected side ramus height and correction of the chin point toward the midline.
Conclusions
Simultaneous maxillary and mandibular distraction improved facial balance and symmetry. Patients in the permanent dentition with fixed orthodontic appliances and well-aligned dental arches responded well to this intervention.
Highlights
- •
Eight growing patients with hemifacial microsomia were operated on the maxilla and affected side ramus.
- •
A semiburied distraction device was placed on the affected side mandibular ramus and intermaxillary fixation was applied.
- •
Outcomes were compared in younger and older patients.
- •
Older patients with fixed orthodontic appliances responded better.
Hemifacial microsomia (HFM) is the best known branchial arch syndrome and the second most common craniofacial birth defect after cleft lip and palate. It occurs in 1:3500 to 1:5600 live births. The term HFM refers to an asymmetric congenital condition of variable expressivity affecting primarily aural, oral, and mandibular development. HFM can be part of a broader and variable phenotypic spectrum known as oculoauriculovertebral dysplasia and always involves mandibular and ear malformations, but its severity varies. The mandibular deficiency usually is associated with microtia, macrostomia, and craniomaxillofacial asymmetry on the affected side.
The maxilla, temporal bone, and orbit are also affected as a result of the primary malformation and not secondarily affected by the mandibular hypoplasia, as suggested by some. In addition to the skeletal components, neural, muscular, and soft tissues are also affected. The mandibular deformity in HFM was classified by Pruzansky in 1969. In his classification, a grade I mandibular deformity consists of a normally shaped but small mandible. Grade II is a small and abnormally shaped mandibular ramus. In grade III, the mandibular deformity is characterized by absence of the mandibular ramus including the temporomandibular joint.
The treatment of HFM is centered on the mandibular deformity, but surgical timing is still controversial. The reason for this controversy relates to what clinicians believe is the facial growth potential in patients with HFM. Those who support early reconstruction, before skeletal maturity, assume that the mandibular skeletal asymmetry will worsen with time, and that early reconstruction will prevent secondary growth deformities. However, studies have found that the growth of the mandible on the affected side parallels that of the unaffected side, with the degree of asymmetry remaining relatively constant throughout craniofacial development.
Another concern is the psychological adjustment problems caused by differences in facial appearance. Some clinicians consider that the surgery should be done earlier to prevent social adjustment problems. Others, who prefer to wait for the completion of growth, believe that expectations of reconstructive surgery can cause disillusionment when performed too early, because the patient will still grow asymmetrically and additional surgery will be required.
The critical step in achieving better facial skeletal harmony is to restore maxillary and mandibular symmetry. Facial asymmetry is a main indication for orthognathic surgery. Traditionally, skeletal hypoplastic malformations are corrected with segment repositioning with autogenous bone grafts to increase the volume and size.
Recently, in patients with HFM, distraction osteogenesis has been used for correcting mandibular asymmetry. Mandibular elongation by gradual distraction is mainly indicated in HFM patients with mandibular deformities grades I and II. Since HFM primarily affects not only the mandible but also the maxilla and the orbit, clinicians have suggested simultaneous maxillary and mandibular interventions to correct these asymmetries with a single procedure. The purpose of this study was to assess skeletal and soft tissue changes after simultaneous maxillary and mandibular distractions in patients with HFM.
Material and methods
Eight patients with HFM grade II mandibular deformity and maxillary asymmetry with a mean age of 13 years 2 months underwent combined maxillary and mandibular distractions.
The surgical procedures were done under general anesthesia with nasotracheal intubation. A complete horizontal LeFort I osteotomy was performed. In contrast to the original method of Ortiz Monasterio et al, the pterygomaxillary junction was freed with a curved chisel on both sides, not only on the affected side. The unaffected maxillary side LeFort I osteotomy was loosely secured with 1 surgical wire placed above the maxillary first and second permanent molars. This wire acted as a hinge and pivot point where the maxillomandibular complex was expected to rotate toward the unaffected side ( Fig 1 ).
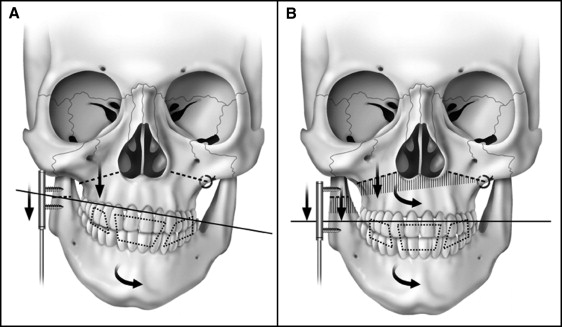
The ascending ramus was exposed along its anterior border behind the last molar and extended to the gonial angle and the surrounding area. The orientation of the osteotomy and the position of the distractor device determined the vector of distraction. A semiburied distraction device (Zürich II Distraction System; KLS Martin, Jacksonville, Fla) was positioned over the ramus in the planned direction (usually parallel to the long axis of the ramus) and fixed with self-tapping screws to secure the foot plates above and below the initially incomplete horizontal ramus osteotomy. The activating arm, from the semiburied device, was placed externally through a small incision below the mandibular angle. The osteotomy was completed and verified by opening the distractor. Before closure, the device was deactivated. The incision was closed, and rigid intermaxillary fixation with surgical wires was applied. Younger patients in the mixed dentition had custom-banded (maxillary and mandibular first permanent molars) arch bars with soldered hooks secured with circumdental wires for additional support during intermaxillary wire fixation and elastic therapy. In the adolescent patients, the orthodontic appliances were used for presurgical alignment and intermaxillary wire fixation and postoperative elastic therapy.
The extent of the required bone elongation and the vector of the distraction were determined by the severity of the ipsilateral mandibular deformity, the shape of the contralateral or unaffected mandibular ramus, and the transverse cant of the occlusal plane. After 7 days (latency period), the device was lengthened by 0.5 mm twice a day, for an average of 22 consecutive days. In younger patients, vertical elongation of over 15 mm was usually not required; therefore, a single 15-mm distractor was able to correct the occlusal plane discrepancy. In the adolescent patients who required more than 15 mm of vertical distraction, we preplanned 2 consecutive surgical procedures; after full activation of the first 15-mm distractor, it was removed, and another distractor of 30 mm was placed to complete the required vertical distraction. This is a required step, since the bone available to fixate the device above and below the planned osteotomy over the ramus is only sufficient to accommodate a distractor of limited length (usually 15 mm). After the initial distraction, a longer distractor can be placed. This device is partially opened before placement to clear the newly generated bone. Another reason why in certain patients it is necessary to use 2 consecutive devices relates to the fact that the initial placement is such that true vertical elongation is not obtained. The placement of the device has mainly a vertical component with a forward and medial vector because of the shape of the hypoplastic ramus and the contralateral ramus that needs to be emulated to correct as much as possible not only the size but also the form of the ramus. The placement of the distractor in this manner results in an effective loss of vertical length. Semiburied distractors are rigid and true to their length, but as explained above, the skeletal change is less than the true expression of the distractor; therefore, the activation to skeletal change ratio is not 1:1.
The goal of bimaxillary distraction is mainly to obtain a level occlusal plane and not perfect symmetry of the gonial angles. The reason is that the vertical discrepancy is usually greater at the gonial angles, and if they are leveled, the occlusal plane will be canted downward on the affected side. The gonial angle asymmetry can be addressed secondarily with bone grafting combined with other required procedures—eg, genioplasty or soft tissue augmentation—to further improve appearance.
Activation of the mandibular distractor resulted in vertical elongation of the affected ramus and medial displacement of both the maxillary and mandibular dentitions toward the unaffected side. This was possible because the patients had a complete affected side horizontal ramus osteotomy and a complete LeFort I osteotomy. In addition, they were placed in intermaxillary wire fixation to move the maxilla, the mandible, and the dentition as a unit. The patient’s preoperative occlusion was preserved through intermaxillary wire fixation during distraction. After distraction, a consolidation period with wire intermaxillary fixation was completed (4 weeks for the younger patients and up to 6 weeks for the adolescent patients). After this period, the wires were replaced with 6-oz, ¼-in orthodontic elastics for the next 3 months.
The patients were placed on a liquid diet during the intermaxillary fixation period and a soft diet for 4 to 6 weeks after the wires were removed. Orthodontic treatment was continued in the adolescent patients for 6 to 8 weeks after the wire fixation was removed. In the younger patients, the fixation appliances were removed after 2 to 3 months of elastic therapy. The distraction device was left in place for 6 months and removed in the operating room under general anesthesia.
All patients had anteroposterior (AP) cephalometric radiographs and clinical frontal photographs taken before and after distraction in a standard manner. Skeletal and soft tissue facial asymmetries were respectively measured with AP cephalometric and soft tissue photographic frontal analysis. Radiographs and photographs were hand traced by the same investigator (E.F.S.). Each measurement was repeated 3 times, and the mean was recorded for data comparison. There was no statistical difference between the 3 measurements as determined by the Dahlberg double determination method.
The measurements from the AP cephalograms are given in Table I . Two reference lines were traced ( Fig 2 ) and used to make vertical and horizontal measurements: a horizontal line (HL), the line connecting the right and left latero-orbitale points, and a vertical line (VL), the line perpendicular to the HL through the center of crista galli (most constricted point of the projection of the perpendicular lamina of the ethmoid).
| Measurement | Definition | Landmark |
|---|---|---|
| Vertical angle measurements | ||
| HL-Co′Co | Angle between the HL and the bicondylar plane | Condylion (Co), external lateral marginal portion of the condylar head |
| HL-NF′NF | Angle between the HL and the nasal floor plane | Nasal floor (NF), most inferior point on inside surface of the bony nasal cavity |
| HL-J′J | Angle between the HL and the maxillary jugal points | Jugal process (J), bilateral points on the jugal process of the maxilla at a crossing with the tuberosity of the maxilla |
| HL-OCP | Angle between the HL and the occlusal plane | Occlusal plane (OCP), horizontal plane passing through the molar and the incisors |
| HL-Go′Go | Angle between the HL and the gonial plane | Gonion (Go), most lateral and inferior point of the mandibular angle |
| Horizontal angle measurements | ||
| VL-isf | Angle between the VL and the superior midline | Incision superior frontale (isf), midpoint between the maxillary central incisor at the level of the incisal edges |
| VL-Me | Angle between the VL and the mental line | Menton (Me), point on the inferior border of the symphysis directly inferior to the mental protuberance |
| Tns-ANS | Angle between the VL and the nasal septum | Anterior nasal spine (ANS), tip of the ANS below the nasal cavity and above the hard palate Top of the nasal septum (Tns), the highest point on the superior aspect of the nasal septum |
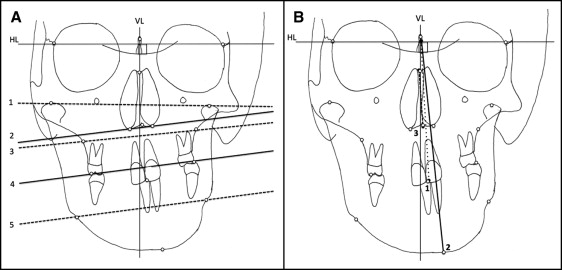
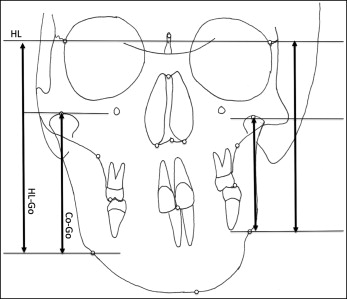
The gonial height ratio (HL-Go′/HL-Go) and the ramus height ratio (CoGo′/CoGo) were calculated from the AP cephalograms to compare the affected vs the unaffected sides. HL-Go′/HL-Go is the ratio between the linear perpendicular distance from the horizontal reference line to the affected Go′ point, and the linear perpendicular distance from the horizontal reference line to the unaffected Go point. Co′Go′/CoGo is the ratio between the linear perpendicular distance from the affected Co′point to the affected Go′point, and the linear perpendicular distance from the unaffected Co point to the unaffected Go point ( Fig 3 ).
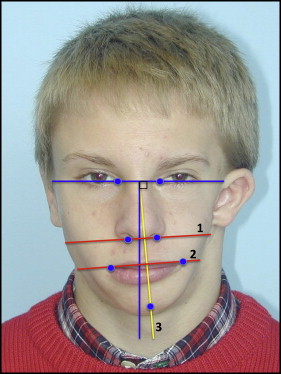
In the photographic facial analysis, we used 3 bilateral soft tissue landmarks identified on the frontal photographs: bilateral endocanthion (inner commissure of the eye fissure) and the center point of a line connecting the right and left endocanthions. Two reference lines were traced on the frontal photographs ( Fig 4 ): an HL, the line connecting the right endocanthion to the left endocanthion points; and a VL, the line perpendicular to the HL through the midline of the distance between the right and left endocanthion points. The measurements obtained from the frontal photographs are shown in Table II .
| Measurement | Definition | Landmark |
|---|---|---|
| Vertical angle measurements | ||
| HL-sbal′sbal (nasal base angle plane) | Angle between the HL and the nasal base plane | Subalare (sbal), lower limit of each alar base |
| HL-ch′ch (labial commissure angle plane) | Angle between the HL and the labial commissure plane, and 1 horizontal angle measurement | Cheilion (ch) point at each labial commissure |
| Horizontal angle measurement | ||
| VL-Pog (chin point) | Angle between the VL and the chin point | Pogonion (Pog), most anterior midpoint of the chin |
Statistical analysis
Paired t tests were used to examine the difference between the preoperative (T1) and postoperative (T2, 6 months after surgery) measurements using the Statistical Package for Social Sciences software (version15.0; SPSS, Chicago, Ill). The power of the paired t test was calculated for each variable considering a sample size of 8 and an α of 0.05, using the free software power and sample size calculator (version 3.1.2; Statistical Solutions, Boston, Mass).
Results
The results of the AP cephalometric analysis demonstrated vertical improvement in all patients as seen by statistically significant decreases relative to the HL of the nasal floor angle ( P = 0.004), the maxillary jugal plane angle ( P = 0.008), the occlusal plane angle ( P = 0.003), and the gonial plane angle ( P = 0.035). Of the horizontal changes, only the menton to the VL measurement ( P = 0.004) was statistically significant ( Table III ).
| Measurement | T1 mean ± SD | T2 mean ± SD | Difference T1 − T2 mean ± SD | P value | 95% CI of the difference | Power of paired t test (%) | |
|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||
| Bicondylar plane (HL-Co′-Co) (°) | 3.42 ± 2.07 | 2.14 ± 1.46 | 1.28 ± 1.70 | 0.093 | −0.29 | 2.86 | 41.2 |
| Nasal floor plane (HL-NF′NF) (°) | 14.28 ± 6.36 | 8.00 ± 6.55 | 6.28 ± 3.72 | 0.004 † | 2.83 | 9.73 | 97.7 |
| Maxillary jugal plane (HL-J′J) (°) | 11.85 ± 6.76 | 3.00 ± 4.12 | 8.85 ± 6.03 | 0.008 † | 2.28 | 3.27 | 94.2 |
| Occlusal plane (HL-OCP) (°) | 12.71 ± 5.85 | 4.42 ± 4.07 | 8.28 ± 4.46 | 0.003 † | 4.15 | 12.41 | 98.8 |
| Gonial plane (HL-Go′Go) (°) | 12.42 ± 7.18 | 4.00 ± 5.13 | 8.42 ± 8.24 | 0.035* | 0.80 | 16.05 | 69.3 |
| Superior midline (VL-isf) (°) | 5.71 ± 4.95 | 3.85 ± 5.08 | 1.85 ± 3.18 | 0.174 | −1.08 | 4.80 | 25.0 |
| Mental line (VL-Me) (°) | 7.00 ± 7.58 | 3.4 ± 7.05 | 3.6 ± 2.50 | 0.033* | 0.48 | 6.71 | 93.5 |
| Nasal septum deviation (Tns-ANS) (°) | 14.71 ± 6.36 | 11.14 ± 6.36 | 3.57 ± 4.03 | 0.058 | −0.16 | 7.30 | 55.5 |
| Gonial height (HL-Go′/HL-Go) (%) | 78.12 ± 14.45 | 93.06 ± 9.32 | −14.93 ± 13.59 | 0.027* | 2.36 | 27.50 | 76.0 |
| Ramus height (Co′-Go′/Co-Go) (%) | 65.85 ± 16.01 | 86.61 ± 12.35 | −20.76 ± 21.37 | 0.042* | 0.99 | 40.53 | 64.4 |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


