Table 18.1
First findings checked at the first visit of the patient (16 June 1994)
|
Findings
|
Tooth
|
|---|---|
|
Caries
|
16mo, 17o, 24mod, 25mo, 31cdl, 32c
|
|
Missing teeth
|
14, 18, 28 (Rö!), 38 verlagert, retiniert (Rö.), 48 verlagert, retiniert (Rö.)
|
|
Destructed teeth
|
12, 26 (Rö!)
|
|
Filled teeth
|
21p AF, 22p AF, 36mod AF, 37mo AF, 45ob CF, 47o CF
|
|
Crowns
|
13, 15 (metal ceramic)
|
|
Bridges
|
14 (pontic), 13, 15 (abutment teeth)
|
|
Nonvital teeth
|
21, 22, 26, 31, 36, 42, 47
|
|
Root fillings
|
21, 22, 36, 47 (Rö.)
|
|
Trepanation
|
42
|
|
Apical changes
|
21, 22, 42 (Rö: chronic apicalostitid)
|
|
Calculus
|
16–27, 35–46
|
Table 18.2
Explanation of abbreviations
|
Definition
|
Abbreviation
|
|---|---|
|
Caries
|
C
|
|
Missing teeth (not visible teeth)
|
X (extracted), X-ray! (shifted teeth?)
|
|
Destructed teeth
|
Z
|
|
Filled teeth (fillings)
|
AF (amalgam), CF (plastic)
|
|
Crowns, bridges
|
MK (metal ceramic), Br (bridge)
|
|
Negative vitality testing
|
Vit (−)
|
|
Root-treated teeth
|
WF
|
|
Trepanation
|
trep
|
|
Apical changes
|
G
|
|
Calculus
|
Zst
|
The quality assessment of information regarding the presence of dental documentation is different. Therefore, identifications may be complicated or even impossible (Andersen et al. 1995) (Table 18.3).
Table 18.3
Quality assessment of antemortem (AM) information
|
Category
|
Definition
|
|---|---|
|
Degree 0
|
No information
|
|
Degree 1
|
Information without patient file (no written documents)
|
|
Degree 2
|
Patient file only
|
|
Degree 3
|
Patient file, with single radiographs (unsystematic)
|
|
Degree 4
|
Patient file, with bitewings
|
|
Degree 5
|
Patient file with a full orofacial review and OPG radiographs (panoramic radiographs or similar)
|
The acceptance of information technology (IT) in dental practices is increasing. Paperless billing was introduced in 1997; now approximately 80 % of practitioners keep electronic records (Stratmann 1997). According to a statistical survey of the Dentist‘s Confederation (KZBV) in December 1998, in Germany, 91.31 % of 52,116 dentists, practice owners, or associates in private practice – with a total of 76,766 chamber members (according to the BZÄK statistics from the fourth quarter of 1998) – file their findings for conservative and surgical services in a computer system. This allows a more rapid recall of findings.
In the initial finding, all extractions, fillings (localization and extent), implants, dentures (crowns, bridges, etc.), bars, root residues, localization and extent of carious lesions, apical and conspicuous marginal bone defects, stains, calculus, and periodontal disease must be recorded. Such a complete initial finding with evaluation of all odontological features is the basis of any dental activity (Kaatsch and Ritz 1993).
18.2 -Finding
For billing of no. 01, the following index Fig. 18.2 (01-finding are made every half year and are paid by health insurance) is used in Germany. It includes a “comprehensive examination of the teeth, mouth and temporomandibular disorders” (Meurer 1988):
-
1 c = dental caries; 2 z = tooth = destructed; 3 f = tooth = missing (Fig. 18.2).
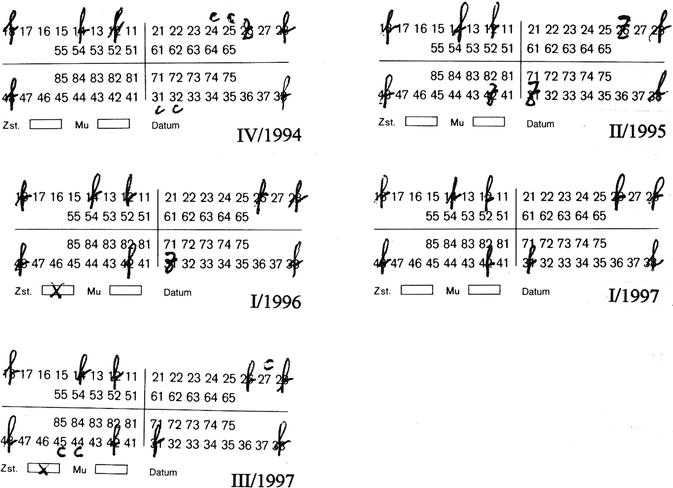 Fig. 18.201-findings are made every half year and are paid by health insurance
Fig. 18.201-findings are made every half year and are paid by health insurance
Most dentists in Germany use this index in the recall stage.
Fillings, implants, removable dentures, crowns, bridges, rails, root residues, the localization and extent of carious lesions, apical and conspicuous marginal bone defects, stains, calculus, and periodontal diseases are not gathered in the 01-finding.
Findings according to the DMF index, which are regarded as inadequate, are recorded as D = tooth = decayed (destructed), M = tooth = missing (missing), F = tooth = filled (filled); the so-called decay index, or the EKF-Index (German Version) records findings as E = tooth = extracted, K = tooth = decayed, F = tooth missing (the total number of teeth is 28 because the wisdom teeth are not taken into account); or in modification to the DMF-area index (DMF-S [surface]) by dividing the crown into five areas and finally to the DMF-tooth index (DMF-T [tooth]) with a maximum of 32 teeth per bite. The indices are used for caries epidemiology (statistical survey of the number of caries manifestations, up to the time of examination).
18.3 File Management
According to recent jurisdiction, the practitioner has to record all findings and measures. Dental records are not only reminders for the practitioners, but also for proper documentation for their patients. The complete recording of all stages of treatment (in a legal sense) has several functions:
1.
To ensure a scheduled further treatment by:
(a)
The same dentist
(b)
An assistant, representative, or successor
(c)
Another dentist/dental specialist by referral
2.
Protection against:
(a)
Complications and incidences
(b)
Liability claims because of malpractice
(c)
The accusation of negligence in examination and planning in case of failure or incident
(d)
The accusation of complicating the burden of proof
(e)
The accusation of providing insufficient documentation for assessments by insurance companies or legal authorities
(f)
The risk of rendering a faulty opinion and its legal consequences
3.
The practitioner is required to record each treatment step with detailed listing of treated teeth, diagnosis, and date of treatment (§ 5 BMV-Z). At the latest, the documentation must be completely available at the end of each treatment step (§ 5 para 2 BMV-Z) (Thieme 1982).
18.4 Documentation
18.4.1 IT – Documentation
Electronic data processing (EDP) was introduced in 1968 to rationalize billing in dental offices. Documentation was not the originally intended purpose. The technical problems were solved by an interface description, developed by the Central Research Institute of Ambulatory Health Care in Germany. The risks of IT for an orderly accounting and documentation for a possible legal dispute are obvious (German 1998). Back-up on a tamper-proof disk must be performed. Of course, a subsequent modification of documented treatments is possible without being apparent. However, a weekly or monthly documentation can be made on an only-once writeable disk. Properly performed IT documentation suggests the correctness of its content. The burden of proof is with the practitioner only if the completeness or accuracy of the stored data is doubtful (Walther 1996). Although the fundamental jurisdiction has yet been decided, it is acknowledged that dental documentation may be based on IT as well as on imaging and virtual recordings (Epple 1994).
A survey of 143 dentists in Middle Franconia, Germany (Hausmann et al. 1997) showed that, in 65 %, only a “minimal finding” was recorded; in 19.5 %, findings that also included restorations made by the respondent (“updated finding”) were recorded; and, in 15.5 %, findings in which all existing restorations, including preexisting restorations, were documented (“exemplar finding”). The study also inspected the error rate in the treatment of 61 patients, which was 21.36 % in “exemplar findings” and 55.6 % in “minimal findings.” The compared dental charts show considerable differences in the scope and quality of the recorded data. As a result, quite often, only a “minimum finding” is available for forensic examinations or assessments in legal disputes. According to this evaluation, IT is increasingly used in dental practice. Interestingly, 82 % of the practitioners with “exemplar findings” have used IT, compared with only 33 % of practitioners with “minimal findings”.
The increasing use of IT in dental offices will significantly improve the scope and quality of dental records. Another advantage inter alia is the rapid access to a large amount of data. The most important question is whether the computerized documentation includes all required data. Compared with handwritten charts, electronic charts are clearer:
-
Treatment date is at the left side, followed by tooth number and measures.
All billing-relevant data must be collected in detailed form. IT systems also offer options of entering additional data and comments, which is not important for billing but is important for medical documentation. All treatment-relevant data must be recorded (Stratmann 1997).
The second question is how corrections are to be handled. Errors must be able to be corrected, otherwise a correct billing is not possible. In a handwritten chart, alterations are always visible. Contrary to IT charts, where alterations are not retraceable, information regarding what was altered, by whom, and at what time, can be documented. The original data must be stored in a write-protected file. Modern image processing programs allow alterations of stored data. These corrections must be securely stored. Subsequent retouchings on an original X-ray image cannot be returned to the original condition (Stratmann 1997).
18.4.1.1 Storage Periods (Table 18.4)
Table 18.4
Storage periods for dental records in Germany (March 1995) (Thieme 1982)
|
1. Medical records (index cards): 3 years after treatment (BMV – Z § 5 (2) EC – Agreement § 4.2)
|
|
2. Orthodontics and periodontal disease: 3 years after treatment (BMV – Z § 5 (2) EC – Agreement § 4.2)
|
|
3. Dentures (planning models): 2 years after placement (§ 135 para 4, sentence 3 SGB V)
|
|
4. X-ray images: much longer storage periods (§ 28 para 3 RöV, valid in the version of 30 April 2003)
|
|
4.1. Recordings of X-ray treatments: 30 years after last treatment (§ 28, 3 RöV), e.g., radiation records
|
|
4.2. X-ray records: 10 years after last examination
|
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


