Introduction
The purpose of this study was to investigate differences in preoperative decompensation and postoperative compensation of the maxillary incisors in patients with skeletal Class III malocclusion treated with 2-jaw surgery and extraction or nonextraction of the maxillary first premolars.
Methods
The subjects consisted of 50 skeletal Class III patients who had a normal maxillary position, prognathic mandible, and mild crowding in the maxillary arch (≤4 mm). All patients were treated with 2-jaw surgery. They were divided into 2 groups: group 1 (n = 25) had extraction of the maxillary first premolars, and group 2 (n = 25) had no extractions. Lateral cephalograms were analyzed before treatment (T0), 1 month before surgery (T1), 1 day after surgery (T2), and after debonding (T3). After measurement of the skeletodental variables, statistical analyses were performed.
Results
At T0, group 1 exhibited more compensated maxillary incisors compared with group 2 (U1-SN, P <0.001). Considerable preoperative decompensation in group 1 and negligible preoperative decompensation in group 2 occurred at T1 (ΔU1-SN, −9.1° vs 1.1°). Although maxillary incisor inclination significantly decreased with surgical movement of the maxilla at T2, this increased to compensate for the postsurgical skeletal relapse in both groups at T3. Although 24% of group 1 had a normal range of maxillary incisor inclination (U1-SN) at T0, it increased to 68% at T1. A dominant pattern of the subjects within the normal range of U1-SN was maintained in groups 1 and 2 (80% and 96% at T2, and 72% and 80% at T3, respectively). According to the achievement ratio, the U1-SN value became close to the norm mainly by preoperative decompensation in group 1 (95.5%) and by surgery in group 2 (130.2%).
Conclusions
The results of this study might provide effective guidelines for predicting the amount and pattern of preoperative decompensation and postoperative compensation of the maxillary incisors in skeletal Class III patients treated with 2-jaw surgery.
Skeletal Class III patients exhibit diverse degrees of dentoalveolar compensation to maintain function and to mask the underlying skeletal discrepancies. Since the amount of surgical correction and the posttreatment stability can be influenced by dental decompensation, the main objective of preoperative orthodontic treatment is to eliminate the preexisting dental compensation.
For decompensation of the maxillary incisors in skeletal Class III patients, some need extraction of the maxillary premolars and others do not. A nonextraction approach and superior impaction of the posterior maxilla in 2-jaw surgery have been used to decompensate the inclination of the maxillary incisors by surgery and to reduce the total treatment duration. Therefore, it is important to know the amounts of change in maxillary incisor inclinations during preoperative orthodontic treatment, surgery, and postoperative orthodontic treatment for accurate surgical and orthodontic treatment planning according to whether or not the maxillary first premolars are extracted.
In terms of preoperative decompensation in skeletal Class III patients, several studies have reported that the incisors were not adequately decompensated, especially in the maxillary arch, and skeletal improvement was compromised by inadequate preoperative decompensation of the incisors. However, when sample selection and classification are inappropriate, the results can be misinterpreted by variations and biases from the skeletal, dental, and crowding characteristics in the subjects. Therefore, to investigate the effect of extraction of the maxillary premolars in 2-jaw surgery and orthodontic treatment, it is necessary to confine the samples as follows. First, the samples should comprise skeletal Class III patients with similar skeletal and dental characteristics except for maxillary incisor inclination before treatment. Second, the patients were treated with the same orthodontic treatment mechanics and surgical method. Third, the amount of crowding in the maxillary arch should be confined to examine the actual amounts and patterns of preoperative decompensation and postoperative compensation of the maxillary incisors. In addition, because maxillary incisor inclination can be changed by the surgical movement of the maxilla, the cephalograms taken immediately after surgery should be included to analyze the effect of the postsurgical skeletal relapse on the postoperative compensation of the maxillary incisors.
Few studies have reported the effect of extraction of the maxillary premolars on preoperative decompensation, surgical change, and postoperative compensation of maxillary incisors in skeletal Class III patients with the sampling criteria mentioned above. Therefore, the purpose of this study was to investigate the differences in preoperative decompensation, surgical change, and postoperative compensation of the maxillary incisors in skeletal Class III adults treated with 2-jaw surgery and orthodontic treatment in terms of extraction and nonextraction of the maxillary first premolars. The null hypothesis was that there was no difference in the amount and pattern of preoperative decompensation, surgical change, and postoperative compensation of the maxillary incisors between extraction and nonextraction of the maxillary first premolars.
Material and methods
The sample consisted of 50 skeletal Class III patients (31 men, 19 women; mean age, 22.4 ± 3.8 years) who had 2-jaw surgery (1-piece LeFort I osteotomy and bilateral sagittal split ramus osteotomy) and orthodontic treatment. This retrospective study was performed with the approval of the institutional review board of Seoul National University Dental Hospital in South Korea (CRI 12005).
The patients were divided into 2 groups according to extraction (group 1, n = 25; 12 men, 13 women; mean age, 22.0 ± 3.8 years) or nonextraction (group 2, n = 25; 7 men, 18 women; mean age, 22.9 ± 3.8 years) of the maxillary first premolars ( Table I ). The mandibular arch was treated without extractions in both groups.
| Variables | Group 1 (n = 25) 12 men, 13 women |
Group 2 (n = 25) 7 men, 18 women |
P value | ||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| Age (y) | 22.00 | 3.77 | 22.86 | 3.84 | 0.4282 |
| Duration (mo) | |||||
| Preoperative orthodontic treatment | 18.44 | 5.42 | 10.76 | 3.95 | 0.0000 ∗ |
| Postoperative orthodontic treatment | 8.68 | 2.44 | 8.48 | 2.74 | 0.7866 |
| Total treatment | 27.12 | 6.89 | 19.24 | 5.36 | 0.0000 ∗ |
| Amount of crowding (mm) | |||||
| Maxillary arch | −1.80 | 1.37 | −1.20 | 1.21 | 0.1117 |
| Mandibular arch | −2.50 | 2.22 | −2.22 | 2.89 | 0.7019 |
The inclusion criteria were bilateral Class III canine and molar relationships, ANB less than or equal to 0° (relatively normal anteroposterior position of the maxilla combined with a prognathic mandible), lack of severe facial asymmetry (≤3 mm of menton deviation from the facial midline), mild crowding in the maxillary arch (≤4 mm), and growth completion confirmed by cervical vertebral maturation status. Exclusion criteria were cleft lip or palate or other craniofacial syndrome, missing teeth (except for third molars), and tooth size discrepancy (eg, peg-shaped lateral incisors).
The amounts of crowding in both arches were not different between groups 1 and 2 (all, P >0.05; Table I ). Patients with moderate or severe crowding (≥4 mm) in the maxillary arch were excluded because extractions of the maxillary first premolars should be performed not for the relief of crowding, but for preoperative decompensation of the maxillary incisors. Despite similar amounts of crowding in the 2 groups, the extraction group included all patients with U1-SN and U1-NA (angular and linear) above normal values, and the extraction group included patients with normal values for those measurements. Therefore, the subjects in the subgroups were selected and not randomly assigned.
All patients were treated with a 0.022-in straight-wire appliance with the Roth prescription and sliding mechanics. We used 0.019 × 0.025-in stainless steel wires as the surgical and final archwires. During the preoperative orthodontic treatment, Class II elastics for decompensation or anchorage reinforcement—eg, transpalatal arch, headgear, and mini-implants—were not used. The major surgical movements were posterior impaction of the maxilla and setback of the mandible. Postoperative orthodontic treatment started after 4 weeks of surgical wafer use. The mechanics of postoperative orthodontic treatment did not differ between the 2 groups. Although the duration of postoperative treatment was not different between them ( P >0.05, Table I ), the durations of preoperative and total treatment were significantly different between the groups (all, P <0.001, Table I ).
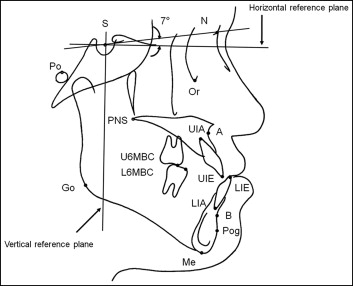
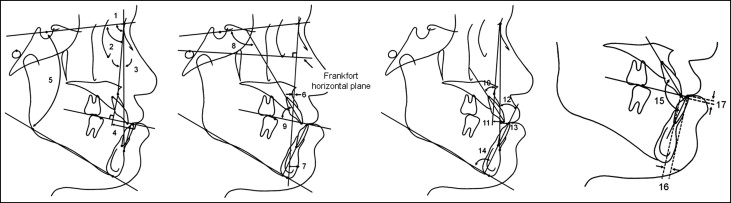
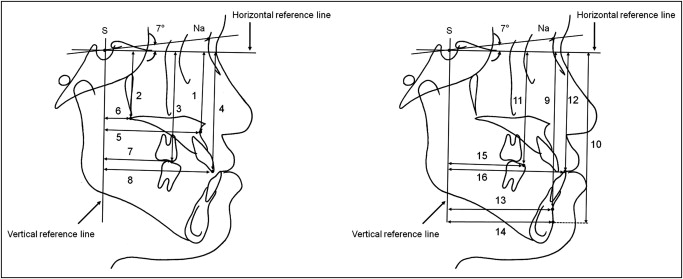
The lateral cephalograms were taken before treatment (T0), a month before surgery (T1), a day after surgery (T2), and at debonding (T3). Definitions of the landmarks, reference planes, and skeletodental variables are given in Figures 1 and 2 . The cephalograms were digitized by 1 operator (D.K.K.) using the V-Ceph program (version 5.5; CyberMed, Seoul, Korea). The horizontal and vertical distances from Point A, posterior nasal spine, Point B, pogonion, incisal edges of the maxillary and mandibular central incisors, and mesiobuccal cusp tips of the maxillary and mandibular first molars to the vertical and horizontal reference planes were measured to assess the amounts of surgical movement of the maxilla and the mandible ( Fig 3 ). The amount and pattern of change in U1-SN were calculated to evaluate treatment efficacy. The patient distributions according to the U1-SN referenced to the ethnic norms ±10° were investigated at each stage.
All variables from 20 randomly selected subjects were reassessed after 2 weeks by the same operator (D.K.K.). Differences calculated with Dahlberg’s formula ranged from 0.39 to 0.62 mm for linear measurements and from 0.47° to 0.74° for angular measurements. Since there were no significant differences between the first and second measurements, the first set of measurements was used.
Statistical analysis
The sample size was determined by a power analysis using a sample size determination program. The values of means and standard deviations of U1-SN from previous studies were used for the power analysis. Since the normality and equality of variance assumptions were not violated in the data set according to the Shapiro-Wilks test, Q-Q normality plots, and the Levene test, parametric analyses were used for the statistical methods. Independent t test, 1-way analysis of variance (ANOVA) with the Duncan multiple comparison test, chi-square test, binomial test, and repeated measures ANOVA were performed for statistical analysis.
Results
The variables between groups 1 and 2 were compared at each stage ( Tables II and III ).
| Variable | Norm ¶ | T0 stage | T1 stage | T2 stage | T3 stage | Comparison according to stages in each group | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Group 1 (n = 25) | Group 2 (n = 25) | P value § | Group 1 (n = 25) | Group 2 (n = 25) | P value § | Group 1 (n = 25) | Group 2 (n =2 5) | P value § | Group 1 (n = 25) | Group 2 (n = 25) | P value § | Group 1 (n =25) | Group 2 (n =25) | ||||||||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | P value ‖ | Multiple comparison | P value ‖ | Multiple comparison | ||||||
| SNA (°) | 81.31 | 82.40 | 3.39 | 82.41 | 2.98 | 0.9909 | 82.22 | 3.24 | 82.15 | 2.75 | 0.9295 | 83.15 | 3.69 | 83.26 | 3.24 | 0.9078 | 83.45 | 2.98 | 83.50 | 2.96 | 0.9547 | 0.5078 | 0.3160 | ||
| SNB (°) | 78.92 | 86.51 | 3.52 | 85.55 | 3.48 | 0.3386 | 86.55 | 3.78 | 85.25 | 3.44 | 0.2085 | 79.87 | 3.46 | 80.70 | 3.29 | 0.3849 | 81.42 | 3.15 | 81.84 | 3.29 | 0.6513 | 0.0000 ‡ | (c,d)<(a,b) | 0.0000 ‡ | (c,d)<(b,a) |
| ANB (°) | 2.62 | −4.11 | 2.24 | −3.14 | 2.06 | 0.1187 | −4.33 | 2.74 | −3.10 | 2.02 | 0.0781 | 3.29 | 1.78 | 2.56 | 1.65 | 0.1432 | 2.03 | 2.19 | 1.66 | 1.76 | 0.5146 | 0.0000 ‡ | (b,a)<(d,c) | 0.0000 ‡ | (a,b)<(d,c) |
| Wits appraisal (mm) | −1.72 | −13.27 | 3.77 | −12.45 | 4.01 | 0.4598 | −13.88 | 3.87 | −12.26 | 4.19 | 0.1618 | −5.03 | 3.17 | −5.59 | 3.68 | 0.5638 | −3.87 | 2.77 | −5.09 | 2.56 | 0.1121 | 0.0000 ‡ | (b,a)<(c,d) | 0.0000 ‡ | (a,b)<(c,d) |
| SN-GoMe (°) | 33.77 | 34.47 | 4.27 | 35.07 | 6.22 | 0.6913 | 34.19 | 4.55 | 35.16 | 6.32 | 0.5366 | 36.52 | 4.67 | 36.29 | 5.10 | 0.8713 | 37.70 | 4.74 | 38.54 | 5.76 | 0.5733 | 0.0212 ∗ | 0.1352 | ||
| A-N perpendicular (mm) | −0.79 | 0.94 | 3.46 | 0.33 | 2.87 | 0.5046 | 0.74 | 3.04 | 0.41 | 3.02 | 0.7018 | 1.71 | 3.86 | 1.53 | 3.21 | 0.8542 | 2.01 | 3.24 | 1.89 | 3.29 | 0.8914 | 0.4981 | 0.1939 | ||
| Pog-N perpendicular (mm) | −2.26 | 11.29 | 8.43 | 9.80 | 5.41 | 0.4604 | 11.29 | 8.44 | 9.00 | 5.79 | 0.2696 | −0.87 | 8.00 | −0.14 | 5.57 | 0.7105 | 1.53 | 8.06 | 1.93 | 6.02 | 0.8424 | 0.0000 ‡ | (c,d)<(a,b) | 0.0000 ‡ | (c,d)<(b,a) |
| U1-SN (°) | 106.55 | 119.51 | 5.25 | 112.09 | 3.67 | 0.0000 ‡ | 110.42 | 8.03 | 113.18 | 4.25 | 0.1350 | 106.31 | 7.35 | 107.96 | 5.47 | 0.3706 | 110.93 | 6.79 | 110.51 | 6.59 | 0.8259 | 0.0000 ‡ | c<(b,d)<a | 0.0033 † | (c,d)<(d,a,b) |
| U1-UOP (°) | 55.16 | 47.24 | 3.28 | 52.58 | 3.02 | 0.0000 ‡ | 53.63 | 5.62 | 52.10 | 2.99 | 0.2379 | 53.38 | 5.27 | 52.40 | 2.97 | 0.4218 | 51.41 | 5.34 | 51.23 | 4.25 | 0.8940 | 0.0000 ‡ | a<(d,c,b) | 0.4925 | |
| U1-NA angular (°) | 29.07 | 36.31 | 4.84 | 29.68 | 3.94 | 0.0000 ‡ | 28.60 | 8.25 | 31.04 | 4.77 | 0.2073 | 23.16 | 7.81 | 24.70 | 5.57 | 0.4251 | 27.35 | 7.18 | 27.01 | 6.65 | 0.8607 | 0.0000 ‡ | c<(d,b)<a | 0.0003 ‡ | (c,d)<(d,a)<(a,b) |
| U1-NA linear (mm) | 6.32 | 10.26 | 2.17 | 7.99 | 2.01 | 0.0004 ‡ | 6.06 | 2.65 | 8.11 | 2.24 | 0.0048 † | 4.86 | 2.32 | 6.14 | 2.28 | 0.0543 | 6.02 | 2.43 | 6.82 | 2.20 | 0.2291 | 0.0000 ‡ | (c,d,b)<a | 0.0041 † | (c,d)<(d,a)<(a,b) |
| L1-NB angular (°) | 25.27 | 20.83 | 5.60 | 20.57 | 8.34 | 0.8979 | 27.20 | 5.60 | 26.50 | 5.52 | 0.6575 | 22.13 | 4.67 | 22.63 | 5.63 | 0.7372 | 21.30 | 4.58 | 22.05 | 6.09 | 0.6238 | 0.0001 ‡ | (a,d,c)<b | 0.0001 ‡ | (a,d,c)<b |
| L1-NB linear (mm) | 6.01 | 6.28 | 2.20 | 6.26 | 3.33 | 0.9761 | 7.68 | 2.25 | 7.73 | 2.78 | 0.9463 | 6.13 | 2.21 | 6.56 | 2.74 | 0.5413 | 5.91 | 1.81 | 6.44 | 2.61 | 0.4092 | 0.0172 ∗ | (d,c,a)<b | 0.2658 | |
| IMPA (°) | 95.39 | 79.85 | 6.81 | 80.35 | 8.52 | 0.8199 | 86.46 | 6.50 | 86.09 | 8.00 | 0.8582 | 85.88 | 6.27 | 85.66 | 7.86 | 0.9119 | 82.18 | 6.47 | 81.67 | 7.98 | 0.8045 | 0.0011 † | (a,d)<(c,b) | 0.0289 ∗ | (a,d)<(d,c,b) |
| Interincisal angle (°) | 127.09 | 126.97 | 7.41 | 132.89 | 10.80 | 0.0283 ∗ | 128.72 | 7.88 | 125.56 | 8.86 | 0.1883 | 131.36 | 8.81 | 130.14 | 8.72 | 0.6257 | 129.32 | 7.78 | 129.28 | 9.28 | 0.9874 | 0.2842 | 0.0592 | ||
| Overjet (mm) | 3.55 | −2.52 | 3.05 | −3.33 | 2.61 | 0.3156 | −8.42 | 3.28 | −4.74 | 2.80 | 0.0001 ‡ | 3.48 | 1.94 | 3.81 | 0.56 | 0.4162 | 3.27 | 0.73 | 3.14 | 0.62 | 0.4987 | 0.0000 ‡ | b<a<(d,c) | 0.0000 ‡ | b<a<(d,c) |
| Overbite (mm) | 1.52 | −0.55 | 2.49 | −0.14 | 2.12 | 0.5312 | −0.35 | 2.00 | −1.04 | 1.76 | 0.2053 | 1.46 | 0.67 | 1.25 | 0.95 | 0.3770 | 1.78 | 0.82 | 1.61 | 0.94 | 0.5039 | 0.0000 ‡ | (a,b)<(c,d) | 0.0000 ‡ | b<a<(c,d) |
§ Independent t test was performed to compare the variables between the 2 groups at each stage
‖ One-way ANOVA was performed to compare the variables among stages in each group; the results were verified with the Duncan multiple comparison test. In multiple comparisons in each stage, a indicates T0; b , T1; c , T2; and d , T3
| Variable | T0-T1 | T1-T2 | T2-T3 | T0-T3 | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Group 1 (n = 25) | Group 2 (n = 25) | P value | Group 1 (n = 25) | Group 2 (n = 25) | P value | Group 1 (n = 25) | Group 2 (n = 25) | P value | Group 1 (n = 25) | Group 2 (n = 25) | P value | |||||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |||||
| ΔSNA (°) | −0.18 | 0.88 | −0.27 | 0.75 | 0.7128 | 0.93 | 2.23 | 1.12 | 1.71 | 0.7368 | 0.30 | 1.57 | 0.23 | 0.76 | 0.8495 | 1.05 | 1.86 | 1.09 | 1.36 | 0.9354 |
| ΔSNB (°) | 0.04 | 0.98 | −0.30 | 0.55 | 0.1311 | −6.69 | 1.87 | −4.55 | 1.93 | 0.0002 ‡ | 1.56 | 1.06 | 1.14 | 1.12 | 0.1770 | −5.08 | 1.71 | −3.71 | 1.86 | 0.0093 † |
| ΔANB (°) | −0.22 | 0.91 | 0.04 | 0.75 | 0.2754 | 7.61 | 2.16 | 5.66 | 1.88 | 0.0013 † | −1.26 | 1.16 | −0.90 | 1.11 | 0.2759 | 6.14 | 1.85 | 4.80 | 1.88 | 0.0146 ∗ |
| ΔWits appraisal (mm) | −0.61 | 1.56 | 0.19 | 1.67 | 0.0867 | 8.86 | 3.50 | 6.67 | 3.42 | 0.0301 ∗ | 1.16 | 2.63 | 0.50 | 2.45 | 0.3654 | 9.40 | 3.07 | 7.36 | 3.37 | 0.0298 ∗ |
| ΔSN-GoMe (°) | −0.28 | 1.27 | 0.09 | 0.84 | 0.2355 | 2.33 | 3.92 | 1.13 | 3.03 | 0.2342 | 1.18 | 2.41 | 2.25 | 3.14 | 0.1822 | 3.23 | 4.21 | 3.47 | 4.06 | 0.8355 |
| ΔA-N perpendicular (mm) | −0.19 | 1.02 | 0.08 | 1.49 | 0.4516 | 0.97 | 2.69 | 1.12 | 1.78 | 0.8235 | 0.30 | 2.08 | 0.36 | 1.23 | 0.9038 | 1.08 | 2.05 | 1.56 | 1.77 | 0.3826 |
| ΔPog-N perpendicular (mm) | 0.00 | 1.97 | −0.79 | 1.86 | 0.1483 | −12.16 | 4.74 | −9.15 | 3.91 | 0.0180 ∗ | 2.40 | 3.31 | 2.08 | 2.44 | 0.6946 | −9.76 | 3.90 | −7.86 | 4.19 | 0.1045 |
| ΔU1-SN (°) | −9.09 | 6.77 | 1.09 | 2.97 | 0.0000 ‡ | −4.11 | 4.33 | −5.22 | 3.48 | 0.3243 | 4.62 | 3.03 | 2.54 | 4.50 | 0.0620 | −8.59 | 6.29 | −1.58 | 5.42 | 0.0001 ‡ |
| ΔU1-UOP (°) | 6.39 | 5.79 | −0.48 | 2.62 | 0.0000 ‡ | −0.24 | 1.65 | 0.30 | 2.22 | 0.3322 | −1.98 | 3.15 | −1.18 | 3.91 | 0.4311 | 4.17 | 5.08 | −1.36 | 3.93 | 0.0001 ‡ |
| ΔU1-NA angular (°) | −7.71 | 8.50 | 1.36 | 3.23 | 0.0000 ‡ | −5.45 | 4.78 | −6.34 | 3.51 | 0.4553 | 4.20 | 3.58 | 2.31 | 4.37 | 0.1012 | −8.96 | 7.83 | −2.67 | 6.01 | 0.0025 † |
| ΔU1-NA linear (mm) | −4.20 | 2.63 | 0.12 | 1.43 | 0.0000 ‡ | −1.20 | 2.06 | −1.97 | 2.08 | 0.1968 | 1.16 | 1.88 | 0.67 | 1.63 | 0.3359 | −4.25 | 3.24 | −1.17 | 2.13 | 0.0002 ‡ |
| ΔL1-NB angular (°) | 6.37 | 5.43 | 5.93 | 6.79 | 0.8002 | −5.07 | 4.40 | −3.87 | 3.29 | 0.2820 | −0.83 | 3.19 | −0.58 | 2.53 | 0.7526 | 0.47 | 4.68 | 1.48 | 7.66 | 0.5758 |
| ΔL1-NB linear (mm) | 1.40 | 1.39 | 1.47 | 1.98 | 0.8817 | −1.56 | 1.48 | −1.17 | 1.13 | 0.3079 | −0.21 | 1.06 | −0.12 | 1.03 | 0.7476 | −0.37 | 1.44 | 0.18 | 2.30 | 0.3135 |
| ΔIMPA (°) | 6.62 | 5.53 | 5.75 | 6.75 | 0.6206 | −0.58 | 4.14 | −0.44 | 4.01 | 0.8992 | −3.70 | 3.19 | −3.99 | 3.33 | 0.7566 | 2.33 | 5.67 | 1.32 | 7.73 | 0.6007 |
| ΔInterincisal angle (°) | 1.76 | 9.77 | −7.33 | 7.94 | 0.0007 ‡ | 2.63 | 5.35 | 4.58 | 4.53 | 0.1716 | −2.04 | 3.56 | −0.86 | 4.05 | 0.2796 | 2.35 | 9.90 | −3.61 | 9.44 | 0.0341 ∗ |
| ΔOverjet (mm) | −5.91 | 3.13 | −1.41 | 2.43 | 0.0000 ‡ | 11.91 | 2.96 | 8.55 | 2.94 | 0.0002 ‡ | −0.21 | 2.08 | −0.67 | 0.73 | 0.3004 | 5.79 | 3.40 | 6.47 | 2.40 | 0.4154 |
| ΔOverbite (mm) | 0.20 | 2.24 | −0.90 | 1.61 | 0.0528 | 1.81 | 2.13 | 2.29 | 1.72 | 0.3888 | 0.32 | 0.99 | 0.36 | 1.14 | 0.8958 | 2.33 | 2.36 | 1.75 | 2.39 | 0.3929 |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


