Introduction
The aim of this study was to evaluate the dentoskeletal and soft-tissue effects of Class II malocclusion treatment with the Jasper jumper followed by Class II elastics at the different stages of therapy.
Methods
The sample comprised 24 patients of both sexes (11 boys, 13 girls) with an initial age of 12.58 years, treated for a mean period of 2.15 years. Four lateral cephalograms were obtained of each patient in these stages of orthodontic treatment: at pretreatment (T1), after leveling and alignment (T2), after the use of the Jasper jumper appliance and before the use of Class II intermaxillary elastics (T3), and at posttreatment (T4). Thus, 3 treatment phases could be evaluated: leveling and alignment (T1-T2), use of the Jasper jumper (T2-T3), and use of Class II elastics (T3-T4). Dependent analysis of variance (ANOVA) and Tukey tests were used to compare the durations of the 3 treatment phases and for intragroup comparisons of the 4 treatment stages.
Results
The alignment phase showed correction of the anteroposterior relationship, protrusion and labial inclination of the maxillary incisors, and reduction of overbite. The Jasper jumper phase demonstrated labial inclination, protrusion and intrusion of the mandibular incisors, mesialization and extrusion of the mandibular molars, reduction of overjet and overbite, molar relationship improvement, and reduction in facial convexity. The Class II elastics phase showed labial inclination of the maxillary incisors; retrusion, uprighting, and extrusion of the mandibular incisors; and overjet and overbite increases.
Conclusions
The greatest amount of the Class II malocclusion anteroposterior discrepancy was corrected with the Jasper jumper appliance. Part of the correction was lost during Class II intermaxillary elastics use after use of the Jasper jumper appliance.
The Jasper jumper is a tooth-borne functional appliance developed by James Jasper in 1987. It is flexible and can be attached reciprocally to the maxillary and mandibular arches to produce efficient sagittal interarch changes. Jasper jumper therapy has been prescribed for extraction and nonextraction Class II malocclusions with deepbites.
Regarding its distinct mode of action, the Jasper jumper appliance has many similar effects to the Herbst appliance, including restriction of maxillary anterior displacement, dentoalveolar retraction of the maxillary dentition, distal movement of the maxillary molars, dentoalveolar protraction of the mandibular dentition, mandibular protrusion, and improvement of the maxillomandibular relationship. On the other hand, some studies have found no significant change in mandibular growth.
The importance of active retention after correction of a Class II malocclusion with fixed orthopedic appliances has been widely emphasized in the literature. However, no previous studies reported the contribution of Class II elastics used as active retention after Jasper jumper therapy by evaluating and comparing the different phases of comprehensive orthodontic treatment. The evaluation of each treatment phase separately would determine the real contribution of the Jasper jumper appliance in Class II malocclusion correction.
Therefore, the aim of this study was to evaluate the different stages of therapy and the dentoskeletal and soft-tissue effects of Class II malocclusion treatment with the Jasper jumper followed by Class II elastics.
Material and methods
This study was approved by the Ethics in Research Committee of the University of São Paulo, Brazil, and all subjects signed informed consent. The sample size was calculated by using the ANB angle as the parameter and assuming detection of a minimum difference of 0.5° with a standard deviation of 0.5°. The minimum number of patients needed was 17. The sample of this prospective study comprised 24 Class II Division 1 patients of both sexes (11 boys, 13 girls) who consecutively came for treatment and fulfilled the inclusion criteria at the Department of Orthodontics, Bauru Dental School, University of São Paulo. Four lateral cephalograms were obtained of each patient in the following stages of orthodontic treatment: T1 (pretreatment), T2 (final leveling and alignment), T3 (after the use of the Jasper jumper appliance and before the use of Class II intermaxillary elastics), and T4 (posttreatment). In this way, 3 treatment phases could be evaluated: leveling and alignment (T1-T2), use of the Jasper jumper (T2-T3), and use of the Class II elastics (T3-T4). All patients were treated without extractions for a mean period of 2.15 years (SD, 0.30; range, 1.81-3.32 years).
The sample was selected according to the following inclusion criteria: at least a half-cusp bilateral Class II molar relationship; no agenesis, or supernumerary or lost teeth; convex profile; mandibular arch with slight or no crowding; and no previous orthodontic treatment. No cephalometric characteristic was considered as an inclusion criterion.
Treatment phase I, fixed appliances (leveling and alignment), started at T1 and lasted until T2, when passive rectangular stainless steel wires were placed in the maxillary and mandibular arches, before the Jasper jumper was placed.
The mean initial age of the patients was 12.58 years (SD, 1.19; range, 10.33-14.83 years), and this phase lasted a mean of 0.64 year (SD, 0.24; range, 0.32-1.25 years).
Treatment phase II comprised the use of the Jasper jumper appliance ( Fig 1 ) and started after leveling and alignment, right before placement of the Jasper jumper appliance (T2), and lasted until removal of the Jasper jumper (T3), after correction of the Class II anteroposterior discrepancy, with overcorrection of at least a quarter-cusp bilateral Class III molar relationship ( Fig 2 ).
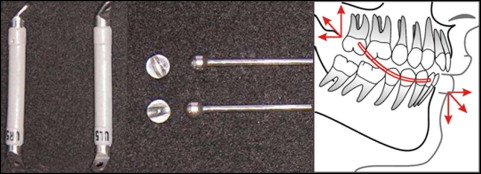

The mean age of the patients at the beginning of this phase was 13.22 years (SD, 1.15; range, 11.42-15.17 years), and this phase lasted a mean of 0.68 year (SD, 0.19; range, 0.41-1.00 year).
Treatment phase III was active retention and use of Class II intermaxillary elastics. The patients were told to use the elastics 18 hours a day. This phase began after removal of the Jasper jumper appliance (T3) and lasted until the end of orthodontic treatment (T4) ( Fig 2 ).
The mean age of the patients at the beginning of this phase was 13.90 years (SD, 1.26; range, 11.92-16.00 years). The mean duration of this phase was 0.83 year (SD, 0.33; range, 0.33-1.83 years); consequently, the mean age at the end of orthodontic treatment was 14.73 years (SD, 1.21; range, 12.67-16.92 years).
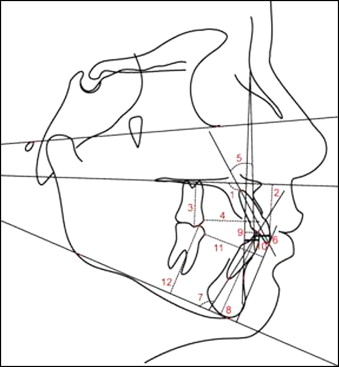
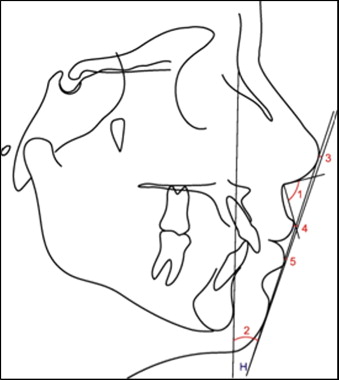
Anatomic tracings of the lateral cephalograms and landmark locations were manually conducted and digitized (AccuGrid XNT, model A30TL.F, Numonics, Montgomeryville, Pa) by 1 investigator (F.S.H.). These data were then stored in a computer and analyzed with Dentofacial Planner software (version 7.02, Dentofacial Software, Toronto, Ontario, Canada). This software corrected the magnification factors (6% and 9.8%) of the radiographic images and calculated the angular and linear cephalometric variables used in this study. The less usual cephalometric variables are illustrated in Table I and Figures 3 and 4 .
| 1.PP (°) Angle formed by the maxillary incisor long axis and the palatal plane (PP) |
| 1-PP (mm) Linear distance from the maxillary central incisor edge projected perpendicularly to the PP |
| 6-PP (mm) Linear distance from mesiovestibular cusp of the maxillary first molar projected perpendicularly to the PP |
| 6-ANSperp (mm) Linear distance from the maxillary first molar mesial point to the ANSperp line (line perpendicular to palatal plane passing through anterior nasal spine) |
| 1.NA (°) Angle formed by the maxillary incisor long axis and the NA line |
| 1-NA (mm) Linear distance between the most anterior point of the maxillary central incisor and the NA line |
| IMPA (°) Angle formed by the mandibular incisor long axis and the mandibular plane (GoMe) |
| 1-GoMe (mm) Linear distance between the mandibular incisor edge perpendicular to GoMe |
| A-Nperp (mm) Linear distance from Point A to the Nperp line (line perpendicular to the Frankfort plane passing through point N) |
| Pog-Nperp (mm) Linear distance from Pog to the Nperp line |
| 1.NB (°) Angle formed by the mandibular incisor long axis and the NB line |
| 1-NB (mm) Linear distance between the most anterior point of the mandibular central incisor and the NB line |
| 6-Pogperp (mm) Linear distance between the mandibular first molar mesial point to the Pog-perp line (line perpendicular to the mandibular plane Go-Me passing through Pog) |
| 6-GoMe (mm) Linear distance between the mesiovestibular cusp of the mandibular first molar perpendicular to GoMe |
| NLA (°) Angle formed by the Prn′-Sn line and UL-Sn′ line (Prn′, pronasal point; Sn subnasal point; UL, upper lip) |
| H.NB (°) Angle formed by the H-line (line that passes through soft-tissue Pog and the upper lip) and the NB line |
| H-nose (mm) Linear distance from the tip of the nose to the H-line |
| UL-E (mm) Linear distance between the upper lip anterior point and the E-line (esthetic plane of Ricketts; line that passes through the tip of the nose and soft-tissue Pog) |
| LL-E (mm) Linear distance between the lower lip anterior point and the E-line |
Thirty lateral cephalograms were randomly selected, retraced, redigitized, and remeasured by the same examiner (F.S.H.) after a 30-day interval. Casual and systematic errors were calculated by comparing the first and second measurements with Dahlberg’s formula and dependent t tests, respectively, at a significance level of 5%.
Statistical analysis
Dependent analysis of variance (ANOVA) and Tukey tests were used to compare the durations of the 3 treatment phases and for intragroup comparisons of the 4 treatment stages. All statistical analyses were performed with Statistica software (Statistica for Windows, version 6.0, Statsoft, Tulsa, Okla).
Results
Only 3 of the 33 evaluated variables (NAP, 6-ANSperp, and 1.NB) showed statistically significant systematic errors, and no variable showed casual errors greater than 1.5° or 1.0 mm.
Phase III, comprising the use of Class II elastics, was significantly longer than the other 2 treatment phases ( Table II ).
| Variable | Phase I | Phase II | Phase III | P |
|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | ||
| Duration (y) | 0.64 (0.24) A | 0.68 (0.19) A | 0.83 (0.33) B | 0.027 ∗ |
There was restriction of anterior growth of the maxilla between stages T1 and T4. There were significant increases in mandibular length only between T1 and T2 ( Table III ).
| Variable | T1 | T2 | T3 | T4 | P |
|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | ||
| Maxillary skeletal component | |||||
| SNA (°) | 83.31 (3.49) A | 82.66 (4.59) AB | 82.20 (4.24) AB | 81.99 (4.24) B | 0.001 ∗ |
| A-Nperp (mm) | 1.66 (3.74) A | 1.14 (4.21) AB | 0.45 (3.88) B | 0.79 (4.68) AB | 0.016 ∗ |
| Co-A (mm) | 85.71 (4.70) A | 85.14 (4.99) A | 84.98 (4.86) A | 85.61 (4.73) A | 0.152 |
| Mandibular skeletal component | |||||
| SNB (°) | 78.11 (2.52) A | 78.52 (2.68) A | 78.34 (2.91) A | 78.47 (2.62) A | 0.445 |
| Pog-Nperp (mm) | −3.91 (6.37) A | −2.90 (7.10) A | −3.97 (6.73) A | −2.64 (6.35) A | 0.907 |
| Co-Gn (mm) | 106.52 (5.73) A | 108.61 (5.26) B | 109.43 (5.56) BC | 110.49 (5.36) C | 0.000 ∗ |
| Maxillomandibular relationship | |||||
| ANB (°) | 5.22 (3.14) A | 4.15 (3.69) B | 3.84 (2.88) B | 3.50 (3.38) B | 0.000 ∗ |
| Wits (mm) | 2.55 (3.02) A | 2.46 (3.16) A | −0.53 (3.21) B | 0.34 (2.87) B | 0.000 ∗ |
| NAP (°) | 8.43 (7.50) A | 5.85 (8.76) B | 5.33 (7.04) B | 4.77 (8.39) B | 0.000 ∗ |
| Vertical component | |||||
| SN.GoGn (°) | 30.26 (4.19) A | 30.08 (4.87) A | 30.81 (4.50) A | 30.57 (4.70) A | 0.204 |
| FMA (°) | 24.39 (5.01) A | 24.30 (5.55) A | 25.15 (5.44) A | 24.40 (5.19) A | 0.108 |
| LAFH (mm) | 61.59 (4.73) A | 63.83 (4.81) B | 64.95 (4.97) C | 64.93 (4.85) C | 0.000 ∗ |
| S-Go (mm) | 69.65 (4.71) A | 72.24 (5.25) B | 73.05 (5.40) B | 73.32 (5.96) B | 0.000 ∗ |
| Maxillary dentoalveolar component | |||||
| 1.PP (°) | 114.34 (6.76) AD | 117.95 (5.74) B | 108.57 (5.21) C | 112.52 (5.22) D | 0.000 ∗ |
| 1-PP (mm) | 26.39 (2.32) A | 26.15 (2.50) A | 27.84 (2.49) B | 27.49 (2.72) B | 0.000 ∗ |
| 1.NA (°) | 24.93 (7.31) AD | 29.19 (7.81) B | 19.97 (7.92) C | 23.74 (8.11) D | 0.000 ∗ |
| 1-NA (mm) | 4.79 (2.99) A | 6.43 (3.50) B | 3.70 (3.33) A | 4.68 (3.95) A | 0.000 ∗ |
| 6-PP (mm) | 20.80 (1.90) A | 21.80 (1.95) A | 20.93 (1.87) A | 21.02 (3.62) A | 0.347 |
| 6-ANSperp (mm) | 31.08 (3.44) A | 29.98 (3.07) A | 31.39 (3.46) A | 31.91 (13.65) A | 0.655 |
| Mandibular dentoalveolar component | |||||
| IMPA (°) | 97.54 (5.65) A | 99.50 (7.78) AC | 104.57 (5.51) B | 101.42 (6.70) C | 0.000 ∗ |
| 1-GoMe (mm) | 38.54 (3.30) A | 39.02 (3.22) A | 37.72 (3.16) B | 38.58 (3.27) A | 0.001 ∗ |
| 1.NB (°) | 28.48 (4.89) A | 30.88 (6.86) AC | 36.38 (4.90) B | 33.11 (5.12) C | 0.000 ∗ |
| 1-NB (mm) | 5.09 (2.04) A | 5.59 (2.21) A | 7.81 (2.22) B | 6.87 (2.31) C | 0.000 ∗ |
| 6-Pogperp (mm) | 29.54 (2.71) A | 29.80 (2.65) A | 28.22 (2.35) B | 28.99 (2.70) AB | 0.000 ∗ |
| 6-GoMe (mm) | 27.30 (2.75) A | 28.62 (2.58) B | 30.34 (2.59) C | 30.29 (2.75) C | 0.000 ∗ |
| Dental relationships | |||||
| Overjet (mm) | 6.20 (2.18) A | 6.13 (1.57) A | 1.06 (1.46) B | 2.51 (0.53) C | 0.000 ∗ |
| Overbite (mm) | 4.95 (1.57) A | 2.49 (1.92) B | 0.67 (1.02) C | 1.84 (0.80) B | 0.000 ∗ |
| Molar relationship (mm) | −1.32 (1.56) A | −1.45 (1.56) A | 3.07 (1.04) B | 2.59 (1.10) B | 0.000 ∗ |
| Soft-tissue component | |||||
| NLA (°) | 104.31 (10.41) A | 107.96 (13.11) AB | 111.49 (14.62) B | 108.79 (11.79) AB | 0.005 ∗ |
| H.NB (°) | 14.54 (5.08) A | 13.75 (3.18) A | 11.41 (4.36) B | 11.12 (4.27) B | 0.000 ∗ |
| H-nose (mm) | 0.95 (5.32) A | 1.33 (4.71) A | 4.84 (4.85) B | 5.12 (5.26) B | 0.000 ∗ |
| UL-E (mm) | −1.79 (2.82) A | −2.54 (2.39) A | −3.94 (2.71) B | −4.14 (2.87) B | 0.000 ∗ |
| LL-E (mm) | −0.86 (2.19) A | 0.00 (2.12) B | 0.32 (2.49) B | −1.05 (2.38) A | 0.000 ∗ |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


