Case• 9. A large carious lesion
SUMMARY
How will you deal with a large carious lesion in a maxillary molar tooth?
History
Complaint
A 30-year-old patient complains of severe attacks of pain, each of a few seconds duration and fading slowly, but she cannot identify which tooth is responsible. Hot, cold or sweet foods or cold air on the upper right jaw make the pain worse.
History of complaint
The pain has been present intermittently for several months but has only recently become severe. There is no pain on biting.
Dental history
The patient attends on a casual basis for dental treatment. Despite the fact that this carious lesion is very large, it is the only lesion in an otherwise intact arch and there have been no other lesions noted in the last 3 years. The patient is therefore classified as a low risk for dental caries.
Medical history
The patient is fit and well.
Examination
Extraoral examination
The extraoral examination reveals no significant abnormality.
Intraoral examination
There is no tenderness or swelling over the buccal or palatal roots.
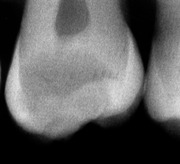
▪ The maxillary right second molar is shown inFigure 9.1. What do you see and how do you assess the problem so far?
The history is classical of acute pulpitis and repeated attacks of pain – as opposed to continuous severe pain – probably indicate that the pulp can be preserved if the caries is treated. The fact that there is no pain on biting and no tenderness over the roots also suggests a reversible pulpitis and excludes periapical periodontitis.
There is a deep, cavitated lesion on the occlusal surface with extensive exposed carious dentine. Opaque white demineralization of the marginal, unsupported enamel indicates that it is also carious, despite not having fractured off. The dark colour of the tooth distally suggests that caries undermines enamel to the distal marginal ridge and it certainly involves the dentine supporting the enamel of the mesial approximal surface.
This is a relatively small upper second molar. Females have slightly smaller teeth, and when second molars are this small, the third molar may not have developed. This may influence the decision to restore or extract the tooth.
Investigations
▪ What investigations would you carry out?
A test of tooth vitality (sensitivity) is required even though the symptoms suggest a vital pulp. This is a large cavity in a molar and partial pulp vitality is a possibility.
A radiograph is required for a variety of reasons. The proximity of the lesion to the pulp and its lateral extent, undermining cusps and the approximal enamel, will affect restorability. Pulp size reduction by reactionary dentine will also be visible. It may also be possible to see evidence of periapical periodontitis, widening of the periodontal ligament and loss of the lamina dura. The ideal views would be a bitewing or periapical depending on your suspicions about pulp vitality or caries in other teeth.
When you perform these investigations, the tooth responds quickly and strongly to ethyl chloride (cold), indicating a hypersensitive pulp, though the proximity of the pulp to the cavity may also contribute to this strong response.
▪ The radiograph is shown inFigure 9.2. What do you see?
 |
| Fig. 9.2 |
The coronal radiolucency indicating caries is extensive. It reaches the inner third of the dentine close to the pulp. There appears to be a bridge of intact dentine between the lesion and the pulp chamber. Caries has undermined most of the occlusal enamel and also the distal enamel, but there are no separate approximal lesions or cavitation present. The coronal pulp chamber is rounded and much reduced in size, with the pulp horns obliterated by reactionary (‘tertiary’) dentine.
There is slight radicular ‘burn-out’ of the dentine immediately above and below the mesial and distal amelodentinal junction. This could be mistaken for caries extending from the crown into the distal root, but the shape and site of the relative radiolucency do not suggest caries.
Diagnosis
▪ What is your diagnosis?
Acute pulpitis in the maxillary second molar caused by extensive occlusal caries. The pulp appears vital and there is no evidence of periapical periodontitis. The pulp does not appear exposed radiographically.
Treatment
▪ Is this tooth restorable?
Yes. The prognosis must be guarded as the pulp may still lose vitality, as a result of either the caries or restoration. There is no indication for immediate endodontic treatment.
▪ What will you do first?
The patient is in pain and the immediate response must be to relieve it. Pulpitis does not respond to analgesic drugs and the appropriate treatment is restoration.
If a permanent restoration cannot be placed immediately, a temporary dressing could be placed following partial excavation of caries. This would relieve pain by removing the stimulus (bacterial products and acid penetrating the dentine) and by insulating the inflamed pulp from the triggering stimuli. Eugenol-containing temporary filling materials have an obtundent effect on the pulp, reducing pain. However, it must be noted that eugenol-containing materials must not be used if the final restoration to be placed is an adhesive composite as the eugenol adversely affects the bond/polymerization process. A second alternative might be to place a longer-term provisional restoration with a calcium hydroxide lining, in an attempt to induce further reactionary dentine formation in the pulp. However, the carious lesion does not appear to be in imminent danger of breaching the pulp.
Removal of caries will leave a weakened crown, more susceptible to fracture under normal occlusal loading. An immediate definitive restoration is the best course of action.
Subsequently, the patient needs a full caries risk assessment and an intensive preventive regime that may include topical fluorides if other lesions are found. Further details are given in problem 1.
▪ Why not extract this tooth?
Such a large lesion in a casual dental patient might well lead to extraction if that were the patient’s wish. However, this is a young patient and she may not have a third molar or, if it is present, it may not erupt spontaneously after extraction of the second molar. Even though the prognosis may be guarded there is a good chance that this tooth could be retained for many years. This would be the better immediate option because the condition of the rest of the dentition has not yet been fully assessed.
Operative treatment
▪ How will you provide analgesia?
A buccal infiltration of local anaesthetic including a vasoconstrictor should be sufficient. There is no continuous pulpal pain to suggest that obtaining analgesia will be a problem. If this fails, palatal infiltration would be an appropriate next step, or intraligamentary injection.
▪ Is rubber dam essential for this restoration?
Yes, it is required. There is a risk of pulp exposure. Though this is small, contamination of the cavity by oral bacteria could reduce the chances of success of subsequent endodontic treatment.
The lesion is extensive and it may be that some carious tissue will have to be retained. The marginal seal of the restoration will be critical to its final success. An adhesive restoration will require a controllable, dry field to achieve the best seal. Rubber dam will also help by controlling the soft tissues, improving visibility and access. The final quality of restorations placed under rubber dam is considered to be higher than those placed without.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses



