Case• 7. A dry mouth
SUMMARY
A 50-year-old lady presents to you in your hospital dental department complaining of dry mouth. Identify the cause and plan treatment.
History
Complaint
She complains of dryness which makes many aspects of her life a misery. The dryness is both uncomfortable and renders eating and speech difficult. She is forced to keep a bottle of water by her side at all times.
History of complaint
She first noticed the dry mouth about 4 or 5 years ago though it may have been present for longer. At first it was only an intermittent problem but over the last 3 years or so the dryness has become constant. Recently the mouth has become sore as well as dry.
Medical history
The patient describes herself as generally fit and well but has had to attend her medical practitioner for poor circulation in her fingers. They blanch rapidly in the cold and are painful on rewarming. She has also used artificial tears for dry eyes for the last 2 years but takes no other medication.
Examination
Extraoral examination
She is a well-looking lady without detectable cervical lymphadenopathy. There is no facial asymmetry or enlargement of the parotid glands and the submandibular glands appear normal on bimanual palpation. Her eyes and fingers appear normal.
Intraoral examination
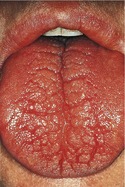
▪ The appearance of the patient’s mouth is shown inFigures 7.1and7.2. What do you see? How do you interpret the findings?
 |
| Fig. 7.2 |
The alveolar mucosa appears ‘glazed’ and translucent or thin (atrophic) suggesting long-standing xerostomia. Some oral debris adheres between the teeth, again suggesting dryness, which causes plaque to be thicker and more tenacious. There are carious lesions and restorations at the cervical margins of the lower anterior teeth, indicating a high caries rate. The tongue is lobulated and fissured. Both features suggest a lack of saliva.
If you were able to examine the patient you would find that her mouth does feel dry. Gloved fingers and mirror adhere to the mucosa making examination uncomfortable. Parts of the mucosa, especially the palate and dorsal tongue appear redder than normal. No saliva is pooling in the floor of the mouth and what saliva can be identified is frothy and thick. Small amounts of clear but viscid saliva can be expressed from all four main salivary ducts.
▪ What are the common and important causes of xerostomia and how are they subdivided?
In true xerostomia the salivary flow is reduced. The term ‘false xerostomia’ describes the sensation of dryness despite normal salivary output.
| Type of xerostomia | Common causes |
|---|---|
| False |
Mouth breathing
Mucosal disease
Psychological
|
| True |
Drugs
Dehydration
Sjögren’s syndrome
Irradiation
Neurological
Developmental anomaly
|
▪ On the basis of the history and examination which cause is the most likely? Why?
Sjögren’s syndrome is the most likely cause. It is the commonest single medical disorder causing xerostomia. It also causes dry eyes and predominantly affects female patients of middle age. Sjögren’s syndrome is sometimes defined by the presence of dry eyes and mouth, with or without an autoimmune/connective tissue disorder. This patient meets these criteria though they are rather imprecise and further investigations would be required to confirm the diagnosis.
▪ Which causes have you excluded and why?
Drugs are by far the commonest cause of true xerostomia but this patient is not taking any medication.
Dehydration is a common cause in elderly people who may have a habitual low fluid intake, especially when institutionalized. It also accompanies cardiac or renal failure or diuretic drugs. (The combination of drugs and disease probably explains the apparent association of xerostomia with age). These are not factors in this case.
False xerostomia is very common. Those who sleep with an open mouth will have xerostomia on waking, compounded by the normal reduction in salivary secretion at night. Diseases causing oral mucosal roughness such as lichen planus or candidosis may cause a sensation of dryness but no such condition is present. False xerostomia may be a feature, sometimes a central one, in psychiatric disorders. However, this patient’s mouth is genuinely dry. The history of prolonged and unremitting dryness over a period of years almost always indicates a salivary disorder and the appearance of the mucosa and the high caries rate indicate true xerostomia.
Neurological and developmental causes, such as aplasia of gland or atresia of ducts, are very rare and need not be considered further until common causes have been investigated. There is no history of irradiation of the head and neck.
▪ What is Sjögren’s syndrome and how may the condition be subclassified?
Sjögren’s syndrome is a poorly understood autoimmune disorder in which exocrine glands are destroyed. In primary Sjögren’s syndrome the salivary and lacrimal glands are those most affected (though there are often nonspecific systemic signs of autoimmune disease such as Raynaud’s phenomenon) and there is sometimes salivary gland swelling. Other exocrine glands and organs are also affected. In secondary Sjögren’s syndrome there is an accompanying connective tissue disorder such as rheumatoid arthritis, systemic lupus erythematosus or mixed connective tissue disea/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses



