Case• 66. A pain in the head
SUMMARY
A 58-year-old female patient attending for routine dental care mentions that she has a severe headache and wishes to delay treatment. What should you do?
History
Complaint
The headaches affect her whole head, are short but severe, with dizziness, nausea and blurred vision (Figure 66.1).
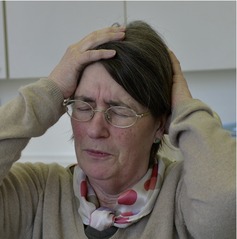 |
| Fig. 66.1 |
History of complaint
The headaches started only 2 weeks ago. She has not been able to identify any causes. The only way she has been able to manage the pain is to lie still in bed until the pain is over. Over-the-counter painkillers have no effect. The present headache started on the way to your surgery.
Medical history
The patient is overweight, has smoked 15 cigarettes a day for 20 years and drinks 22 units of alcohol a week.
Dental history
The patient attends regularly and has no dental problems. You have noted attrition from bruxism but she has never complained of tenderness in the muscles of mastication.
▪ How do you assess the history so far?
Severe headaches with nausea and visual disturbance on an occasional basis would suggest migraine as a cause.
However, migraine usually has onset in young adult or middle age and would be unusual as a new diagnosis in a postmenopausal patient. The headache is not described as unilateral, as most migraines are, and there is no typical description of an aura. Dizziness, nausea and blurred vision, on the other hand, can be associated with migraine.
The bruxism is irrelevant. It may be associated with masticatory muscle tenderness but is usually asymptomatic.
▪ What is the role of the dentist in headache diagnosis and treatment?
It would be wise to consider this question before dismissing the complaint, referring to a medical practitioner or taking on analysis of the problem. A dentist would be expected to have a fairly broad knowledge of signs, symptoms and causes of craniofacial pain, but mainly for diagnostic and patient referral purposes.
The primary role of the dentist in headache is to exclude pain of dental or local origin. This is most important but not always easy.
The key causes of pain of dental origin that might present as headache are:
• Pulpitis and referred pain of dental origin
• Sinusitis
• Temporomandibular joint/myofascial pain dysfunction.
In addition some causes of head and neck pain can be misinterpreted by the patient as pain of dental origin and so present to the dentist. The key causes to consider are:
• Trigeminal and other neuralgias
• Giant cell arteritis
• Chronic idiopathic (atypical) facial pain.
The dentist should be very familiar with these causes of pain and should also be able to diagnose many others.
However, it is not the role of the dentist to undertake primary diagnostic responsibility for other causes of headache or facial pain. Craniofacial pain is usually managed by a multidisciplinary team, which may well include a dentist, and in such a setting the dentist may take on considerably more responsibility. In other settings the dentist will not have the necessary neurological knowledge or access to investigations.
Your management of true headache, whether in primary or secondary care, should be limited to:
• Identifying and treating dental causes or
• Making a provisional diagnosis
• Ensuring appropriate referral
• Informing the patient about possible causes and treatments.
One of the most important factors is to be able to identify any sinister signs that might indicate significant underlying disease.
▪ What further information do you need?
You will need to question the patient for further details about the features in the left-hand column of Table 66.1. When you do this, the patient gives the answers shown on the right.
▪ How can pulpitis be excluded as a cause of craniofacial pain?
Toothache is the commonest cause of pain sensed by the trigeminal system. Diagnosis of toothache is discussed in several other problems. The key features of pulpitis are that it may be intermittent or constant, sometimes with a dental trigger, exacerbated by hot, cold and osmotic stimuli and may be poorly localized. Periapical periodontitis, sensed in the periodontal ligament, is well localized and sensitive only to pressure. Pain from multirooted teeth may have both a pulpal and periodontal component.
The main problems in excluding pulpal pain are caused by teeth with cracks or low-grade chronic pulpitis, such as in teeth with leaking restorations or small amounts of caries below restorations. When a cause is not evident it may be necessary to investigate a number of teeth by tests of vitality, replacement of restorations and by placing orthodontic bands or copper rings to exclude cracks; this may be quite time-consuming and require several visits. Short stabbing neuralgia-type pain from a pulpitic or cracked tooth can often be detected with cold stimulation or by applying biting pressure on to individual cusps.
One of the most useful diagnostic features of toothache is the patient’s interpretation of the pain. In past decades, when dental disease was prevalent, most patients would have sufficient experience to make a clear diagnosis themselves. Now that caries is less prevalent and less extensive, patients may have no experience of either the severity or poor localization of toothache and so attribute the pain to other causes.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


