Case• 64. A pain in the neck
SUMMARY
A 51-year-old man has a recurrent swelling in his neck at mealtimes. What is the cause and how may he be treated?
History
Complaint
The patient has a swelling in the left neck, below the angle of the jaw in the submandibular region. It appears suddenly on eating and is painful, lasts 1 or 2 hours and then slowly subsides. He reports that the swellings are worse when eating citrus fruit. The swelling is still present following his last meal.
History of complaint
The swelling first appeared suddenly during a meal 4 months ago. It resolved within 2 hours but recurred once during the following week. In the following weeks the swelling appeared more frequently and then, on one occasion stayed swollen for 3 days. This swelling appeared different; the swelling was warm to touch and more painful. He consulted his medical practitioner and was prescribed amoxicillin and the swelling resolved shortly afterwards. After that episode the recurrent swelling did not appear for nearly 2 months but it now appears daily. The patient’s medical practitioner has suggested that he see a dentist to exclude a dental cause for the swelling.
Medical history
The patient is an otherwise fit and healthy man.
▪ How do you interpret the information you have so far?
The patient is almost certainly suffering from the symptom known as mealtime syndrome, swelling of a salivary gland associated with eating or the thought of eating. Provided the swelling is in the correct site to be a salivary gland, this will be the underlying process. The cause of mealtime syndrome is obstruction. Between meals the low flow of saliva leaks around a partial obstruction. When flow is stimulated the saliva is held back, causing the gland to swell and inducing pain because the gland is restricted within a capsule.
This accounts for the recurrent swelling but the patient’s episode of persistent swelling appears to be infectious. The classical signs of inflammation were present and the swelling resolved on antibiotics (though the causative link between the resolution and antibiotic is conjectural). When salivary flow is reduced the gland is prone to ascending infection by oral commensal bacteria and opportunistic pathogens so the two causes of swelling could well be linked.
▪ Are there any specific questions you would ask? Why?
Whether the patient has noticed any abnormality of salivary flow such as a foul tasting saliva or sudden resolution of the swelling following a sudden discharge of saliva or salty fluid into the mouth. The first would suggest infection and the second would confirm intermittent obstruction.
Examination
Extraoral examination
▪ The appearance of the swelling is shown inFigure 64.1. What do you see?
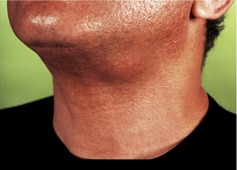 |
| Fig. 64.1 |
The patient has a round swelling of approximately 3 cm in diameter in the region of the left submandibular gland, below the lower border of the mandible on the left side and just anterior to the angle of the mandible. If you were able to palpate the neck you would feel no cervical lymphadenopathy and find that the swelling is firm, mobile and tender.
Intraoral examination
▪ What features of the intraoral examination are important?
Bimanual palpation of the submandibular gland will allow the gland to be steadied for examination. Palpation from only one side displaces the mobile gland, making differentiation of the gland from an enlarged lymph node or swelling of the gland from swelling in the gland difficult.
Expression of saliva from the salivary gland ducts. Massaging the duct should produce a free flow of clear saliva. Cloudy saliva indicates infection or inflammation. No saliva may indicate reduced secretion or blockage. Pus indicates infection and a sample should be taken for culture and sensitivity.
When you examine the patient you discover that the oral mucosa and dentition appear normal. A small amount of clear saliva can be expressed from the orifice of the left submandibular duct. Bimanual palpation reveals a 3 cm diameter hard mass in the floor of mouth near the posterior free border of mylohyoid muscle. The mass is freely mobile vertically and appears to be the submandibular gland.
Diagnosis
The patient has mealtime syndrome and probably obstruction. The gland is hard because of recurrent sialadenitis, a result of ascending low-grade infection.
▪ What are the possible causes of obstruction?
| Type | Cause |
|---|---|
| Intraductal causes (common) |
Sialolithiasis (stone)
Mucous plug
Stricture
|
| Extraductal causes (rare) |
Trauma
Pressure from adjacent neoplasm or other swelling
|
▪ Are there any other causes of intermittent swelling that need to be considered?
Yes. Intermittent swelling may be associated with overvigorous rinsing (particularly with chlorhexidine) or in wind instrument players who force air or liquids back into the gland. A number of other chronic conditions that cause persistent swelling may cause intermittent swelling in their early stages. These include sialadenitis (usually the result of obstruction), primary Sjögren’s syndrome, sialosis, drug-induced salivary gland swelling (caused by iodine-containing compounds, phenylbutazone and other drugs). However, this last group do not cause such obvious and short-lived swelling as obstruction.
Investigations
▪ What investigations are required? Why?
Investigations are required to plan treatment rather than confirm the diagnosis. The information required is the cause of the blockage, the site of the blockage and the degree of damage sustained by the gland and ducts from sialadenitis. Useful investigations are shown in Table 64.1.
| Investigation | Rationale and role |
|---|---|
| Plain radiograph | Simple to perform, suitable for detection of radiopaque stones in ducts or the submandibular gland; a lower true occlusal film for the submandibular duct or a lateral view of the upper neck, oblique lateral or panoramic tomogram for the gland itself. The parotid duct may be visualized in a posteroanterior jaws view with the cheek blown out. Useful for submandibular calculi because 60–80% are radiopaque but of less value in the parotid where only 20–40% of calculi are radiopaque and other tissues are superimposed on the image. Radiolucent ‘stones’ are unmineralized or poorly mineralized masses of inspissated mucin. |
| Sialogram |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


