Case• 58. A complicated extraction
SUMMARY
A 35-year-old man attends your general dental practice surgery requesting extraction of a tooth.
History
Complaint
He points to the lower left second premolar and says that the tooth is very tender to touch.
History of complaint
The tooth has been tender for some months and root canal treatment at another surgery was initially successful but has proved ineffective in the longer term.
Medical history
The patient’s medical questionnaire indicates no relevant medical conditions.
Examination
Extraoral examination
The extraoral examination is normal except for a few palpable but normal-sized lymph nodes in his right and left cervical chain.
Intraoral examination
You immediately notice that the patient’s oral mucosa is not normal. The appearance of the palate is shown in Figure 58.1.
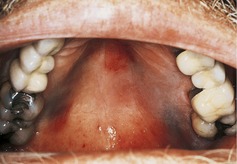 |
| Fig. 58.1 |
The lower left second premolar has a large amalgam restoration and is tender to percussion. A sinus is present over the apex and the tooth does not respond to a test for vitality.
▪ What do you see in the patient’s mouth?
• The palate appears bruised with two purple-coloured lesions, one on each side of the palate extending from the gingival margin up the sides of the vault. Neither lesion appears to be raised above the surface.
• There is a discrete sharply defined slightly red patch in the anterior palate, just to the left of the midline.
• There are a few scattered red spots on the soft palate.
▪ What do these changes tell you?
Individually none of these lesions can be diagnosed on the basis of the appearance alone. However in combination the appearances are almost diagnostic. The purple lesions appear vascular and could be haemangiomas or another blood vessel lesion including Kaposi sarcomas. The red patch has the characteristic appearance of erythematous/chronic atrophic candidosis. Both lesions are associated with immunosuppression, and you should immediately suspect HIV infection because Kaposi sarcoma is extremely rare with other causes of immunosuppression. In this clinical setting the palpable lymph nodes also support this diagnosis. It is almost certain that the patient is HIV-positive.
▪ What do you need to know? What would you say to the patient?
You need to identify whether the patient is aware of his HIV infection but has chosen not to tell you the full medical history, or whether he is completely unaware of it. Almost all patients who know that they are HIV-positive will tell their dentist provided they are asked in an appropriate manner. Sometimes patients withhold the information because of previous insensitive management, a dentist having refused to provide treatment or because they are worried that practice confidentiality cannot be relied on. However, your questions need to be phrased to take account of the fact that the patient may be unaware of his HIV infection. It is very important that you approach this matter with sensitivity. You could adopt the following line of questioning.
• Tell the patient that he has some unusual signs in his mouth which you cannot easily explain. Ask whether he has noticed them.
• Point out that there are several possible reasons for being prone to infection and that it would be worthwhile investigating further to find the cause. Proffer examples such as anaemia, immunosuppression as a result of steroid therapy or viral infection. Patients who know that they are at risk of HIV infection may often use the prompt of a viral infection to discuss the possibility.
• If the patient indicates that they are HIV positive, ask whether you might have their clinic address so that if necessary you may make contact for medical advice relating to dental treatment.
• If the patient gives no indication that they are HIV-positive, they should be referred to their general medical practitioner or to a specialist oral medicine or oral surgery unit for further investigation.
It is inappropriate to ask questions about lifestyle or sexuality. Even pointing out that HIV infection is one potential cause of the oral signs may not be well received in a dental setting. It would be reasonable to check the medical history questionnaire, including whether the patient has recorded coming into contact with someone with HIV infection or AIDS.
If the patient discloses HIV infection you should respond positively and acknowledge that you will respect the confidentiality of this sensitive information.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


