Case• 56. Rapid breakdown of first permanent molars
SUMMARY
A 7-year-old boy presents with first permanent molar teeth which his parents say have decayed rapidly, starting immediately on eruption. Identify the cause and discuss the treatment options.
History
Complaint
The child complains of pain from his back teeth on both sides. The pain is worse with sweet foods and cold liquids and persists for several minutes after stimuli. Toothbrushing with cold water is also painful but the teeth do not cause pain on biting.
History of complaint
The pain has been present for a few months and has increased in severity over the last month. The child now reports that one of his back teeth feels broken. The first permanent molars erupted on time and his mother noticed that some of them appeared to crumble as soon as they emerged through the gum. She has read in magazines that fluoride can damage teeth and has switched to a toothpaste without fluoride on the assumption that this is the cause.
Medical history
The patient is a healthy child, the only history of note being neonatal jaundice.
Dental history
The child has no experience of operative dental care. A diet history reveals a reasonably well-balanced diet, with limited consumption of refined carbohydrates and carbonated beverages. Toothbrushing has been performed with adult-formula fluoride-containing toothpaste, starting at approximately 1 year and continuing until 7 years of age.
Examination
Extraoral examination
The child has no facial swelling or asymmetry and no lymph nodes are palpable.
Intraoral examination
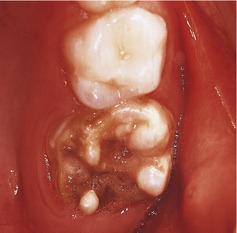
He is in the early mixed dentition stage. All four first permanent molars have areas of brown, rough, irregular enamel. The severity varies between the teeth and the worst affected are the maxillary molars whose enamel appears to be completely absent in some areas. These teeth have soft dentine exposed occlusally. The lower right first permanent molar is the least severely affected with only a small localized brown enamel defect on the buccal aspect. This is hard on probing. In addition, there are areas of white enamel opacity in the incisal third of the labial surface of all permanent central and lateral incisors, which are most pronounced in the maxillary central incisors. The remaining primary dentition is caries free, and appears normal in structure and morphology. Oral hygiene appears good. The appearances of the dentition are shown in Figures 56.1 and 56.2.
▪ On the basis of what you know already, what do you suspect?
The defects appear to be hypoplasia or hypomineralization of the enamel which has either become carious or taken up extrinsic stains. The molars are so severely affected that diagnosis is difficult, but the opaque white zones on the central incisors are characteristic of enamel hypoplasia. Hypoplasia is the result of reduced ameloblast numbers or activity. Enamel is missing so that the surface contour is abnormal. A hypomineralized enamel usually has normal contour initially but is softer than normal and may be worn away.
▪ Do the enamel defects follow a chronological pattern, and if so, at what time was the affected enamel formed?
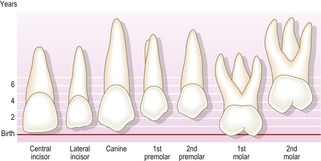
Almost, the incisal and occlusal parts of the permanent central incisors and first molars form at about the same time, starting to mineralize just before birth. The affected enamel would have been formed after birth and during the first 1–2 years of life. This may be seen by consulting Figure 56.3.
This distribution of hypoplasia is often referred to as molar–incisor hypoplasia. There is some evidence that molar-incisor hypoplasia is not completely chronological. The occlusal and buccal surfaces tend to be worst affected. Canines and premolars are unaffected despite mineralizing at the same time. Defects may be asymmetrical and enamel loss may be a secondary phenomenon.
▪ What additional questions would you ask, and why?
A chronological pattern suggests systemic illness which may be identifiable in the history. Defining a possible cause may allow others such as fluorosis to be excluded. You need to ask further details about the prenatal and perinatal medical history. The following conditions may be relevant and should be specifically sought:
• Preterm birth or low birth-weight baby
• Rhesus incompatibility
• Intubation as neonate
• Maternal vitamin D deficiency.
These disturbances may manifest as enamel defects distributed along the enamel formed around birth. You should also enquire about all severe systemic disturbances in the first 2 years of life, for example meningitis, encephalitis, severe measles or pneumonia. Even relatively minor fevers or infections, such as ear infections, are known to be associated with similar enamel defects.
 |
| Fig. 56.1 |
 |
| Fig. 56.2 |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses