Case• 52. Refractory periodontitis?
SUMMARY
A 30-year-old male patient is referred for periodontitis that has not responded to treatment. What is the cause and how would you proceed?
History
Complaint
The patient complains that he has been undergoing intensive treatment for gum disease, but with little success. His upper right first molar is slightly loose and his dentist wishes to extract it. He would like a second opinion.
History of complaint
The gum disease was noted 9 months ago. He has never had pain or discomfort from the tooth.
Dental history
The patient has attended for dental treatment and prevention regularly. He has no dental restorations, no caries and no other oral problems. The previous dental practitioner has undertaken intensive oral hygiene instruction, scaling and root planing, with regular hygienist review. The patient flosses his teeth daily and brushes twice a day with a fluoride toothpaste, and occasionally uses a disclosing agent.
Medical history
The patient is fit and well.
▪ What are your initial thoughts?
Periodontal disease is often difficult to treat. Many patients are not able to maintain a sufficiently effective oral hygiene regime. However, this patient appears to be doing all the correct things. It remains possible that he is not cleaning effectively despite his efforts and this must be assessed. There may be local predisposing causes such as subgingival calculus to account for localized disease. There has been sufficient time for improved cleaning to have had an effect.
Examination
Extraoral examination
The extraoral examination is normal. No lymph nodes are palpable.
Intraoral examination
One lower third molar is partially erupted; the upper third molars are unopposed and distally inclined. There is no dental caries and no restorations are present.
The oral hygiene is very good. Only a few flecks of interdental plaque are present. The gingivae in most areas are healthy in appearance and do not bleed on probing.
However, there are three areas of concern:
1. The upper right first molar is mobile about 1 mm in the buccopalatal direction. It is not depressible in the socket. A 9 mm probing depth is present distally and the furcation can be probed, though not from the buccal aspect. The gingivae appear loose but they are not oedematous and there is only slight bleeding on probing. Inflammation appears diffuse rather than related to the gingival margin or pocket. The gingiva lifts easily from the tooth.
3. There is a 6 mm pocket on the mesial of the lower left second molar with no bleeding on probing.
Investigations
▪ What do you see in the two periapical views that the patient has brought?
The top film (Figure 52.1) shows extensive bone loss distally to the first molar. There is loss of lamina dura around the whole of the distal root, into the furcation and around the apex. No calculus is visible.
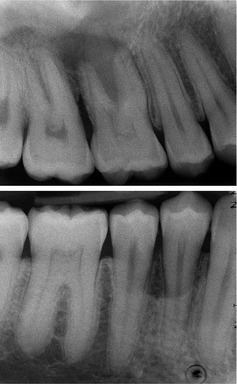 |
| Fig. 52.1 |
The lower film shows a curved area of alveolar bone loss associated with the first and second premolars. The lamina dura and alveolar crest appear intact on both teeth. The bone loss would be consistent with the probing depth. No calculus is visible.
▪ What further investigations are required?
The vitality of the upper first molar must be determined. Bone loss involves the furcation and there is a significant chance of loss of vitality. The apical lamina dura is not clearly defined, giving rise to further suspicion.
A radiograph is required to show the bone levels around the lower left molars, and possibly other teeth. However, before selecting a suitable view, some further thinking is required.
In the meantime you check the vitality of the upper right first molar. It is vital and not hypersensitive to cold and electric pulp testing.
Differential diagnosis
▪ What are your thoughts now?
This is odd. The patient is motivated and the oral hygiene is good but there are three areas of localized periodontitis and these cannot be accounted for by local factors such as overhanging restorations, calculus or plaque traps.
Perhaps the patient has a form of aggressive periodontitis. This is defined by rapid attachment and bone loss, sometimes with a familial pattern. The sites of lesions, on two first molars and one premolar, the age of the patient and failure to respond to treatment suggest the localized juvenile periodontitis pattern of aggressive periodontitis, though premolars are not usually affected unless several other molars and incisors are. Perhaps some adjunctive treatment with antibiotics might help?
Perhaps the patient has some systemic predisposition to periodontitis. The most likely would be diabetes or smoking. However, diabetes would have to be undiagnosed or poorly controlled to contribute to this severity of disease. Both diabetes and smoking exacerbate periodontitis in a generalized plaque-associated distribution, and do not predispose to localized disease.
Other medical predisposing conditions include neutropenia, Down’s syndrome and rare developmental neutrophil defects. These become obvious in childhood and can be excluded.
▪ Is this refractory periodontitis?
No, this term was removed from the classification of periodontal diseases in the 1999 International Workshop for the Classification of Periodontal Diseases. Prior to this it had been thought a separate entity but it was realized that there were many factors that could cause treatment to fail, including furcation involvement, smoking, microbiological and host factors. If diseas/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


