Case• 49. A swollen face
SUMMARY
A 30-year-old man is referred to your dental hospital by his general practitioner with a painful swelling of the right side of the face. What is the cause and what treatment would you provide?
History
History of complaint
The patient has had toothache intermittently for many months. A few weeks ago the pain became excruciating and did not respond to analgesics. Then, suddenly, it reduced in severity and the patient thought it had resolved.
However, about 10 days ago a different pain developed. A tooth on the upper right has become very tender and he has not been able to bite on it. The swelling suddenly enlarged yesterday.
Over the last few months the patient has been prescribed several courses of antibiotics and he finished a course of oral erythromycin 2 days ago.
Medical history
The patient is otherwise fit and well.
Examination
Extraoral examination
The patient is shown in Figure 49.1. The swelling is hot, tender and firm centrally but peripherally it is almost painless and softer. It extends from the nose to the anterior border of the masseter and the lower eyelid is very oedematous and contains blood pigment as if bruised.
 |
| Fig. 49.1 |
The swelling is not pointing extraorally. There are palpable tender lymph nodes in the upper deep cervical chain.
Intraoral examination
The patient has slight limitation of opening which does not significantly hamper examination. The sulcus adjacent to the upper first molar and both premolars is tender and slightly reduced in depth by a firm swelling. The upper first and second premolars and first molar have large amalgam restorations. However the patient indicates clearly that the second premolar is the cause of the pain and this tooth is slightly mobile and raised in its socket. It is very tender on percussion and nonvital on testing with ethyl chloride. The first molar and first premolar appear vital.
Investigations
▪ Which additional investigation is critically important? Why?
Taking the patient’s temperature. This gives a good indication of the systemic effects of the infection and reflects the amount of pus in abscesses and/or the tendency of the infection to spread. The patient has a temperature of 37.2°C.
▪ Would you take a radiograph?
In this case a radiograph is not a useful investigation. Tests of vitality are much more likely to identify the causative tooth and, in any case, there appears to be no doubt about the diagnosis.
However there are good reasons why taking a radiograph may not help or even be counterproductive:
1. It takes up to 3 weeks for radiographic changes to develop at the root apex after pulp necrosis.
2. The radiographic features may mislead if you attempt to use them to diagnose loss of vitality. When root apices are radiographed with the maxillary antrum superimposed, the normal periodontal ligament appears wider. This may be confused with early apical changes of infection.
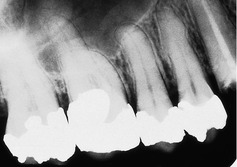
Both these problems are appreciated in Figure 49.2, the periapical radiograph of this patient, which is completely normal.
Diagnosis
▪ What do these findings tell you?
The combination of inflammation, the nonvital tooth and adjacent probable abscess indicate an odontogenic soft tissue infection. The history of severe toothache which suddenly resolved suggests pulpitis subsequently relieved by necrosis of the pulp. The subsequent pain of a different character with a tender tooth suggests an apical abscess. The patient points clearly to the second premolar and this is almost certainly the cause of the pain because pain involving the periodontal ligament is well localized.
Trismus is an important sign, indicating that infection or inflammation has spread to involve muscles of mastication. However, trismus is not severe and probably results from inflammation and oedema of the buccinator and the anterior fibres of the masseter which lie at the posterior border of the swelling.
The infection has induced minimal systemic effects and the patient is not significantly pyrexic. Luckily, the infection appears to be localized. The firm centre to the swelling and the swelling in the sulcus will contain pus.
▪ What types of soft tissue infection arising from teeth cause facial swelling? How may they be distinguished and what is the relevance of doing so?
Facial swelling may be the result of oedema, abscess formation, cellulitis or their combination.
It is important to determine which of these types of infection are present because the treatment and sequelae are different. Abscesses require drainage. Cellulitis requires aggressive treatment, usually including antibiotics, and oedema requires no direct treatment but resolves when the causative tooth is removed or the pulp treated.
Despite the fact that these terms are convenient, in practice most odontogenic soft tissue infections are caused by a mixed microbial flora and do not fall neatly into one category or another. It is not unusual to find an abscess with a surrounding zone of cellulitis and a degree of oedema is always present. Which type of infection develops is determined by the virulence of the pathogens (and synergy between species in the mixed flora), the resistance of the host and the anatomical constraints on the infection.
| Cause of swelling | Features |
|---|---|
| Oedema | Soft, not very red or hot, not tender on palpation and not painful. Compressible with slow continuous pressure. Often accounts for much of the facial swelling in children with odontogenic infection. |
| Abscess | Localized collection of pus which feels hard if small, tense or covered by a thick layer of tissues. If large it may be softer and exhibit fluctuance. Pointing to the skin or mucosa indicates abscess formation. |
| Cellulitis | Brawny, poorly localized swelling with marked tenderness and dusky redness. May contain small collections of pus but no large localized abscesses. Spreads, sometimes rapidly, through tissues. Usually associated with systemic symptoms, pyrexia, malaise, leucocytosis and lymphadenitis. |
▪ If infections are not easily characterized, what are the important features on which treatment must be based?
The critical factors which must be determined are whether:
• an abscess cavity is present (palpation, eliciting fluctuation)
• there is evidence of systemic effects (malaise, pyrexia, a toxic-shocked appearance)
• the infection is spreading rapidly (judged by the history and observation during treatment)
• the patient is predisposed to infection (from the medical history).
▪ Which type of infection is this?
This appears to be primarily an abscess with surrounding oedema.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses