Case• 38. Advanced periodontitis
SUMMARY
A 56-year-old man has severe periodontitis. Diagnose and plan treatment for his condition.
History
Complaint
The patient complains of loose back teeth, particularly the last tooth on the lower right.
History of complaint
He has recently moved to your area and has been a regular dental attender. His previous dental practitioner diagnosed periodontal disease several years ago and organized repeated courses of oral hygiene instruction and scaling. Despite this, several teeth are loose though he has suffered no pain.
Three years ago the remaining upper right molar teeth became very loose and were extracted when abscesses developed. Subsequently two implant fixtures were placed because he could not tolerate partial dentures. An implant-retained bridge was planned but the implants remain unused.
Medical history
The patient is fit and well and no illness is revealed by his medical history questionnaire.
▪ What questions will you ask the patient? Explain why.
Ask about his tooth cleaning regime, because it is clearly failing. The patient tells you that he cleans his teeth three times a day using a modified Bass technique and changes his toothbrush at monthly intervals. He uses floss on his anterior teeth every day and occasionally on his molars and premolars where access is difficult.
Whether he smokes. Smoking is a risk factor for periodontitis.
Whether he is diabetic or has any other susceptibility to infection. This is relatively severe periodontitis and there is a history of multiple abscesses. These features do not necessarily indicate an underlying condition but it would be worthwhile to exclude diabetes. Other features which might suggest diabetes are a period of rapid tooth destruction in middle age, suggesting late-onset diabetes.
Examination
Extraoral examination
No cervical lymphadenopathy is present. The temporomandibular joint and mandibular movements appear normal.
Intraoral examination
The mucosa and soft tissues of the mouth are normal. The teeth present are:
Most molars contain small- to medium-sized amalgam restorations. No caries is detected.
The patient’s oral hygiene is fair but the lower second molar teeth and upper left molars are mobile. The plaque control around the anterior teeth is good with minimal deposits of plaque or calculus. There is bleeding on probing around most posterior teeth and increased probing depths of 7–8 mm around the molars. No recession is present.
▪ How will you assess the patient’s periodontal health and oral hygiene?
They will be assessed by a combination of measurements and indices.
The measurements are:
• recession
• probing depths
• attachment loss.
Recession and probing depth measurements are made at six points around the circumference of a tooth: mesially, at the midpoint and distally on the buccal and palatal surfaces. The distance from the cementoenamel junction to the gingival margin records the amount of recession. Probing depths are measured from the gingival margin to the base of the periodontal pocket. The sum of recession and probing depth gives the length of attachment loss.
The indices are described in Table 38.1.
| Index score | Significance of score | |
|---|---|---|
| Oral hygiene | ||
| Degree 0 | No plaque or debris | Reflection of effectiveness of cleaning. |
| Degree 1 | Looks clean but material can be removed from the gingival third with a probe. | |
| Degree 2 | Visible plaque | |
| Degree 3 | Tooth surface covered with abundant plaque. | |
| Bleeding on probing | ||
| Degree 0 | None | Healthy or inactive disease. |
| Degree 1 | Bleeding | Active disease. N.B. in smokers bleeding may be less than expected for the disease activity. |
| Tooth mobility | ||
| Degree 1 | Movement of the crown of the tooth between 0.2–1 mm in a horizontal direction. | Minor movement, possibly physiological. If periodontal disease present, treat conservatively. |
| Degree 2 | Movement of the crown of the tooth exceeding 1 mm in a horizontal direction. |
Caused by loss of attachment. The degree of mobility depends on remaining periodontal support and the shape of the roots.
Conical roots on molars are more likely to develop mobility than divergent roots on teeth with a similar degree of attachment loss.
|
| Degree 3 | Movement of the crown of the tooth in a vertical and horizontal direction. |
Indicates bone loss below the apex and little or no bony support.
Usually indicates a need for extraction.
|
| Furcation involvement | ||
| Degree 1 | Horizontal loss of supporting tissues not exceeding 1/3 of the width of the tooth. | Early furcation involvement, can be treated conservatively; predisposes to further and more rapid attachment loss if untreated. |
| Degree 2 | Horizontal loss of supporting tissue exceeding 1/3 but not a ‘through and through’ lesion | Much more difficult to keep clean. Unlikely to respond to conservative treatment. |
| Degree 3 | A ‘through and through’ lesion |
May be easier to clean depending on soft tissue contour. The prognosis for the tooth would depend upon the remaining amount of periodontal attachment and the length and shape of the roots.
Indicates susceptibility to furcation caries and risk of loss of vitality.
|
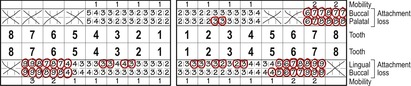
The results of these examinations are shown in Figure 38.1. The lower right second molar is mobile to grade 3. All other molars are mobile to grade 2 and there is bleeding on probing from most pockets. The anterior teeth have only 2–3 mm probing depths and no bleeding on probing or gross attachment loss.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses