Case• 36. Skateboarding accident?
SUMMARY
A 6-year-old boy with a facial injury attends late one afternoon without an appointment. Assess the child and decide what treatment he needs.
History
Complaint
The child complains of loose front teeth and that his mouth is sore and it hurts to eat.
History of complaint
The child’s mother says that he fell off his skateboard and banged his teeth. The injury occurred yesterday evening when he was playing at a friend’s house.
Dental history
The family attend your practice occasionally. The patient had some primary molars extracted under general anaesthesia 6 months ago and has since missed two appointments for review.
Medical history
The patient is otherwise fit and well.
▪ What do you need to know about the accident?
Further details, including the exact time, whether it was witnessed by others and who was responsible for looking after him at the time. Was he knocked out when he fell?
What type of surface did he fall on? Were the abrasions or mouth contaminated with soil or other dirty material? Is the patient’s antitetanus immunization up-to-date?
Examination
Extraoral examination
The child looks anxious and withdrawn. Abrasions are present on the tip of the nose and the upper lip, as shown in Figure 36.1. These have a parallel vertical pattern consistent with scraping on a pavement but are not visibly contaminated with debris. When asked if he has injuries elsewhere, he does not respond at first then shows abrasions on his knees and elbows.
 |
| Fig. 36.1 |
On examining his face, you notice faint parallel lines of petechial bruising running horizontally across the left side of his neck (Figure 36.2) and bruising on both the outer and inner surface of the right ear (Figure 36.3). No other injuries are visible on those parts of his arms and legs which are not covered by clothing.
 |
| Fig. 36.2 |
 |
| Fig. 36.3 |
Intraoral examination
The patient’s upper anterior teeth and lip are shown in Figure 36.4.
▪ What do you see?
He is in the early mixed dentition, has poor oral hygiene and no obvious caries. There are abrasions on the vermilion border and inner surface of the upper lip. The upper labial frenum is torn and bruised. The upper left primary central incisor has bleeding around the gingival margin and is displaced palatally.
 |
| Fig. 36.4 |
If you were to examine the patient you would find that both upper primary central incisors are slightly mobile and tender to pressure. The displaced incisor is not causing occlusal interference.
Whether he has already received any medical attention and why they did not seek dental care sooner. Who was looking after the child when he was injured?
You should also ask the child himself about the cause of the injury, particularly allowing him to talk and volunteer information without asking leading questions.
When you ask the patient what happened to him, he looks away and says nothing. When you note the marks on the neck and ear, his mother looks uncomfortable and says, ‘He fell off a wall last week. He’s very accident-prone.’
Investigations
▪ What radiographs would you take and why?
A periapical view of the primary upper incisors should be taken to show the extent of physiological root resorption, any displacement or root fractures and the proximity of the developing permanent incisors. As well as aiding diagnosis the radiograph will act as a baseline for future monitoring.
If a periapical film is too uncomfortable to hold, an occlusal view or occlusal taken with a periapical film or detector may prove more acceptable.
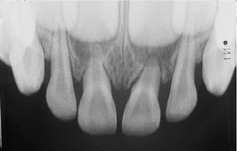
▪ The radiograph is shown inFigure 36.5. What do you see?
 |
| Fig. 36.5 |
All permanent incisors are present and appear to be relatively distant from the primary tooth roots. There is resorption of the upper primary central incisor roots consistent with the patient’s age.
There is increased periodontal ligament space and displacement of the upper left primary central incisor but no other abnormalities.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


