Case• 20. A lump in the neck
SUMMARY
A 55-year-old man presents to your oral and maxillofacial surgery department clinic with a lump on the left side of the neck. You must make a diagnosis.
History
Complaint
The patient complains of the lump and notices some discomfort on swallowing, as if something is stuck in his throat. He assumes the lump is the cause.
History of present complaint
He thinks he first noticed the lump about 3 months ago. It has always been painless and is slowly enlarging. The discomfort on swallowing is of recent onset.
Medical history
The patient is otherwise fit and well. He smokes 20 cigarettes per day and drinks 10 units of alcohol each week as beer.
Examination
Extraoral examination
The appearance of the swelling is shown in Figure 20.1.
▪ What do you see? What is the likely origin of the mass?
There is a swelling just anterior to the anterior border of the sternomastoid muscle and below and behind the angle of the mandible. It is several centimetres in diameter and extends forwards below the angle of the mandible towards the submandibular region. The overlying skin does not appear to be inflamed.
The lesion lies over the deep cervical lymph node chain and could well arise from a cervical lymph node. It is too low and too far posterior to be arising from the submandibular gland and too low to have arisen in the lower pole of the parotid gland. Other soft tissues of the neck could be the origin, but a lymph node is the most likely cause.
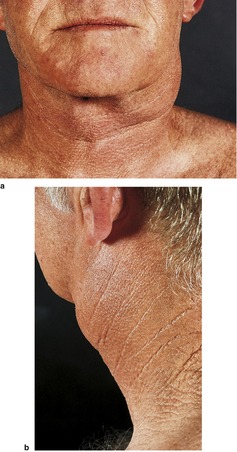 |
| Fig. 20.1 |
If you could palpate the lesion you would find that it is approximately 8 cm by 6 cm in size and feels firm on palpation, possibly slightly fluctuant. It is mobile, not fixed to the overlying skin or deep structures. The patient does not notice any tenderness on palpation. There are no other swellings or enlarged lymph nodes palpable on either side of the neck.
Intraoral examination
The submandibular glands are palpable bimanually and appear symmetrical. Both are mobile and clearly separate from the swelling, which lies posterior to the gland.
The patient’s mouth has been well restored in the past but suffers from recent neglect and several carious cavities are visible. There is no significant periodontal disease with most probing depths less than 5 mm and no mobile teeth. The lower left first permanent molar has lost a large restoration and has extensive caries. There is no soft tissue swelling, sinus or tenderness in the sulcus adjacent to the apices of the roots. The tooth is not tender to percussion. The oral mucosa appears normal, and the tonsils appear to be symmetrical.
Differential diagnosis
▪ What are the most likely causes of the lump and why?
Metastatic malignancy appears likely and this lesion is so typical of a cervical lymph node metastasis that it must be considered to be malignant until proved otherwise. The combination of features suggestive of metastasis is the patient’s age (should be considered a possible cause in any patient aged over 45), the site (consistent with a cervical lymph node), the firm consistency and lack of tenderness. Fixation to the skin or other structures would be almost conclusive of malignancy but is a late sign. The patient is a smoker and drinker and so has an increased risk of malignancy. Either a squamous carcinoma or adenocarcinoma is likely. Melanoma and other malignancies are further possible causes.
Lymphadenitis secondary to a local cause is common and so must be considered. However there is no tenderness on palpation to suggest an inflammatory cause. If this were a reactive inflammatory enlargement, the most likely source of infection would be a dental, pharyngeal or skin infection. The patient has a potential source of dental infection in the lower left first permanent molar but the tooth is not tender to percussion nor associated with overt infection, making it an unlikely cause.
Tuberculosis needs to be considered both as a possible diagnosis and as a factor affecting management. Most patients with cervical lymph node enlargement caused by tuberculosis have reactivation (‘secondary’ or post-primary) tuberculosis in which a previous quiescent infection becomes reactivated. This localized infection may or may not be accompanied by pulmonary disease though there may be radiologial evidence of past tuberculosis on chest radiograph. Cervical tuberculous lymphadenitis is common in those from the Indian subcontinent. Atypical mycobacterial infection is a disease which often affects the cervical lymph nodes but is almost always seen in children or the immunosuppressed.
▪ Which additional but less likely causes need to be considered whenever a patient complains of an enlargement at this site? Why are they unlikely causes in this case?
Numerous lesions could arise at this site and it is not useful to list them all. A number of possible causes (Table 20.1) merit consideration, because they are common, easily excluded or cause significant morbidity.
| Cause | Reasons | |
|---|---|---|
| Developmental causes | Branchial cyst | Branchial cysts develop at this site. They usually present in childhood or early adulthood but can on occasion be asymptomatic for many years and present late with infection. However, 55 years of age would be extremely late and a metastatic malignancy is a much more likely cause. Cystic change in metastatic carcinoma in lymph nodes is a well-recognized finding and fluctuation can be misinterpreted as indicating a benign cyst such as a branchial cyst. Branchial cysts are rare. |
| Infectious causes | Cat scratch disease, toxoplasmosis, brucellosis, glandular fever |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


