Case• 18. Oroantral fistula
SUMMARY
A 42-year-old man presents with pain following extraction of an upper first molar. What is the cause and how will you treat him?
History
Complaint
The patient is suffering dull throbbing pain in his upper jaw and face on the left side only. Pressure below his eye is painful and all his upper teeth on the left are tender on biting. He has a nasal discharge and blocked nose on the left.
History of complaint
He has had the pain for 2 weeks following extraction of the upper left first molar by his dentist. The extraction was difficult and the roots required surgical removal. There was little pain immediately afterwards but pain has slowly developed so that it is now preventing him from sleeping. The pain is constant.
Medical history
He gives a history of smoking 20 cigarettes a day for 24 years but considers himself fit and healthy.
Examination
Extraoral examination
He is a healthy looking man with no facial swelling or lymphadenopathy. There is a lightly blood-stained discharge from the left nares and halitosis.
Intraoral examination
▪ The appearances on presentation are shown inFigure 18.1. What do you see and how do you interpret the features?
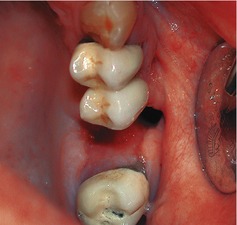 |
| Fig. 18.1 |
There is a large defect in the alveolus at the site of the first molar socket, the socket appears empty and the oral mucosa has grown to line the visible sides of the socket. After 2 weeks the oral epithelium should have proliferated to cover the socket mouth but there must have been a failure of clot formation and/or organization. One possibility is that the patient has a dry socket (see Case 15). No bone is visible in the socket but it could be exposed apically. However, dry socket is rare in the maxilla and it is more likely that the socket is communicating with the maxillary antrum.
Differential diagnosis
▪ What causes for this pain are possible and why?
Sinusitis secondary to oroantral fistula. An oroantral communication itself causes little or no discomfort but usually induces a degree of sinusitis. The nature and distribution of pain and presence of nasal discharge are typical of sinusitis. This seems the most likely diagnosis. Fistula formation is most commonly associated with extraction of maxillary first and second molars.
Dental pain. Before jumping to conclusions, it is worth considering whether the wrong tooth may have been removed. If the extraction was performed for pulpitis (which is often poorly localized), it is possible that at least some of the symptoms may arise from the adjacent teeth. You will need to check whether additional symptoms suggest pain of dental origin.
▪ What is an oroantral fistula?
An oroantral fistula (OAF) is a persistent epithelialized communication between the maxillary antrum and the mouth, present for more than 48 hours. The epithelial lining of the fistula grows from the gingival epithelium, periodontal pocket lining or the antral lining and it may take up to 7 days for the epithelium to completely line the walls of the communication. If the tract is not lined by epithelium it is known as an oroantral communication or perforation. Oroantral communications either close spontaneously or become epithelialized and persist as fistulae.
▪ What is the aetiology of oroantral fistula?
The vast majority of oroantral fistulae result from dental extraction. Up to 10% of upper molar extractions may create oroantral communications but very few, only 0.5%, persist to become fistulae. Other causes include malignant neoplasms arising in the oral cavity or antrum.
▪ What factors predispose to formation of oroantral fistulae following extraction of teeth?
• Proximity of roots to maxillary antrum, large sinus
• Difficult extraction, unfavourable root morphology
• Periapical lesions such as apical granulomas or cysts
• Bone loss due to periodontitis or periapical–endodontic lesion
• Hypercementosis
• Local infection or sequestrum
• Predisposition to infection (e.g. diabetes)
• Dry socket or other poor healing
• Advanced age
• Pre-existing diseases in the sinus, though this is probably not a very significant factor.
▪ What are the signs and symptoms of OAF?
The symptoms depend on the size of the fistula. Initially there may be persistent pain localized to the tooth socket but later, when inflammation has subsided, the fistula will be painless. If pain is a prominent symptom, some additional element such as infection must be suspected. The socket may present as an empty cavity or as a prolapse of antral lining through the socket into the mouth.
The most characteristic symptoms are the escape of fluids from the mouth into the nose on eating, or air or fluid into the mouth on blowing the nose. Passage of saliva, food and bacteria into the antrum causes sinusitis and the symptoms experienced will depend on its severity. Unilateral nasal obstruction, a feeling of fullness, pain over the maxilla and tenderness on pressure are typical.
Investigations
▪ What investigations would you carry out, how and why?
Investigations need to be performed to confirm the communication with the antrum, to check for associated complications and to exclude the possibility that a malignant neoplasm is the cause of either the antral communication itself or the failure of the socket to heal. Investigations are summarized in the Table 18.1.
| Aim of investigation | Methods |
|---|---|
| To demonstrate communication between antrum and mouth, the definitive test for oroantral fistula if there is no history of fluid or air passing between sinus and mouth. | If the fistula is large it may be possible to see into the antrum or pass a probe or large gutta percha point through into the antrum. If not, the patient can be asked to blow air into their nose while pinching the anterior nares closed and keeping their mout/> |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


