Case• 1. A high caries rate
SUMMARY
A 17-year-old sixth-form college student presents at your general dental surgery with several carious lesions, one of which is very large. How should you stabilize his condition?
History
Complaint
He complains that a filling has fallen out of a tooth on the lower right side and has left a sharp edge that irritates his tongue. He is otherwise asymptomatic.
History of complaint
The filling was placed about a year ago at a casual visit to the dentist precipitated by acute toothache triggered by hot and cold food and drink. He did not return to complete a course of treatment. He lost contact when he moved house and is not registered with a dental practitioner.
Medical history
The patient is otherwise fit and well.
Examination
Extraoral examination
He is a fit and healthy-looking adolescent. No submental, submandibular or other cervical lymph nodes are palpable and the temporomandibular joints appear normal.
Intraoral examination
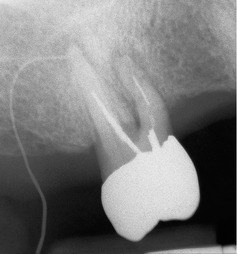
The lower right quadrant is shown in Figure 1.1. The oral mucosa is healthy and the oral hygiene is reasonable. There is gingivitis in areas but no calculus is visible and probing depths are 3 mm or less. The mandibular right first molar is grossly carious and a sinus is discharging buccally. There are no other restorations in any teeth. No teeth have been extracted and the third molars are not visible. A small cavity is present on the occlusal surface of the mandibular right second molar.
▪ What further examination would you carry out?
Test of tooth vitality of the teeth in the region of the sinus. Even though the first molar is the most likely cause, the adjacent teeth should be tested because more than one tooth might be nonvital. The results should be compared with those of the teeth on the opposite side. Both hot/cold methods and electric pulp testing could be used because extensive reactionary dentine may moderate the response.
The first molar fails to respond to any test. All other teeth appear vital.
Investigations
▪ What radiographs would you take? Explain why each view is required.
| Radiograph | Reason taken |
|---|---|
| Bitewing radiographs | Primarily to detect approximal surface caries, and in this case also required to detect occlusal caries. |
| Periapical radiograph of the lower right first molar tooth, preferably taken with a paralleling technique | Preoperative assessment for endodontic treatment or for extraction should it be necessary. |
| Panoramic radiograph | Might be useful as a general survey view in a new patient and to determine the presence and position of third molars. |
▪ What problems are inherent in the diagnosis of caries in this patient?
Occlusal lesions are now the predominant form of caries in adolescents following the reduction in caries incidence over the past decades. Occlusal caries may go undetected on visual examination for two reasons. First, it starts on the fissure walls and is obscured by sound superficial enamel, and secondly lesions cavitate late, if at all, probably because fluoride strengthens the overlying enamel. Superimposition of sound enamel also masks small and medium-sized lesions on bitewing radiographs. The small occlusal cavity in the second molar arouses suspicion that other pits and fissures in the molars will be carious. Unless lesions are very large, extending into the middle third of dentine, they may not be detected on bitewing radiographs.
▪ The radiographs are shown inFigure 1.2. What do you see?
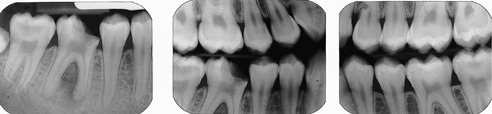 |
| Fig. 1.2 |
The periapical radiograph shows the carious lesion in the crown of the lower right first molar to be extensive, involving the pulp cavity. The mesial contact has been completely destroyed and the molar has drifted mesially and tilted. There are periapical radiolucencies at the apices of both roots, that on the mesial root being larger. The radiolucencies are in continuity with the periodontal ligament and there is loss of most of the lamina dura in the bifurcation and around the apices.
The bitewing radiographs confirm the carious exposure and in addition reveal occlusal caries in all the maxillary and mandibular molars with the exception of the upper right first molar. No approximal caries is present.
▪ If two or more teeth were possible causes of the sinus, how might you decide which was the cause?
A gutta percha point could be inserted into the sinus prior to taking the radiograph, as shown in Figure 1.1. A medium- or fine-sized point is flexible but resilient enough to pass along the sinus tract if twisted slightly on insertion. Points are radiopaque and can be seen on a radiograph extending to the source of the infection, as shown in another case in Figure 1.3.
Diagnosis
▪ What is your diagnosis?
The patient has a nonvital lower first molar with a periapical abscess. In addition he has a very high caries rate in a previously almost caries-free dentition.
Treatment
The patient is horrified to discover that his dentition is in such a poor state, having experienced only one episode of toothache in the past. He is keen to do all that can be done to save all teeth and a decision is made to try to restore the lower molar.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses