Over the past few decades, dental implants have been found to have high predictability and survival rates because of improvements in knowledge, clinical expertise, and implant designs. As such, dental implants are frequently integrated in the clinical management of fully or partially edentulous patients. It is prudent to realize that despite the high early survival rates, dental implants do have their fair share of long-term esthetic, biological, and mechanical complications. Therefore, this paper aims to review the current evidence on the management of peri-implant diseases in an attempt to answer the following question: Can periimplantitis be treated?
Key points
- •
Periimplantitis can be treated, but the treatment outcome is not always successful or predictable.
- •
The combination of resective and regenerative surgical techniques seemed to have favorable treatment outcomes in the management of periimplantitis.
- •
It is best to prevent peri-mucositis, which is the precursor of periimplantitis. This prevention can be achieved by eliminating bacterial plaque through meticulous oral hygiene practices and professional mechanical debridement. In addition, other contributing factors, such as wrong implant position, poor patient selection, and the presence of residual cement or deep probing depths, should be corrected.
Introduction
Over the past few decades, dental implants have been found to have high predictability and survival rates because of improvements in knowledge and clinical expertise, together with technological advances in implant designs. They are thus integrated into the clinical management of fully or partially edentulous patients. However, having a high implant survival rate is not equivalent to long-term implant success, which is defined as having a functional and esthetic implant restoration with no pain, mobility, and suppuration and no more than 2 mm of radiographic peri-implant bone loss. Also, despite the high early survival rates, dental implants do have their fair share of long-term esthetic, biological, and mechanical complications. The incidence of esthetic complications might have reduced because of the recent introduction of zirconia, but the incidence of biological and mechanical complications remained high. Therefore, this paper aims to review the current evidence on the management of peri-implant diseases in an attempt to answer the following question: Can periimplantitis be treated?
Definition
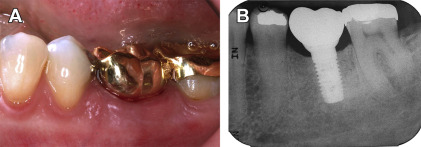
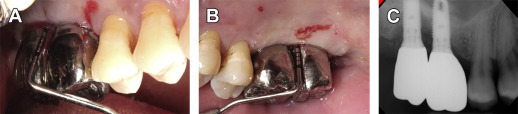
Peri-implant diseases, which are infectious inflammatory diseases of the peri-implant tissues, can be broadly categorized into peri-implant mucositis and periimplantitis. In sites with peri-implant mucositis, the inflammatory lesion is found to be limited to the peri-implant soft tissues with no evidence of progressive peri-implant bone loss beyond the initial physiologic bone remodeling that occurred following implant placement ( Fig. 1 ). Sites with periimplantitis, on the other hand, exhibit progressive peri-implant bone loss following the initial physiologic bone remodeling that occurred after implant placement as the inflammatory lesion progresses in both the mucosa and bone ( Fig. 2 ). As the discriminating feature is progressive bone loss beyond physiologic bone remodeling, it is, thus, important to establish baseline peri-implant bone levels, which is recommended to best occur at the time of prosthesis installation. Changes in bone levels from the time of implant placement to prosthesis installation are considered the result of physiologic bone remodeling or early implant failure. Therefore, it is challenging to determine the baseline peri-implant bone levels for immediately loaded implants, as time is not allowed for physiologic bone remodeling.