Many bone grafting techniques have been used to reconstruct the partially dentate and edentulous mandible. This article discusses the various bone grafting techniques to reconstruct mandibular defects. Also included are issues such as whether autogenous bone is necessary for reconstruction of the mandibular ridge and the importance of membranes.
Multiple bone grafting techniques have been used to reconstruct the partially dentate and edentulous mandible. Many of these techniques have been successful. In this article, the various bone grafting techniques to reconstruct mandibular defects are reviewed. Other issues discussed include whether autogenous bone is necessary for reconstruction of the mandibular ridge and the importance of membranes.
Block onlay grafts
Block onlay grafts have been used extensively for reconstruction of mandibular alveolar defects. Autogenous and nonautogenous options are available for vertical and horizontal deficiencies of the mandible. Autogenous bone grafts have the advantage of transferring osteogenic cells to the recipient site. Autogenous donor sites for block grafts include the calvarium, mandible, zygoma, and ilium. Intramembranous bone (calvarium, mandible, and zygoma) has the advantage of decreased rates of resorption compared with endochondral bone (ilium), due to its dense cortical structure and microarchitecture.
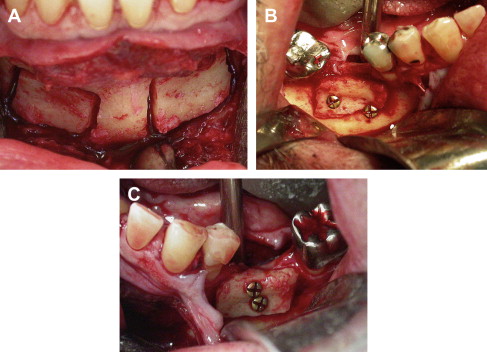
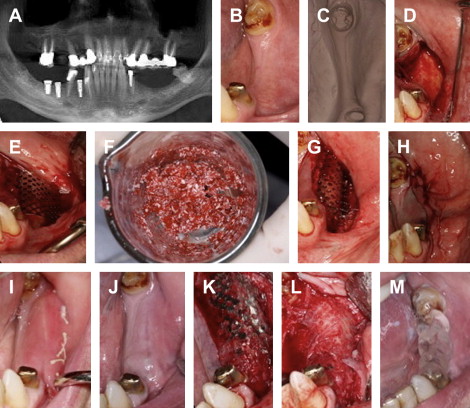
When a small amount of bone is needed, local grafts harvested from the mandibular symphysis or ramus have been used extensively ( Fig. 1 ). These sources have the advantage of being convenient due to their proximity to the reconstruction site and low risk of morbidity. The disadvantage of the mandible as a bone source is the limited amount of bone available and the fact that mandibular harvesting can sometimes interfere with the planned reconstruction if too close to the reconstruction site ( Table 1 ). The most common postoperative morbidity associated with chin and ramus grafts has been reported as temporary paresthesia. For the chin it ranges from 10% to 50%, and for the ramus, it ranges from 0% to 5%. The zygomaticomaxillary region also can be used as a harvest site. The advantage of this site is that when performing grafts in the maxilla, simple extension of the incision is needed. The procedure is associated with a low risk of morbidity. The disadvantage is the limited amount of bone available. Other sites that can be used are the maxillary tuberosity and tori.
| Donor Site | Noncompressed Corticocancellous (mL) | Block (cm) | References |
|---|---|---|---|
| Symphysis | 4.71 | 2.09 × 0.99 × 0.69 | Montazem et al, 2000 |
| Ascending Ramus | 2.36 | 3.76 × 3.32 × 2.25 × 0.92 | Gungormus et al, 2002 |
| Lateral Ramus | NA (not available) | 1.3 × 3 | Li and Schwartz, 1996 |
| Cornoid Process | NA | 1.8 × 1.7 × 0.5 | Choung and Kim, 2001 |
| Zygomatic Butress | NA | 1.5 × 2 | Gellrich et al, 2007 |
| Tiba | 20–40 | 1 × 2 | Caytone et al, 1992 |
| Anterior Ilium | 50 | 1 × 3 | Marx and Morales, 1988 |
| Posterior Ilium | 100–125 | 5 × 5 | Marx and Morales, 1988 |
| Calvarium | NA | NA | Moreira-Gonzalez et al, 2006 |
Distant site bone harvesting is indicated when a large graft is needed (see Table 1 ). Sites that have been reported as reliable include the calvarium and the ilium ( Fig. 2 ). The tibia can be used for harvesting cancellous bone; however, a small amount of block cortical bone also can be harvested. When cancellous bone is needed, the tibia is chosen, because it yields an abundant amount with a relatively low risk of morbidity.
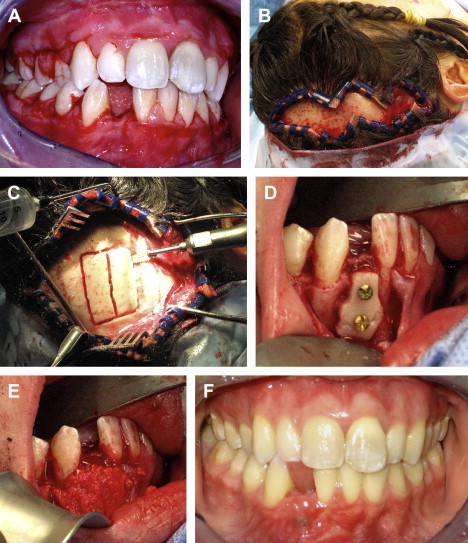

The types of grafts harvested from the calvarium and the ilium are entirely different. Calvarial grafts are usually harvested in strips from the parietal bone. The average thickness of the parietal bone is 7.45 mm. A split thickness harvest technique is used, which can yield graft thicknesses of approximately 3 mm. The main advantage of calvarial grafts is their dense cortical structure that resists resorption. The amount of available cortical graft is abundant. However, this procedure usually requires general anesthesia in a hospital or ambulatory care setting, but there are a few reports of office based techniques. The incidence of complication is low, with the most common reported complication being seroma/hematoma. Larger amounts of bone can be harvested from the ilium, but these grafts typically have a thin cortical layer and a thick cancellous portion. The main advantages of these grafts are the large volume of bone that can be harvested and carved into various shapes. The main disadvantage is the morbidity associated with bone graft harvest. The reported complication incidence is higher than with other donor sites. Reported complications include gait disturbance, paresthesia, hematoma/seroma, and fracture.
Horizontal Segmental Defects
These cases have adequate alveolar bone height but inadequate width. The deficiency is most commonly on the facial surface of the mandible. The planning of these cases should include physical and radiographic examination. The site and the planned implant diameter dictate the amount of bone required. In the mandibular incisor, region a 3 mm diameter implant is usually indicated. The amount of bone needed is 1 mm to 1.5 mm of bone on both the facial and lingual aspect of the implant. Thus, in the incisor region, the minimum amount of bone needed is 4 mm to 5 mm. In the canine and premolar region, the usual implant diameter is approximately 4 mm, and the width of bone needed is 6 mm to 7 mm. In the molar region, the approximate size of the implant needed is usually 5 mm, and the minimum width required is 7 mm to 8 mm. When grafting these various sites, the thickness of the block graft should be slightly larger than the final planned width.
For most segmental deficiencies in the mandible, autogenous grafts can be harvested from the symphysis or ramus. The planned recipient site is usually exposed through a crestal incision. Depending on location of the deficiency, the donor site may be accessed through extension of this incision. Once the site is exposed, the defect can be measured and the size of the bone graft determined.
Many surgeons choose to use a piezoelectric drill because of its versatility. Both the donor site and the recipient site require preparation. The graft, once harvested, is tried into position to determine where trimming is needed. The facial surface of the recipient site is usually flattened, as is the surface of the graft that will be in contact with the recipient site. This allows for more intimate contact between the two surfaces and better incorporation of the graft. Once the desired shape is achieved, the graft is set into position, and depending on the size of the graft, secured into position with 1–2 resorbable or titanium screws. Gaps between the bone graft and the recipient site are filled with particulate bone and covered with a resorbable or nonresorbable membrane. Primary closure is achieved, and the graft is allowed to heal for 3 to 4 months before implant placement.
With larger segments of deficient bone, multiple local sites can be harvested or a distant site can be chosen. The calvarium or ilium can be used but should be chosen based on the application needed. In the case of horizontal deficiency, that is 3 mm or less, the calvarium would be a good choice. When more horizontal augmentation is needed, the ilium could be used or particulate graft added along the buccal or facial aspect of the graft. The block graft is secured with screws, and the entire graft is covered with a membrane. Primary closure is achieved with 4(0) Vicryl (Ethicon Incorporated, Somerville, NJ, USA) or Monocryl (Ethicon Incorporated, Somerville, NJ, USA).
Horizontal Deficiency of the Mandibular Arch
The edentulous horizontally deficient mandible can be treated with multiple local grafts or bone from distant sites. Because of the large amount of bone needed, harvest from a distant site is usually indicated. Exposure is usually performed through a vestibular incision. The mental nerves are identified and protected. Once the alveolus is encountered, the incision is carried through the periosteum, and the ridge is exposed. The grafts are mortised into position by preparing both the recipient site and bone graft. Once a good fit is ensured, the graft is secured into position with screws. The graft is protected with a membrane, and the wound is closed primarily.
Vertical Segmental Defects
Vertical augmentation of the alveolar ridge is more difficult than horizontal augmentation. There is concern when expanding the soft tissue envelope vertically there is an increased risk of graft exposure. A second concern is the adequate adaptation of the bone graft, which is critical for graft success.
Many of these alveolar ridges are deficient in height and width and may require flattening for better graft adaptation. If thin cortical grafts are harvested, then a stack technique is used to achieve the desired result. This technique involves the mortising of the graft to the ridge surface and the placement of multiple block grafts stacked on one another to achieve height. The graft is secured with a bone screw or by dental implants. A second technique is to augment the defect with a single corticocancellous block that adequately replaces the desired amount of bone.
Segmental defects are usually exposed through a crestal incision. Once good bone adaptation is achieved between the graft and recipient site, the graft is secured with titanium screws. Any gaps between the recipient site and the bone graft are filled with particulate bone graft and covered with a membrane. To achieve closure of the wound, the periosteum of the flap is released. This is achieved by placing a horizontal incision just through the periosteum under the flap. This allows the flap to stretch and permits primary closure without wound tension.
Vertical Deficiency of the Mandibular Arch
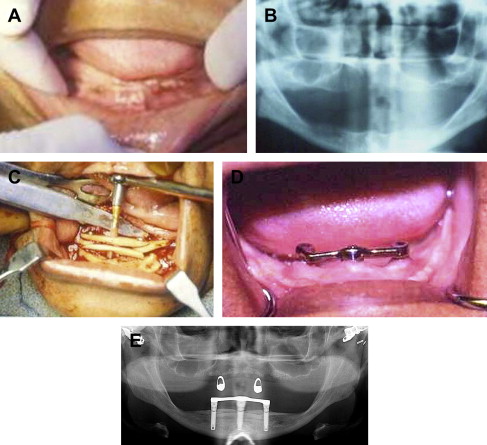
This generally requires a large amount of autogenous bone from the calvarium or the ilium. As discussed earlier, reconstruction can be performed using a stacked calvarial graft that is shaped and mortised to the desired height ( Fig. 3 ). Iliac crest grafts do not require stacking; instead the ridge is exposed through a vestibular incision, the mental nerves identified, the block secured with titanium screws, and gaps filled with cancellous particulate, then covered with a membrane before performing a 2-layer closure.
Allogeneic Block Grafts
Allogeneic block grafts have not had extensive use in implant dentistry. A systemic review of the literature by Waasdorp identified 35 papers, with only nine publications meeting inclusion criteria (2 case reports, 6 case series, and 1 prospective, multicenter, consecutive case series). There were no randomized controlled clinical trials identified. Observational studies generally report graft incorporation rates of 90% or greater and implant survival of 99% to 100%. The shortcomings of these studies is that most reports involved selected defects in anterior regions and had short term follow-ups of less than 3 years. The reviewers concluded that case-based reports document the potential for allogeneic block grafts to support alveolar ridge augmentation and implant placement, but there is insufficient evidence to establish treatment efficacy relative to graft incorporation, alveolar ridge augmentation, and long-term dental implant survival.
Allogeneic block grafts can be substituted for autogenous grafts to avoid donor site morbidity, but the risk of exposure is higher, especially with vertical augmentation.
Barrier membranes
Barrier membranes have been studied extensively in the dental and maxillofacial literature. Membranes have been shown to protect both block and particulate onlay grafts. The surgeon has the choice of resorbable versus nonresorbable and rigid versus nonrigid membranes when performing grafting procedures. Studies suggest that there is less resorption of block and particulate grafts when a membrane remains in place throughout the healing phase of the graft. Significant resorption can occur for block grafts left unprotected, but not always. Vertical augmentation is particularly problematic with both block and particulate grafts, with resorption rates that have been reported higher than for horizontal augmentation. Cordaro reported resorption rates of 23.5% for lateral augmentation and 42% for vertical augmentation when using block grafts without a membrane. Particulate onlay grafts can undergo even more resorption.
Block grafts have structural integrity and thus maintain space and resist resorption. Particulate grafts lack structural integrity and can be displaced. With horizontal augmentation, where the vertical height is adequate and only width is lacking, particulate graft material can be used and protected with a membrane. The choice of particulate graft material becomes important if a nonrigid membrane is used. The particulate graft must have some strength to resist deformation by the soft tissue envelope. In this case, it is preferable to use a mineralized bone product such as autogenous bone, mineralized allogeneic bone, or anorganic bovine bone. If a rigid membrane is used, then the choice of material becomes less crucial, as a rigid membrane will maintain space and protect the graft.
When vertical augmentation is indicated, block or particulate graft can be chosen. If a block graft is chosen, it has the advantage of structural integrity to maintain space; however, because of high resorption potential, membrane protection is warranted. A nonrigid, resorbable or nonresorbable membrane can be used.
When a particulate graft is selected for vertical augmentation, a rigid membrane must be used to protect the graft. The technique of vertical augmentation with particulate grafts protected by a rigid membrane has been reported to be successful. These techniques have been associated with a high rate of exposure that can negatively affect the graft. Exposure rates are as high as 50%, particularly when large vertical augmentations are performed. One of the techniques that has been described to minimize graft exposure is the use of PRP (platelet-rich plasma gel) placed over the rigid membrane before wound closure.
Barrier membranes
Barrier membranes have been studied extensively in the dental and maxillofacial literature. Membranes have been shown to protect both block and particulate onlay grafts. The surgeon has the choice of resorbable versus nonresorbable and rigid versus nonrigid membranes when performing grafting procedures. Studies suggest that there is less resorption of block and particulate grafts when a membrane remains in place throughout the healing phase of the graft. Significant resorption can occur for block grafts left unprotected, but not always. Vertical augmentation is particularly problematic with both block and particulate grafts, with resorption rates that have been reported higher than for horizontal augmentation. Cordaro reported resorption rates of 23.5% for lateral augmentation and 42% for vertical augmentation when using block grafts without a membrane. Particulate onlay grafts can undergo even more resorption.
Block grafts have structural integrity and thus maintain space and resist resorption. Particulate grafts lack structural integrity and can be displaced. With horizontal augmentation, where the vertical height is adequate and only width is lacking, particulate graft material can be used and protected with a membrane. The choice of particulate graft material becomes important if a nonrigid membrane is used. The particulate graft must have some strength to resist deformation by the soft tissue envelope. In this case, it is preferable to use a mineralized bone product such as autogenous bone, mineralized allogeneic bone, or anorganic bovine bone. If a rigid membrane is used, then the choice of material becomes less crucial, as a rigid membrane will maintain space and protect the graft.
When vertical augmentation is indicated, block or particulate graft can be chosen. If a block graft is chosen, it has the advantage of structural integrity to maintain space; however, because of high resorption potential, membrane protection is warranted. A nonrigid, resorbable or nonresorbable membrane can be used.
When a particulate graft is selected for vertical augmentation, a rigid membrane must be used to protect the graft. The technique of vertical augmentation with particulate grafts protected by a rigid membrane has been reported to be successful. These techniques have been associated with a high rate of exposure that can negatively affect the graft. Exposure rates are as high as 50%, particularly when large vertical augmentations are performed. One of the techniques that has been described to minimize graft exposure is the use of PRP (platelet-rich plasma gel) placed over the rigid membrane before wound closure.
Particulate grafts
Particulate onlay grafts have been used extensively for reconstruction of mandibular alveolar defects. Autogenous and nonautogenous options are available. The source of autogenous particulate is the same as has been discussed for block harvest (see Table 1 ). For small amounts of bone, local sites can be used, including the symphysis, ramus, and maxillary tuberosity. This is usually harvested with a bone shaver. When greater volumes of bone are needed, then distant sites are employed. Particulate grafts have the advantage of rapid vascularization, but they must be protected by a membrane to reduce the risk of resorption.
Allogeneic and xenogenic particulate grafts have been growing in popularity. These grafts are readily available and abundant. They can be used in combination with autogenous bone or alone. Recent studies have shown success with these graft materials for vertical ridge augmentation when protected with a rigid membrane.
Segmental Horizontal Defects
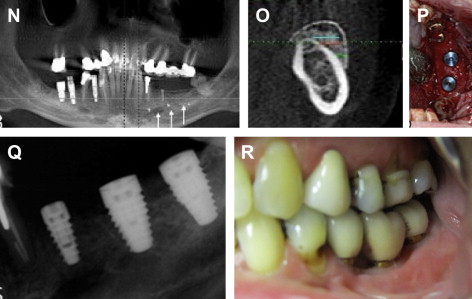
The reconstruction of the partially edentulous mandible with particulate graft material can be performed with various bone graft materials. The type of graft material needed will depend on the size of the defect and type of membrane used. With horizontal augmentation, where the vertical height is adequate, and only width is lacking, particulate graft material can be used and protected with a membrane ( Fig. 4 ). When a mineralized bone graft is used, a nonrigid membrane is suggested. In this technique, the graft is placed through a crestal incision. The defect is grafted, then protected with membrane. If a rigid membrane is used, it must be fixed with screws. If a nonrigid membrane is used, the edges of the membrane must be tucked and secured underneath the flap.
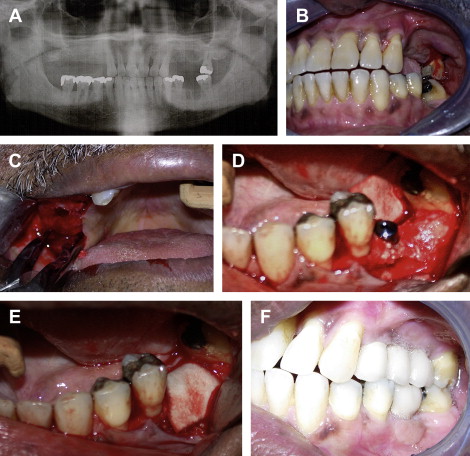
Demineralized bone graft materials tend to be soft and easily compressed by the soft tissue envelope. If only demineralized product is used to augment a horizontal defect, a rigid membrane should be used to protect the graft. This membrane must be secured with screws to the underlying bone to prevent micromotion. To close the wound, a periosteal releasing incision may be required. The particulate graft must have some strength to resist deformation. In this case, it is preferable to use mineralized product such as autogenous bone, mineralized allogeneic bone, or anorganic bovine bone as the graft of choice. However, if a rigid membrane is used, then the choice of material becomes less crucial.
The technique is done through a vestibular incision to expose the edentulous space. The incision is extended to near the junction of the attached mucosa. Mobilization of the facial, crestal, and lingual aspect of the soft tissues is usually performed. The dissection around the cervical portion of the teeth is performed in a tunneling fashion subperiosteally to mobilize the gingival cuff. As an alternative to a vestibular incision, a crestal incision can be used in conjunction with releasing incision at least 2 teeth on either side of the defect. Once the ridge is exposed, a titanium mesh membrane can be trimmed and contoured to fit into position as a crib. This is then filled with bone graft and secured with at least 2 screws on the facial aspect. When a crestal incision is used for exposure, the periosteum must be released along the facial vestibule to facilitate a tension-free closure of the wound. This is usually not necessary when a vestibular incision is used. Closure is performed in layers with 3.0 Vicyrl suture material placed deep to the mucosa. The mucosa is closed with 4.0 Vicyrl or Monocryl suture.
Segmental Vertical Defects
When using a particulate bone graft for vertical ridge augmentation, a rigid membrane must be used to prevent deformation and resorption of the graft. The reconstruction is performed in similar fashion as described in the section Segmental Horizontal Defects ( Fig. 5 ).
Horizontal Deficiency of the Mandibular Arch
To reconstruct horizontal deficiency of the mandibular alveolus with particulate graft, the principles of graft protection during the healing phase are important. The ridge is exposed through a vestibular incision. After identification of the mental nerves, the dissection is carried toward the ridge. The periosteum is incised, and a subperiosteal dissection is performed to expose the ridge. The particulate graft is placed and then covered with a membrane. The choice of particulate graft material becomes important if a nonrigid membrane is used. The particulate graft must have some strength to resist deformation. In this case, it is preferable to use mineralized bone as the graft of choice. If a rigid membrane is used, the choice of material becomes less crucial, as a rigid membrane will maintain space and protect the graft. Following membrane placement, the wound is closed primarily.
Vertical Deficiency of the Mandibular Arch
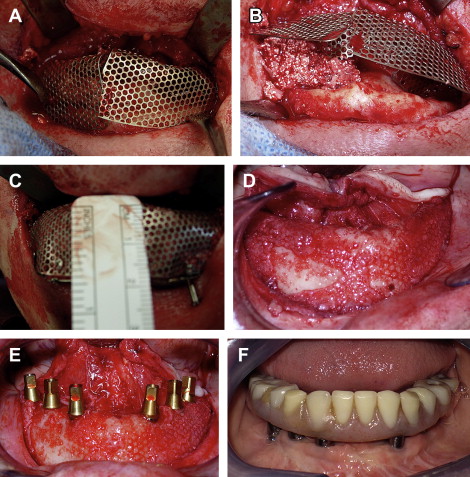
When augmenting the highly atrophic edentulous mandible vertically, an intraoral or extraoral approach can be used. The intraoral approach is more straightforward. In this technique, an incision is made in the depth of the mandibular vestibule just anterior to the retromolar pad extending anteriorly across the midline. After identifying and protecting the mental nerves, a subperiosteal dissection is achieved. In the extremely atrophic mandible, the inferior alveolar nerve may be exposed along the crest due to dehiscence of the canal. In this case, a preferred technique is to start anteriorly and identify the mental foramina and then dissect posteriorly. With this technique, the dissection is carried onto the lingual surface of the mandible in a subperiosteal fashion. The lingual extent of the dissection anteriorly is to the genial tubercles. The genioglossus and geniohyoid should not be detached.
Once the mandible is exposed, the preferred technique for vertical augmentation is the use of preformed titanium mesh. A right hemi-tray and left hemi-tray are chosen based on the desired level of augmentation. This is determined by preoperative planning with study models and radiographs. The mesh is contoured and trimmed to fit. Relief over the mental foramina is necessary to avoid injury to the nerve. It is desirable to extend the mesh to the posterior aspect of the mandible in the region of the retromolar pad, as the crest of the ridge begins to turn superiorly to form the ramus. This is done to avoid any sharp areas at the end of the mesh that may later become exposed. In patients with larger mandibles, two trays may not be long enough to extend posteriorly to the retromolar region while still covering the anterior aspect of the mandible. In these cases, a third piece of titanium mesh must be contoured and overlapped onto the anterior aspects of both hemi-trays in order to protect the graft that will be placed in this location.
The mesh is filled with the bone graft and secured into position with at least 2 screws on the facial surface of each hemi-tray and 1 screw on the lingual, usually in the anterior region just above the genial tubercles. If an additional midline mesh is needed to cover the graft, it can be secured on the facial and lingual of the ridge. PRP gel can be placed over the mesh before closure of the incision to minimize exposure. Because the incision is made in the vestibule, the soft tissue is thick and should be closed in two layers.
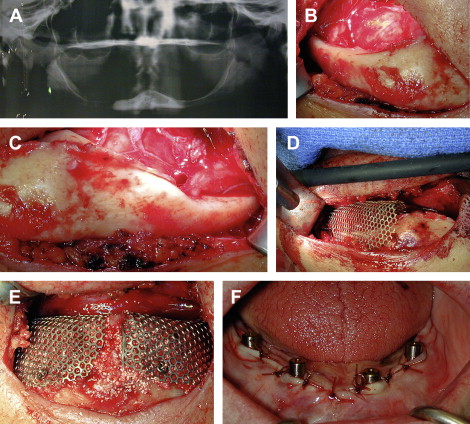
An extraoral approach also can be used when augmenting the mandible ( Figs. 6 and 7 ). This approach is more difficult than an intraoral approach because it involves transposition of the inferior alveolar nerves. This incision is made under sterile conditions along the submental crease. The incision must be extended along the full length of the submental crease in order to achieve adequate exposure. This dissection is carried sharply down to the inferior border of the mandible where a subperiosteal dissection is performed to expose the facial and superior aspect of the mandible. From this approach, the mental nerves can be easily identified. When there is a dehiscence of the inferior alveolar nerve, the neurovascular bundle is mobilized and transposed posteriorly. In cases where there is no dehiscence, the inferior alveolar nerve transposition is performed in order to achieve adequate mobilization of the mental nerve and provide room for the bone graft and titanium mesh trays. Once the inferior alveolar nerve is transposed, usually to the second molar region, the titanium mesh tray can be contoured and trimmed.

Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


