Introduction
The purpose of this study was to evaluate the effect of bone densities on the success rate of orthodontic microimplants with cone-beam computed tomography images.
Methods
We examined 127 orthodontic microimplants implanted into the maxillary buccal alveolar bone of 71 patients (53 female, 18 male; mean age, 19.2 years) with malocclusion. The cortical, cancellous, and total bone densities were measured with Simplant Pro 2011 software (version 13; Materialise, Leuven, Belgium), and the correlations between these measurements and the orthodontic microimplant success rates were evaluated with cone-beam computed tomography.
Results
The overall success rate was 85.0% (108 of 127). Sex, age, and side of placement were not significant factors for success in the results ( P >0.05). The density of the cortical bone increased apically (3, 5, and 7 mm) from the alveolar crest, but in the cancellous bone it decreased. Whereas the orthodontic microimplant success rates significantly increased as cancellous bone density and total bone density increased ( P <0.01), cortical bone density did not have a significant effect on the success rate ( P >0.05).
Conclusions
The success rate of orthodontic microimplants significantly increased with higher cancellous and total bone densities, whereas cortical bone density did not have a significant effect.
Highlights
- •
Cortical and cancellous bone densities were measured with cone-beam computed tomography.
- •
Correlations were made between bone densities and orthodontic microimplant success rates.
- •
Cortical bone density did not have a significant effect on the success rate of microimplants.
- •
Cancellous bone density was significantly related to the success rate of microimplants.
Adequate anchorage control is essential for the treatment of skeletal and dental malocclusions. To achieve this, clinicians have started to use intraosseous anchorage, which does not require patient compliance and shows no loss of anchorage. Orthodontic microimplants (OMIs) are favored in practice because of their many advantages; they are simple and economical and have few anatomic limitations in placement sites. As the usage of OMIs in orthodontic treatment is increasing, much attention has been focused on their success rates and the factors affecting outcomes.
Many studies have reported success rates with OMIs from 70% to 100%. Radiographic examination has been commonly used to study the factors affecting the success rate: root proximity, insertion height, cortical bone thickness, placement angle, and bone density are the keys to the success of OMIs.
Recently, with the development of cone-beam computed tomography (CBCT), 3-dimensional bone density measurements have become possible. Although the use of CBCT is increasing in the dental field because of its low radiation dose compared with multidetector computed tomography and its cost, there have been some doubts about its accuracy for bone density measurement.
Silva et al reported that bone density in Hounsfield units (HU) from CBCT images had low reliability because the average Hounsfield unit value was higher with CBCT than with multidetector computed tomography. Campos et al also reported that CBCT should not be considered as the examination of choice for the determination of mineral density of osseous and soft tissues, especially when the values obtained are compared with predetermined standard values. However, Mah et al reported that Hounsfield units could be derived from the gray levels in dental CBCT scanners using linear attenuation coefficients as an intermediate step, and that the results were as accurate as those with medical computed tomography (CT) Hounsfield units.
There have been many studies on bone density affecting the success rates of OMIs, but most were animal experiments with multidetector computed tomography, evaluating only the cortical bone or measuring the primary stability of OMIs, not the success rates. Studies on the success rates and bone densities in CBCT images from patients with OMIs are rare. Therefore, the aim of this study was to evaluate the effect of cortical, cancellous, and total bone densities on the success rate of OMIs using CBCT images.
Material and methods
A power analysis using G*Power (version 3.19.2; Franz Faul, Christian-Albrechts-Universitat, Kiel, Germany) was performed to estimate the sample size needed for this study. It was calculated based on a significance level of 0.05 and a power of 85%. The power analysis showed that 121 subjects were required. Institutional review board approval was granted by Wonkwang University Dental Hospital (number WKD IRB W1403/002-001) in Daejeon, Korea, to conduct this study.
Patients who received OMIs in the maxillary buccal alveolar bone for orthodontic anchorage at the Department of Orthodontics of Wonkwang University Daejeon Hospital from January 2007 to December 2013 and who had had initial CBCT images taken in C-mode were selected. Before implantation, the patients were informed of the advantages and disadvantages of this procedure, and informed consents were obtained from all of them.
A total of 127 OMIs (diameter, 1.2-1.3 mm; length, 8 mm; implant type, AbsoAnchor SH1312-08 [self-drilling and tapered]; Dentos, Daegu, Korea]) were placed in 71 orthodontic patients (53 female, 18 male; mean age, 19.2 years; SD, 6.63 years) who were observed. All OMIs were placed directly by self-drilling with a hand driver under local anesthesia by 3 right-handed operators (M-Y.L., N-Y.C., J-M.C.). OMIs were implanted into the maxillary buccal alveolar bone between the second premolar and the first molar or the first molar and the second molar on the attached gingiva near the mucogingival junction, with immediate loading of 50 to 200 g.
It was considered to be a success when the OMIs were retained in the alveolar bone as an appropriate anchor for at least 1 year during the orthodontic treatment. Success rates based on age, sex, and placement sites (right or left) were calculated. To assess the effect of age on the success rate, the patients were divided into 2 age groups : young patients (<20 years) with 73 orthodontic microimplants, and adults (≥20 years) with 54 orthodontic microimplants ( Table I ).
| Success rate (%) | Success/total orthodontic implants (n) | Significance (chi-square test) | |
|---|---|---|---|
| Sex | 0.483 (1.000) | ||
| Male | 87.1 | 27/31 | |
| Female | 84.4 | 81/96 | |
| Age (y) | 0.410 (0.801) | ||
| <20 | 83.6 | 61/73 | |
| ≥20 | 87.0 | 47/54 | |
| Side of placement | 0.134 (0.217) | ||
| Right | 80.6 | 50/62 | |
| Left | 89.2 | 58/65 | |
| Total | 85.0 | 108/127 |
CBCT (PSR 9000N; Asahi Alphard Vega, Kyoto, Japan) images were taken in C-mode (scan size, 200 × 179 mm; voxel size, 0.39 mm; field of view, 19.97 cm). The radiologic parameters used were 80 kVp, 60 mAs, and 17-second scan time.
The CBCT data were saved in digital imaging and communications in medicine (DICOM) files, and Simplant Pro 2011 pack software (version 13; Materialise, Leuven, Belgium) was used to analyze the DICOM data to reorient the reference planes and generate the quantitative measurements.
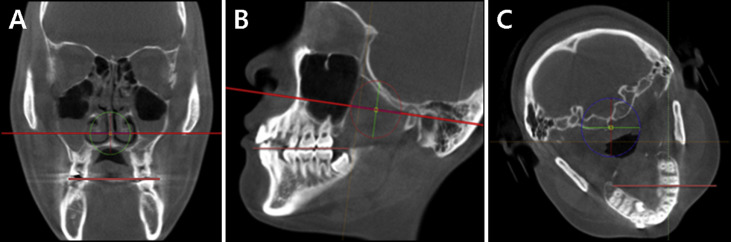
For the measurements, the transverse occlusal plane of the posterior teeth was aligned to the axial plane on the coronal view, and the horizontal occlusal plane of the posterior teeth going through the cusps of the first premolar and second molar was aligned to the axial plane on the sagittal view. Then the interradicular space between the second premolar and the first molar or the first molar and the second molar was aligned to the horizontal plane on the axial view ( Fig 1 ).
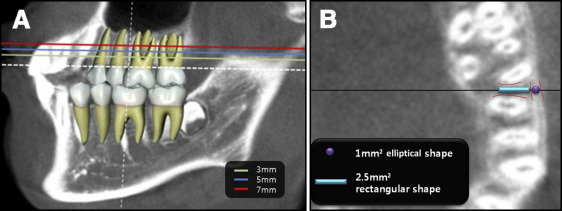
After the image was reoriented with the Simplant software in this way, the axial planes 3, 5, and 7 mm above the alveolar crest of the sagittal view were obtained. Because we used 8-mm-long OMIs and because the mean height of the OMIs was 6.3 mm (SD, 1.01 mm) apically from the alveolar crest, the bone density was measured at points up to 7 mm above the alveolar crest. Cortical and cancellous bone densities were determined on the axial view by measuring them in Hounsfield units at the line dividing the interradicular space in half by making a 2.5-mm 2 rectangular shape in the cancellous bone and a 1.0-mm 2 elliptical shape in the cortical bone using the software program ( Fig 2 ). The total bone density was determined by combining cortical bone and cancellous bone densities.
Statistical analysis
To test the reliability of the measurements, 1 investigator (M-Y. L.) randomly reevaluated 30 subjects 3 weeks after the initial measurement: this showed no statistically significant difference ( P >0.05) in the intraclass correlation coefficient, which showed great test-retest reliability of bone density at a 95% confidence interval.
SPSS software (version 22.0; IBM, Armonk, NY) was used for all statistical calculations. Logistic regression analysis was carried out to evaluate the correlations between measurements of bone density and success rates. The Wald test was also used to test the true value of the measurements on the success rates. The Pearson correlation coefficient of cortical, cancellous, and total bone densities was carried out. Significance at P <0.05 was established.
Results
The overall success rate was 85.0% (108 of 127 OMIs). It tended to be higher on the left sides than on the right sides in adults and in male subjects, although these differences were not statistically significant ( Table I ).
Table II and Figure 3 show the mean bone density patterns apically (3, 5, and 7 mm) from the alveolar crest. Whereas cortical bone density tended to increase apically from the alveolar crest, cancellous bone density showed the highest value at the 3-mm height from the alveolar crest and gradually decreased apically from the alveolar crest. The total bone density increased from the alveolar crest to the 5-mm height of the alveolar bone and then slightly decreased.
| Bone density | Alveolar bone height (mm) | Mean (HU ∗ ) | SD (HU ∗ ) |
|---|---|---|---|
| Cortical bone | 3 | 922.82 | 198.6 |
| 5 | 963.11 | 198.4 | |
| 7 | 968.17 | 214.7 | |
| Mean | 950.79 | 191.1 | |
| Cancellous bone | 3 | 578.39 | 174.2 |
| 5 | 561.56 | 165.7 | |
| 7 | 555.05 | 173.5 | |
| Mean | 564.69 | 159.5 | |
| Total bone | 3 | 750.61 | 186.4 |
| 5 | 762.34 | 182.1 | |
| 7 | 761.61 | 194.1 | |
| Mean | 757.74 | 175.3 |
∗ Hounsfield units, a linear transformation of the original linear attenuation coefficient measurement into one in which the radiodensity of distilled water at standard pressure and temperature is defined as 0 HU, and the radiodensity of air at standard pressure and temperature is defined as –1000 HU.
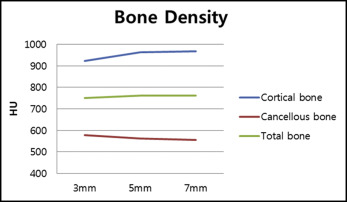
Table III shows bone density according to sex, age, and side of placement. As Table II shows, the patterns of bone density are similar. Cortical bone density is higher in female subjects, adults, and the right side. Cortical bone density increased as bone height increased from the alveolar crest except on the left side at the 7-mm height. Cancellous bone density was higher in female patients, young patients, and the right side than in male patients, adults, and the left side, except at the 7-mm height. Cancellous bone density decreased as bone height increased from the alveolar crest except in adult patients at the 7-mm height. Total bone density was higher in female subjects, adults, and the right side than in male subjects, young patients, and the left side except at the 3-mm height. However, there were no significant differences except for cortical bone densities between male and female patients at the heights of 5 and 7 mm.
| Alveolar bone height/n | Sex | Age (y) | Side of placement | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Male | Female | Sig | <20 | ≥20 | Sig | Right | Left | Sig | |
| 31 | 96 | 73 | 54 | 62 | 65 | ||||
| Cortical bone | |||||||||
| 3 mm | 906.96 ± 169.0 | 925.65 ± 207.9 | 0.203 | 914.55 ± 205.8 | 925.93 ± 193.6 | 0.465 | 995.77 ± 194.9 | 849.86 ± 175.8 | 0.200 |
| 5 mm | 918.55 ± 140.8 | 977.49 ± 212.3 | 0.009 ∗ | 952.12 ± 214.9 | 975.51 ± 178.7 | 0.077 | 1049.20 ± 187.3 | 880.98 ± 173.3 | 0.304 |
| 7 mm | 921.38 ± 158.5 | 983.28 ± 228.6 | 0.033 ∗ | 947.67 ± 231.7 | 994.05 ± 192.6 | 0.187 | 1060.33 ± 207.9 | 880.27 ± 182.9 | 0.155 |
| Mean | 915.63 ± 146.7 | 962.14 ± 202.7 | 0.073 | 938.11 ± 206.2 | 965.16 ± 172.7 | 0.094 | 1035.10 ± 179.3 | 870.37 ± 166.8 | 0.369 |
| Cancellous bone | |||||||||
| 3mm | 548.52 ± 170.4 | 587.93 ± 175.2 | 0.609 | 586.81 ± 162.3 | 552.47 ± 184.3 | 0.291 | 581.76 ± 165.3 | 575.02 ± 183.5 | 0.238 |
| 5 mm | 536.80 ± 163.5 | 569.06 ± 166.4 | 0.966 | 560.55 ± 156.6 | 548.84 ± 173.4 | 0.221 | 577.42 ± 167.5 | 545.69 ± 163.7 | 0.750 |
| 7 mm | 510.30 ± 165.2 | 568.86 ± 174.5 | 0.919 | 543.04 ± 163.7 | 559.26 ± 183.7 | 0.165 | 575.48 ± 175.9 | 534.62 ± 170.1 | 0.727 |
| Mean | 531.87 ± 155.9 | 575.28 ± 160.1 | 0.887 | 563.47 ± 149.9 | 553.52 ± 167.9 | 0.189 | 578.22 ± 157.4 | 551.78 ± 161.8 | 0.484 |
| Total bone | |||||||||
| 3 mm | 727.84 ± 141.9 | 756.79 ± 164.6 | 0.406 | 750.68 ± 154.9 | 739.19 ± 166.2 | 0.754 | 788.76 ± 159.7 | 712.44 ± 150.8 | 1.1052 |
| 5 mm | 727.68 ± 133.5 | 773.28 ± 164.0 | 0.270 | 756.34 ± 157.9 | 762.18 ± 159.8 | 0.405 | 813.32 ± 156.7 | 713.34 ± 143.8 | 0.089 |
| 7 mm | 715.84 ± 140.2 | 776.07 ± 168.7 | 0.126 | 745.36 ± 164.4 | 776.66 ± 164.5 | 0.669 | 817.91 ± 161.6 | 707.45 ± 147.8 | 0.240 |
| Mean | 723.75 ± 131.9 | 768.71 ± 157.4 | 0.318 | 750.79 ± 152.3 | 759.34 ± 153.9 | 0.620 | 806.67 ± 149.7 | 711.07 ± 140.6 | 0.156 |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


