Bimaxillary protrusion in a 28-year-old woman was complicated by multiple missing, restoratively compromised, or hopeless teeth. The maxillary right central incisor had a history of avulsion and replantation that subsequently evolved into generalized external root resorption with Class III mobility and severe loss of the supporting periodontium. This complex malocclusion had a discrepancy index of 21, and 8 additional points were scored for the atrophic dental implant site (maxillary right central incisor). The comprehensive treatment plan included extraction of 4 teeth (both maxillary first premolars, the maxillary right central incisor, and the mandibular right first molar), orthodontic closure of all spaces except for the future implant site (maxillary right central incisor), augmentation of the alveolar defect with an autogenous chin-block graft, enhancement of the gingival biotype with a connective tissue graft, and an implant-supported prosthesis. Orthodontists must understand the limitations of bone grafts. Augmented alveolar defects are slow to completely turn over to living bone, so they are usually good sites for implants but respond poorly to orthodontic space closure. However, postsurgical orthodontic treatment is often indicated to optimally finish the esthetic zone before placing the final prosthesis. The latter was effectively performed for this patient, resulting in a total treatment time of about 36 months for comprehensive interdisciplinary care. An excellent functional and esthetic result was achieved.
Highlights
- •
Augmented alveolar defects are good sites for implants.
- •
Space closure of the grafted defect is contraindicated.
- •
Activated pericytes can be stimulated to differentiate into osteoblasts.
- •
A thick block of autogenous cortical bone resorbs slowly.
- •
It can support an implant and is more stable initially than vital alveolar bone.
Orthodontists require a broad interactive knowledge of interdisciplinary care to manage partially edentulous malocclusions and may be the appropriate clinicians to head the interdisciplinary team. Failing teeth and alveolar defects in the maxillary esthetic zone are particularly challenging diagnostic problems. One of the more perplexing challenges is the subsequent orthodontic treatment of teeth with a history of trauma. These teeth may fail before, during, or after orthodontic treatment. A history of incisor avulsion and replantation is often associated with a compromised long-term prognosis. The consequences of tooth avulsion are directly related to the severity of the injury, the surface area of the inflamed root surface, the damaged root surface that must be repaired, and the treatment rendered at the time of injury. Donaldson and Kinirons found that periodontal ligament “dry time” is the most crucial clinical factor associated with the development of subsequent root resorption. If the periodontal ligament is left attached to the root surface and does not dry out for longer than 15 minutes, the probability of severe root resorption is minimal. Appropriate pulp therapy can also minimize or prevent inflammatory root resorption. Gregg and Boyd and Kinirons et al suggested that a replanted tooth with a closed apex should be endodontically treated as soon as the tooth has achieved adequate stability, ideally within 10 days after the trauma. When pulp extirpation is delayed for more than 20 days, the incidence of inflammatory resorption increases. For a tooth with a wide-open apex, endodontic treatment may be delayed because revascularization of the pulp is possible, but the patient should be carefully followed for inflammatory resorption.
Despite advances in managing traumatically avulsed teeth, severe cervical and root resorption is common, with a reported prevalence of 57% to 80%. Extensive resorption can compromise not only the tooth but also its supporting periodontium. This case report presents a 28-year-old woman with a chief complaint of poor esthetics and function, related to a hopeless (previously avulsed and replanted) maxillary central incisor, missing or compromised mandibular first molars, and bimaxillary protrusion ( Fig 1 ). Prescribing and performing appropriate interdisciplinary treatment required the orthodontist (C.H.N.C.) to have a thorough knowledge of all aspects of the necessary interdisciplinary care, as well as the relevant basic science. Because of the dynamic nature of the interactive treatment required, the orthodontist led the interdisciplinary team.

Diagnosis and etiology
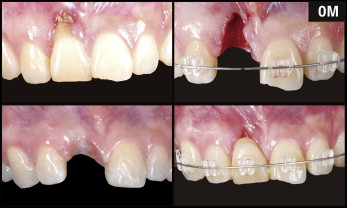
A 28-year-old woman sought consultation for a mutilated bimaxillary protrusion complicated by a failing maxillary right central incisor with a severe labial cleft and Class III mobility ( Fig 2 ). There was an etiology of trauma at about 9 years of age, when the tooth was avulsed and replanted. This is a common but highly variable problem affecting up to 16% of children. The patient reported that the replanted tooth healed uneventfully, but there was no follow-up pulp evaluation. The tooth remained asymptomatic until mobility was first noted about 5 years previously (age 23 years). Mobility and soft tissue recession had progressively increased since that time.
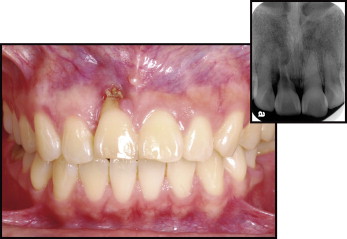
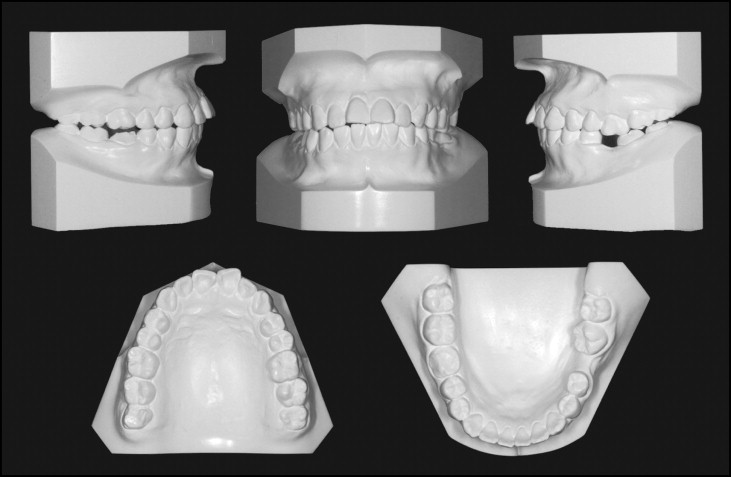
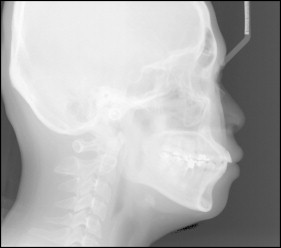
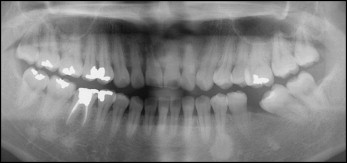
Clinical and radiographic evaluation of the maxillary right central incisor showed extensive external root resorption (>80% of the root surface), an enlarged pulp chamber, and severe loss of periodontal support ( Fig 2 ). In the mandibular arch, the left first molar was missing, the left second molar was mesially tipped, and the right first molar was endodontically treated and was temporarily restored with amalgam ( Fig 1 ). The pretreatment study casts showed that the patient had an excessive overjet of about 4 mm and a space deficiency in the maxillary arch of about 5 mm ( Fig 3 ). The pretreatment cephalometric analysis was consistent with a Class I skeletal pattern, a convex profile, bimaxillary protrusion, and excessive axial inclination of the maxillary and mandibular incisors ( Fig 4 , Table ). The panoramic radiograph showed that all third molars were present and fully erupted ( Fig 5 ). The American Board of Orthodontics (ABO) discrepancy index was 21 points, as shown in the Supplementary Discrepancy Index (Worksheet 1) . The compromised implant site (maxillary right central incisor) scored an additional 8 points for complexity (form in Worksheet 1 ). Overall, this mutilated malocclusion ( Figs 1-3 ) was a severe problem requiring a carefully sequenced, interdisciplinary approach.
| Pretreatment | Posttreatment | Difference | |
|---|---|---|---|
| Skeletal analysis | |||
| SNA (°) | 87 | 87 | 0 |
| SNB (°) | 83 | 83 | 0 |
| ANB (°) | 4 | 4 | 0 |
| SN-MP (°) | 29 | 29 | 0 |
| FMA (°) | 22 | 22 | 0 |
| Dental analysis | |||
| U1-NA (mm) | 10 | 6 | 4 |
| U1-SN (°) | 120 | 113 | 7 |
| L1-NB (mm) | 13 | 9 | 4 |
| L1-MP (°) | 105 | 102 | 3 |
| Facial analysis | |||
| E-line-upper lip (mm) | 5 | 3 | 2 |
| E-line-lower lip (mm) | 5.5 | 4.5 | 1 |
Treatment objectives
The following treatment objectives were determined.
- 1.
Maintain the dimensions of all 3 skeletal planes in both the maxilla and the mandible.
- 2.
Extract both maxillary first premolars, the hopeless maxillary right central incisor, and the compromised mandibular right first molar.
- 3.
Use full fixed orthodontic therapy to relieve crowding, retract the anterior segments to correct the bimaxillary protrusion, and close all spaces except the maxillary right central incisor implant site.
- 4.
Surgically repair the atrophic maxillary right central incisor alveolar defect with an autogenous chin-block graft and correct the thin gingival biotype with connective tissue grafts.
- 5.
Use an implant-supported prosthesis to restore the maxillary right central incisor.
- 6.
Optimize dentofacial esthetics with orthodontic treatment and soft tissue detailing.
Treatment objectives
The following treatment objectives were determined.
- 1.
Maintain the dimensions of all 3 skeletal planes in both the maxilla and the mandible.
- 2.
Extract both maxillary first premolars, the hopeless maxillary right central incisor, and the compromised mandibular right first molar.
- 3.
Use full fixed orthodontic therapy to relieve crowding, retract the anterior segments to correct the bimaxillary protrusion, and close all spaces except the maxillary right central incisor implant site.
- 4.
Surgically repair the atrophic maxillary right central incisor alveolar defect with an autogenous chin-block graft and correct the thin gingival biotype with connective tissue grafts.
- 5.
Use an implant-supported prosthesis to restore the maxillary right central incisor.
- 6.
Optimize dentofacial esthetics with orthodontic treatment and soft tissue detailing.
Treatment alternatives
A common option for correcting bimaxillary protrusion is extraction of all 4 first premolars. However, this patient had missing and compromised mandibular first molars, so the appropriate extraction sequence was maxillary first premolars and mandibular first molars. This approach presented anchorage problems that were manageable with advance planning.
Omitting the bone graft and closing the space for the extracted maxillary right central incisor ( Fig 2 ) may be an attractive orthodontic option, but that approach would create extensive restorative problems to scale the incisors and prevent an end-on occlusion, which would likely result in compromised dental esthetics in the critical maxillary anterior area. A fixed partial denture to replace the maxillary right central incisor was not a viable alternative because it would require preparing adjacent virgin teeth. The patient rejected space closure and a fixed partial denture in favor of augmenting the soft and hard tissue defects and restoring with an implant-supported crown. When selecting this option, the patient was informed that it was a complex treatment plan with many steps that might or might not be completely successful. Also, follow-up orthodontic treatment might be necessary for final detailing. After considering the pros and cons of each option, the patient exercised her informed consent by selecting bone and soft tissue augmentation followed by an implant-supported prosthesis.
Treatment progress
After the maxillary right central incisor, both maxillary premolars, and the mandibular right first molar were extracted, a mixed 0.022-in fixed appliance was bonded on all teeth using ICE clear fixed brackets (Ormco, Glendora, Calif) in the anterior segments. After extraction, the crown portion of the maxillary central incisor was prepared as a pontic and bonded with an ICE bracket to provide natural esthetics and space maintenance during active orthodontic treatment ( Fig 6 ). The archwire sequence in both arches was 0.016-in nickel-titanium, 0.016 × 0;0.022-in nickel-titanium, and 0.016 × 0;0.022-in stainless steel. Class II elastics were used to close the posterior extraction spaces and retract the maxillary anterior segment ( Fig 7 ). Lingual buttons were bonded on the mandibular right second molar and first premolar, and the mandibular left first premolar and second molar; lingual power chains were applied to help close the spaces ( Fig 8 ). Balancing buccal and lingual force can facilitate space closure and help prevent molar tipping and rotation. The mandibular left second premolar was mesially rotated about 80°, so it was necessary to rebond the bracket twice during treatment to correct the alignment ( Fig 9 ).


After 21 months of active treatment, all mandibular arch spaces were closed, but extraction spaces remained in the maxillary arch. Extra-alveolar miniscrews were placed in the mandibular buccal shelves to retract the entire dentition. Once a positive overjet was achieved, maxillary elastomeric chains were used to close the residual space by retracting the anterior segment ( Fig 10 ).
After 25 months of treatment, all spaces were closed except for the maxillary right central incisor implant site ( Fig 11 ). All fixed appliances were removed, and retention was accomplished with a maxillary clear overlay and a mandibular fixed retainer.




