In this article, we report the combined surgical and orthodontic treatment for a patient with bilateral craniofacial microsomia and facial asymmetry.
The patient, a 24-year-old woman, sought treatment with a chief complaint of facial asymmetry. Although she had undergone surgery to treat an external ear deformation at the age of 1 year, she had no history of surgery thereafter. She was diagnosed with bilateral craniofacial microsomia (mandibular bone retrusion, open bite, and facial asymmetry) and received a 2-stage operation at 2 times because of the marked retrusion of the mandible. The first operation was a LeFort I osteotomy and intraoral mandibular bone callus distraction, and the second was a bilateral sagittal split ramus osteotomy and chin reconstruction. The period of preoperative orthodontic treatment was approximately 24 months, and postoperative orthodontic treatment was performed for 24 months. A favorable occlusal relationship and an improved facial appearance were achieved.
Diagnosis and etiology
This patient consulted the Maxillofacial-Oral Surgery Department at Kanazawa Medical University Hospital in Japan with a chief complaint of facial asymmetry. Although she had undergone surgery for an external ear deformation at the age of 1 year, she had no other history of surgery thereafter, and no abnormality was noted on the medical examinations at school and in the workplace until she visited our department. Family members had no history of disorders. Facial photographs at the first examination ( Fig 1 ) showed that the frontal appearance was asymmetric, a right deviation of the mandible was marked, and the facial profile exhibited mandibular retrusion. Furthermore, although slight scars from the earlier surgery were noted in the bilateral external ears, no malformation was observed, and she had no functional abnormality such as a hearing disorder.

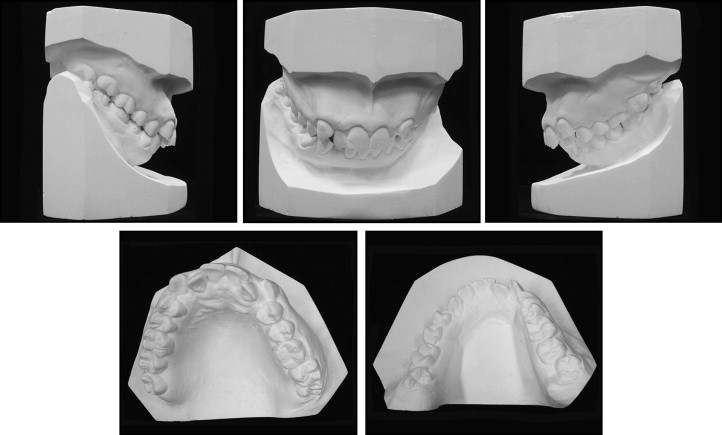
The intraoral photographs ( Fig 1 ) and a panoramic radiograph ( Fig 2 ) showed an anterior open bite and crowding. Overbite was −3 mm, and overjet was 7 mm. The molar relationship was Angle Class II on the left side and Angle Class I on the right. Furthermore, the bilateral third molars in the maxillary dentition had erupted, and the maxillary left canine showed labial displacement. All teeth in the mandibular dentition other than the left third molar had erupted, with no missing or malformed teeth. Both temporomandibular joints were deformed, especially the right joint as seen on the panoramic radiograph.

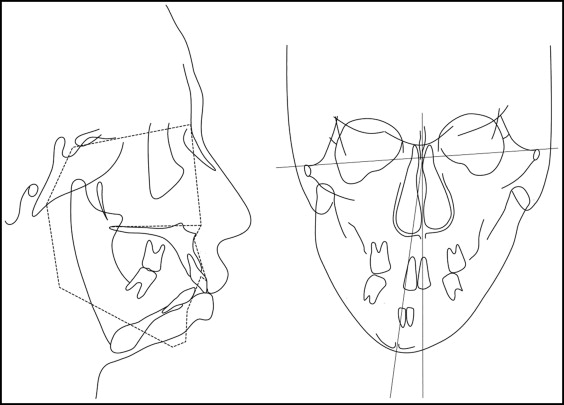
The pretreatment lateral cephalometric radiograph at the first examination ( Fig 3 ) showed that sella-nasion had a mean standard value, and the facial height (N-Me) was +1 standard deviation. Her upper facial height was +2 standard deviation. The position of the maxilla (SNA) showed a standard value, whereas the mandible was slightly rotated in a clockwise direction, and the mandible was located in a posterior position with hypoplastic growth. The frontal tracing showed hypoplastic growth of the right mandibular condyle. Menton in the mandible was deviated from the facial median by approximately 13 mm. Furthermore, the frontal view of the dental casts ( Fig 4 ) showed that the occlusal plane was inferiorly inclined on the right, and the difference in the distance between the interoccular plane and the occlusal plane on the maxillary right molar was approximately 5 mm.
The diagnosis was bilateral craniofacial microsomia with facial asymmetry, mandibular retrusion, and open bite.
Treatment alternatives
Surgical orthodontic treatment was planned to improve facial asymmetry, mandibular retrusion, and open bite. However, since the retrusion of the mandible was marked, with almost no mandibular angle, it was thought that sufficient anterior movement of the mandible could not be achieved with 1 surgery; therefore, a 2-stage operation at 2 times was selected. The first operation was LeFort I osteotomy and intraoral mandibular callus distraction to improve the deviation of the maxilla and the upper facial height, and to achieve anterior movement of the mandible. For the second operation after the mandibular distraction, bilateral sagittal split ramus osteotomy and chin reconstruction were planned. The maxillary and mandibular first premolars and right second molar were extracted. Although the mandibular right second molar had been devitalized and a crown had been placed, the condition of the infected root canal was poor. Therefore, it was extracted because of its poor prognosis, and the mandibular right third molar was moved mesially. Furthermore, both maxillary third molars were extracted.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


