This case report describes the treatment of a 16-year-old girl with a unilateral posterior buccal crossbite, a unilateral Class II molar relationship, and a maxillary right canine high in the labial sulcus. The treatment plan included surgically assisted unilateral maxillary expansion for the correction of the buccal crossbite, with simultaneous dentoalveolar distraction of the maxillary right canine into the extraction space of the first premolar aided by skeletal anchorage. Reduced orthodontic treatment time was facilitated by these 2 surgical procedures. A pleasing esthetic result and a good functional occlusion were achieved in 13 months.
Distraction osteogenesis is a bone-lengthening procedure that became popular after the extensive work by Ilizarov. It was first performed in the human mandible by Guerrero and McCarthy et al. Since then, it has been applied to various bones of the craniofacial region for correction of skeletal malformations.
First premolars are the most commonly extracted teeth for orthodontic purposes. Retraction of the canine into the extraction space is typically the second phase of orthodontic treatment, after the leveling and aligning phase. It has been reported that patients who undergo premolar extractions have prolonged treatment times.
With more adults opting for orthodontic treatment in the last decade, various attempts have been made to reduce the total treatment time and increase the efficiency of orthodontic treatment. To accomplish this, Liou and Huang proposed distraction of the periodontal ligament fibers during orthodontic tooth movement; this elicited rapid canine retraction in 3 weeks. According to the authors, the process of periodontal ligament distraction is similar to distraction osteogenesis in the midpalatal suture. The main drawback of the technique was that once canine retraction was completed, the new bone tissue distal to the lateral incisors was still too fibrous to retract the anterior teeth; thus, treatment progress was delayed by the consolidation and secondary mineralization process. To overcome this problem, Kisnisci et al and Iseri et al described the technique of dentoalveolar distraction in which osteotomies surrounding the canines are made to achieve rapid movement of the canines through the dentoalveolar segment, according to the principles of distraction osteogenesis.
Because of increased resistance of the midpalatal suture toward separation in a skeletally mature patient under an orthopedic load, surgically assisted rapid maxillary expansion has been recommended for correction of the maxillary transverse dimension ; it is now considered a form of distraction osteogenesis. Although posterior maxillary subapical osteotomy with immediate repositioning of the segment in the desired position has been proposed for transverse correction of isolated unilateral posterior crossbite, the stability of this procedure might be compromised. Using the principles of distraction osteogenesis, Swennen et al recently described how a posterior maxillary subapical osteotomy can be used to correct a unilateral posterior crossbite.
In this case report, we want to demonstrate how dentoalveolar distraction performed in 2 directions can simultaneously correct malocclusion in both planes of space and reduce the total treatment time for a patient in the late adolescence.
Diagnosis and etiology
A 16-year-old African American girl came to the orthodontic clinic at the University of Connecticut with a chief complaint of irregular teeth in the maxillary front region of the jaw. Her medical history was noncontributory, and the temporomandibular joint examination was normal with no mandibular shift.
The pretreatment facial examination showed an orthognathic soft-tissue profile ( Fig 1 ). The ratio of lower anterior facial height to upper anterior facial height and the ratio of lower facial height to throat depth were within normal limits. The nasolabial angle and the lip protrusion were within normal limits. The interlabial gap was 2 mm, and 100% of the occlusogingival length of the maxillary incisors was visible upon smiling. The maxillary and mandibular dental midlines were deviated to the right by 1 and 2 mm, respectively, from the facial midline.

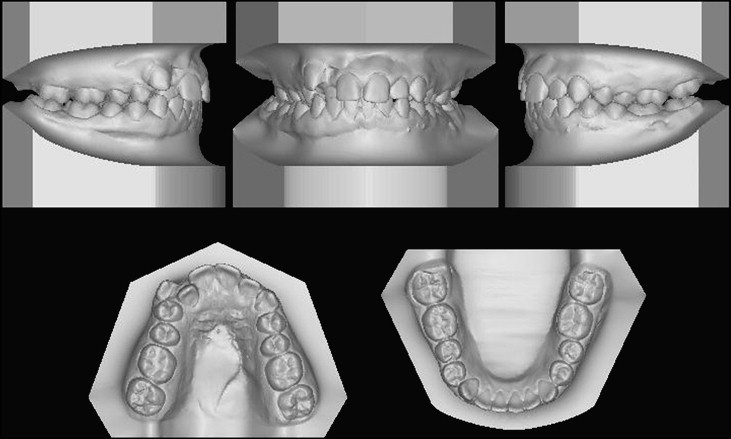
The intraoral examination showed that the patient had a full complement of teeth except for the third molars ( Figs 1 and 2 ). The molar relationships were Class I on the left side and full-cusp Class II on the right side. The maxillary right buccal segment and the lateral incisor was in complete lingual crossbite, and the maxillary canine on right side was highly placed in the labial sulcus. The mandibular dental arch was well aligned without crowding or spacing. The mandibular first molars had excessive labial crown inclinations. The patient had an overbite of 2 mm and an overjet of 3 mm ( Fig 3 ).
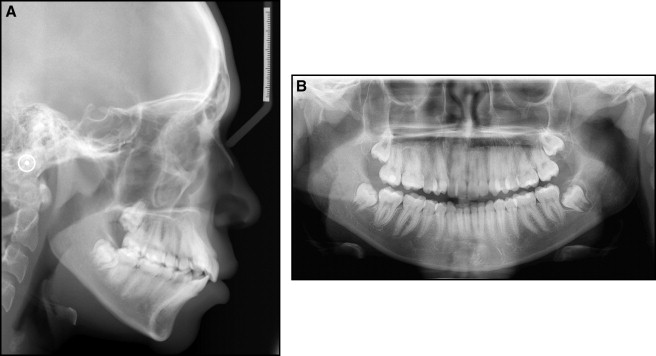
The cephalometric analysis showed a mild skeletal Class II relationship (ANB angle, 5°) with a slightly increased mandibular plane angle (SN-Go-Gn angle, 34°), and proclined maxillary incisors (U1-NA, 12 mm/28°) and mandibular incisors (L1-NB, 16 mm/40°) ( Table ).
| African American norm | Pretreatment | Posttreatment | |
|---|---|---|---|
| SNA (°) | 85 | 87 | 87 |
| SNB (°) | 81 | 82 | 82 |
| ANB (°) | 4 | 5 | 5 |
| Occlusal plane to SN (°) | 16 | 12 | 8 |
| Pg-NB (°) | 0 | 0 | 0 |
| MP-SN (°) | 33 | 34 | 35 |
| Maxillary incisor-NA (mm) | 8 | 12 | 12 |
| Maxillary incisor- NA (°) | 23 | 28 | 25 |
| Mandibular incisor-NB (mm) | 10 | 16 | 17 |
| Mandibular incisor-NB (°) | 33 | 40 | 42 |
| IMPA (°) | 101 | 104 | 106 |
| Interincisal angle (°) | 119 | 105 | 111 |
| Facial convexity G-Sn-Pg (°) | 13 | 10 | 10 |
| Upper lip protrusion Ls–Sn-Pg (mm) | 9 | 13 | 12 |
| Lower lip protrusion Li–Sn-Pg (mm) | 7 | 14 | 13 |
The patient was diagnosed with a skeletal and dental Class II subdivision right malocclusion with a slightly prognathic maxilla, moderate maxillary crowding, and a unilateral posterior crossbite on the right side.
Treatment alternatives
This patient’s malocclusion was in 2 planes of space, sagittal and transverse. The traditional approach would be to address the transverse dimension early in treatment with surgically assisted rapid palatal expansion, followed by extraction of the maxillary right first premolar to align the labially placed maxillary right canine. The total treatment time was expected to be about 20 to 24 months.
The second alternative was to simultaneously perform surgically assisted rapid palatal expansion and distraction of the labially placed maxillary right canine into the extraction space of the right first premolar, taking anchorage from a skeletal anchorage device.
The third alternative would entail 4 premolar extractions to reduce the incisor inclinations in conjunction with the first or the second option. This option would also require distalization of the maxillary right buccal segment (aided by skeletal anchorage) to move the incisors lingually without affecting the maxillary midline.
The patient chose the second option over the conventional approach, since the total treatment time was estimated to be 12 to 15 months.
Treatment progress and surgical plan
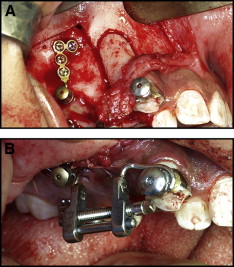
After the initial appointment for the records, the patient was referred to the Division of Oral Surgery at the University of Connecticut for placement of a skeletal anchorage plate. A miniplate (Stryker, Kalamazoo, Mich) was placed below the key ridge area on the right maxilla under local anesthesia. It was positioned so that the attachment head would be at the same level as the crown of the highly placed maxillary right canine. Impressions were taken to fabricate a custom distraction appliance for the canine retraction.
Two weeks later, the patient was scheduled for the osteotomy for canine distraction and unilateral surgically assisted rapid palatal expansion. The operation was performed under general anesthesia with nasal endotracheal intubation after local infiltration with a vasoconstrictor (lidocaine 2% with 1:100,000 epinephrine) at the height of the maxillary vestibule. A horizontal soft tissue incision was made 3 to 4 mm apical to the attached gingivae from the midline to the first molar on the right side. The mucoperiosteum was carefully reflected with a periosteal elevator, exposing unilaterally the nasal floor and the lateral aspect of the maxilla between the canine root and the infraorbital nerve. Posteriorly, the periosteum was undermined up to the pterygomaxillary junction.
For the canine distraction, the surgical bone cuts were done with a piezotome, under copious external saline-solution irrigation. Cortical cuts were made on the mesial and distal aspects of the canine root starting at the midroot region and continuing apically 3 mm from the apex. Cortical bone cuts were advanced in the coronal direction with narrow osteotomes. The first premolar was extracted at this stage. Osteotomes of appropriate sizes were then used from the mesial aspect of the dentoalveolar segment that included the canine to split the surrounding trabecular bone around its root from the palatal cortex and neighboring teeth. The transport dentoalveolar segment included the buccal cortex and the underlying trabecular bone-enveloped canine root while leaving an intact palatal cortical plate ( Fig 4 , A ).