Fig. 19.1.
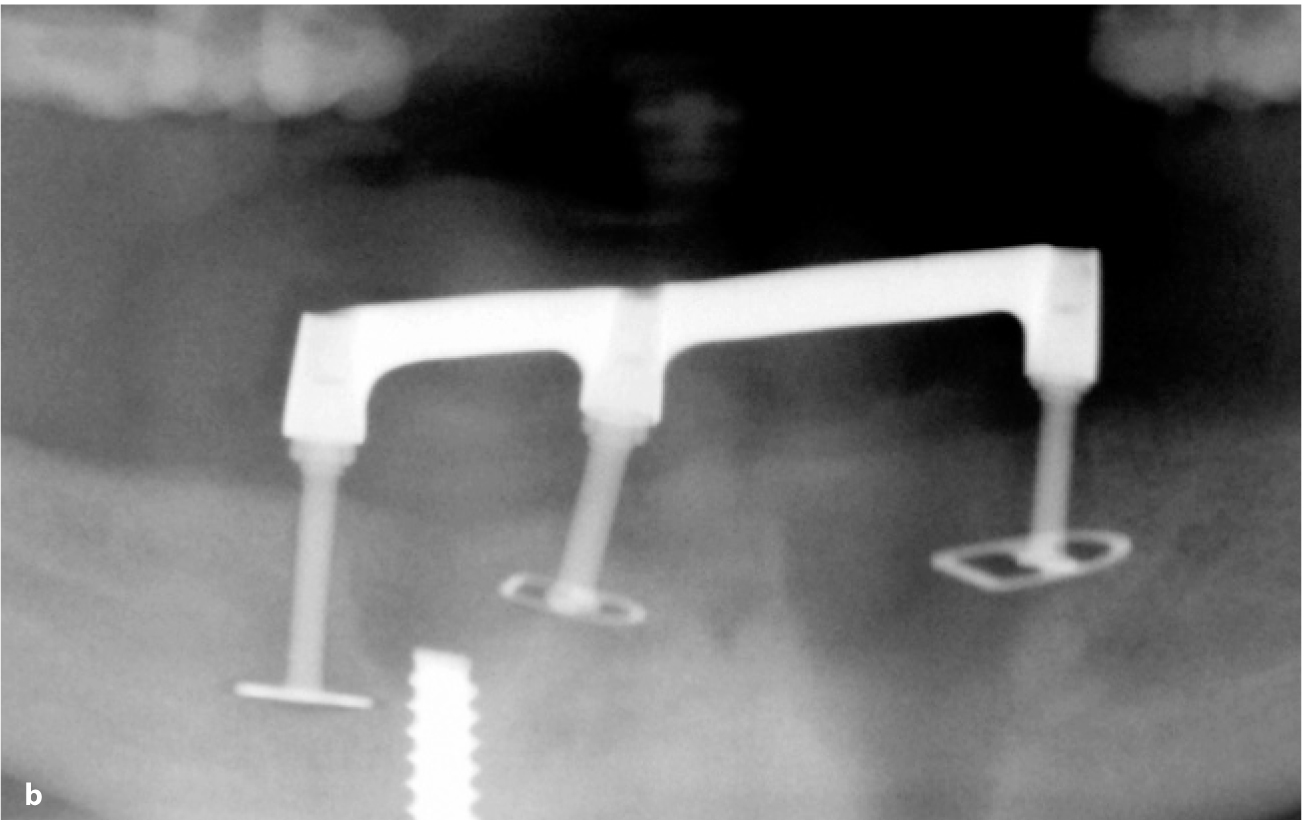
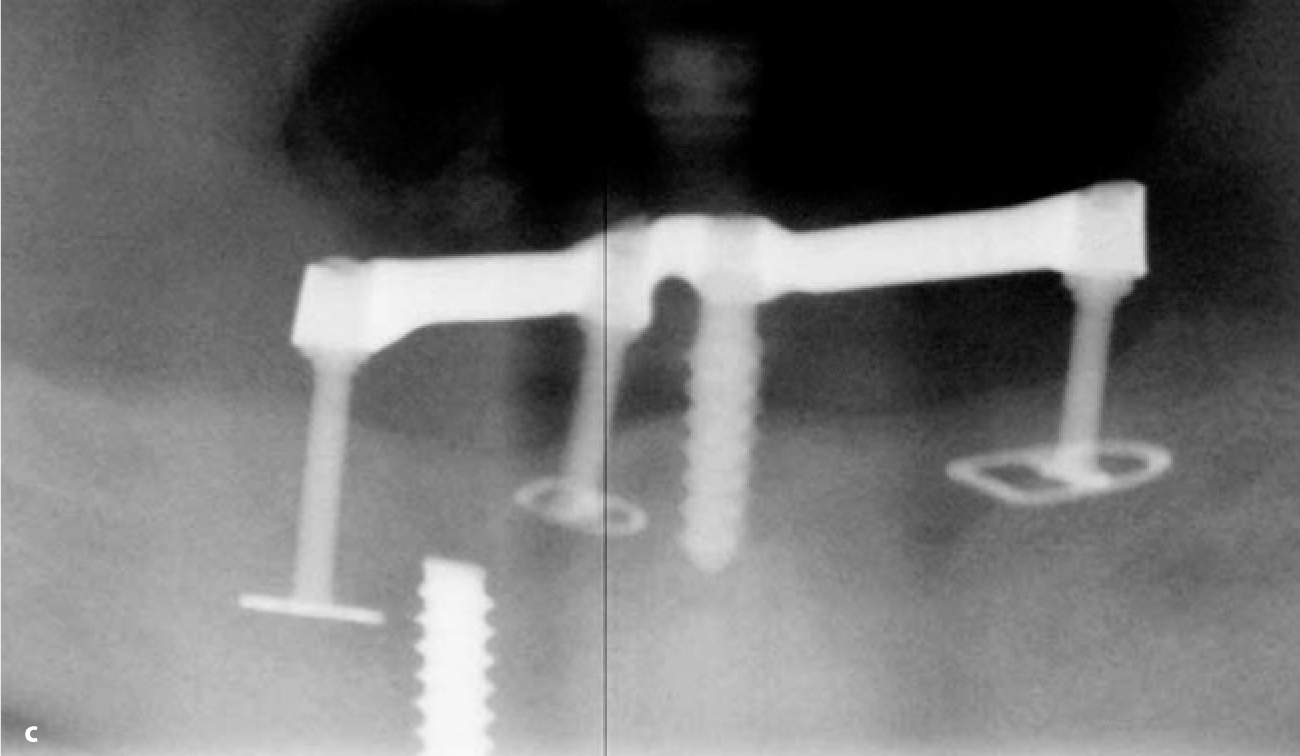
a Preoperative radiograph. b After the granulation tissue and all non-integrated implant segments had been removed, extremely large craters remained in the mandible. Nevertheless, three BOI implants could be inserted right away. Primary stability was immediately achieved. c After the defects had healed, a screw implant was inserted. Bone resorption in the anterior segment was likely to occur as a function of mandibular remodelling in accordance with the new functional orientation and the healing potential of the residual bone. The threaded part of the screw implant is somewhat exposed for this reason. Peri-implantitis is not the cause for this exposure, since the bone structure harbouring the implant is convex in crestal direction, whereas bone loss associated with peri-implantitis would be characterized by a tray-like concave collapse (see also Chapter 9.2). With BOI implants, it does not matter whether and to what extent the threaded pin is vertically anchored “inside the bone”


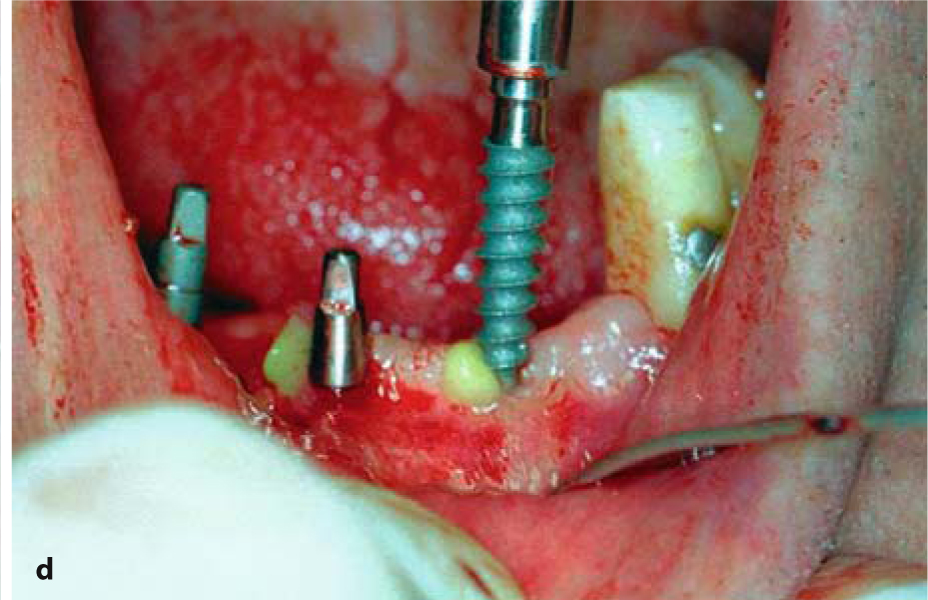
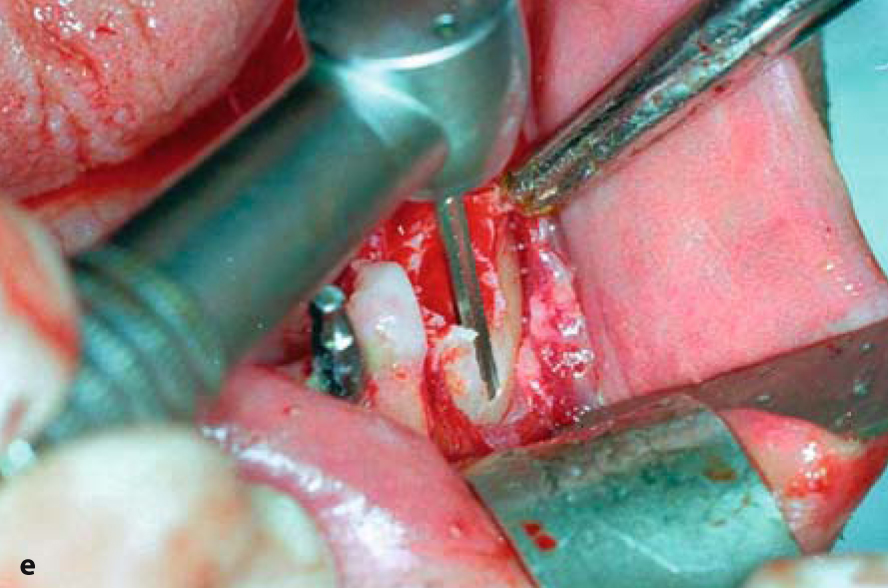
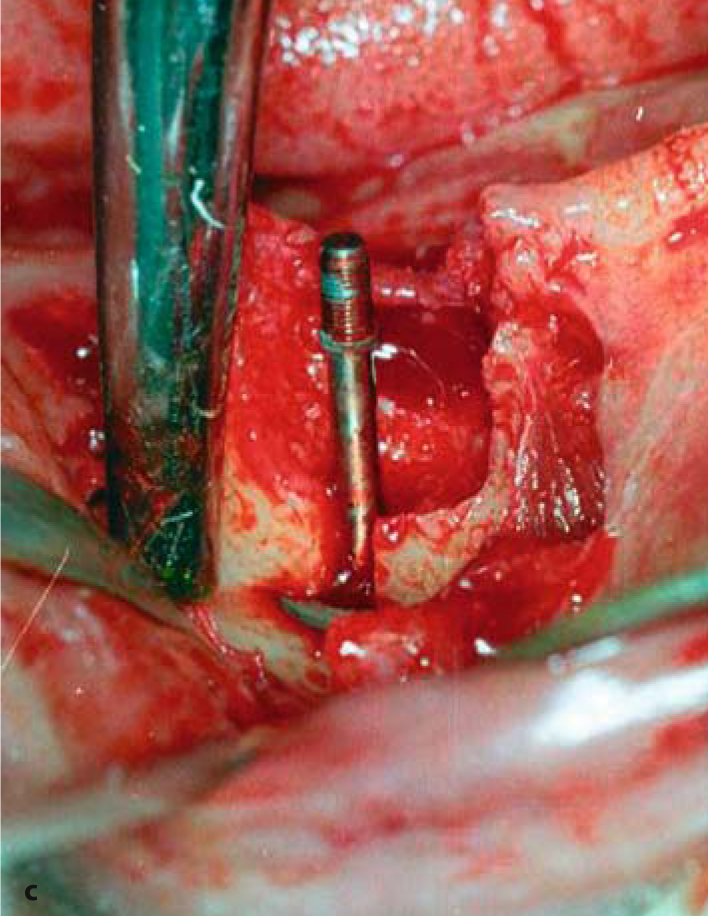
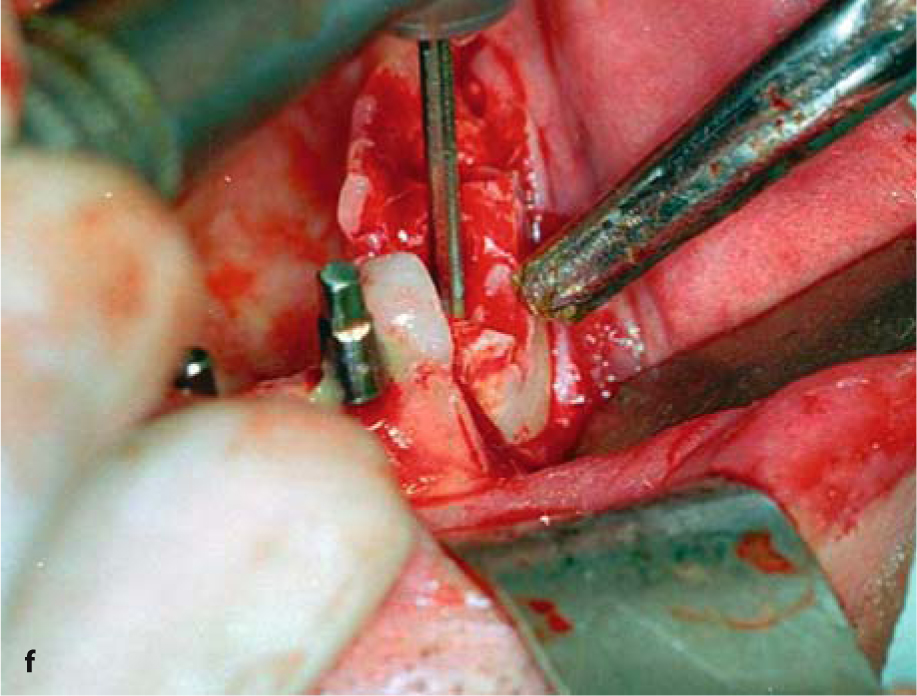
Fig. 19.2.
a Residual dentition in the anterior mandible. Both canines and the first premolar on the left were highly mobile. b The situation was due to a removable clasp denture that had been worn without enossal support in the distal area. c Following extraction of tooth 43, which left an impressively large bone defect, an ED 7 G8 implant was bicortically inserted in the basal mandibular segment. A double- or triple-disk BOI implant, inserted into the distomedial bone walls, would have been an option as well. The use of BOI implants in this situation is strictly confined to designs featuring a smooth surface of the threaded pin. d Crestal implants can be inserted in the anterior segment. In this specific case, we used compression screws of the KOS type, which were inserted in a transgingival approach. e
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


